 [Description exercise 2]
[Description exercise 2]
Findings: Squamocolumnar junction is elevated from the diaphragmatic orfice more than 2cm. At far distal esophagus, 4 wide and linear mucosal breaks covered with white exudate were found. They were confluent. In the mid-esophagus, linear mucosal breaks are also seen.
Impression: (1) Sliding hiatal hernia, (2) Reflux esophagitis, LA-D
[comment]
GERD is a clinical dignosis. Endoscopic diagnosis is reflux esophagitis.
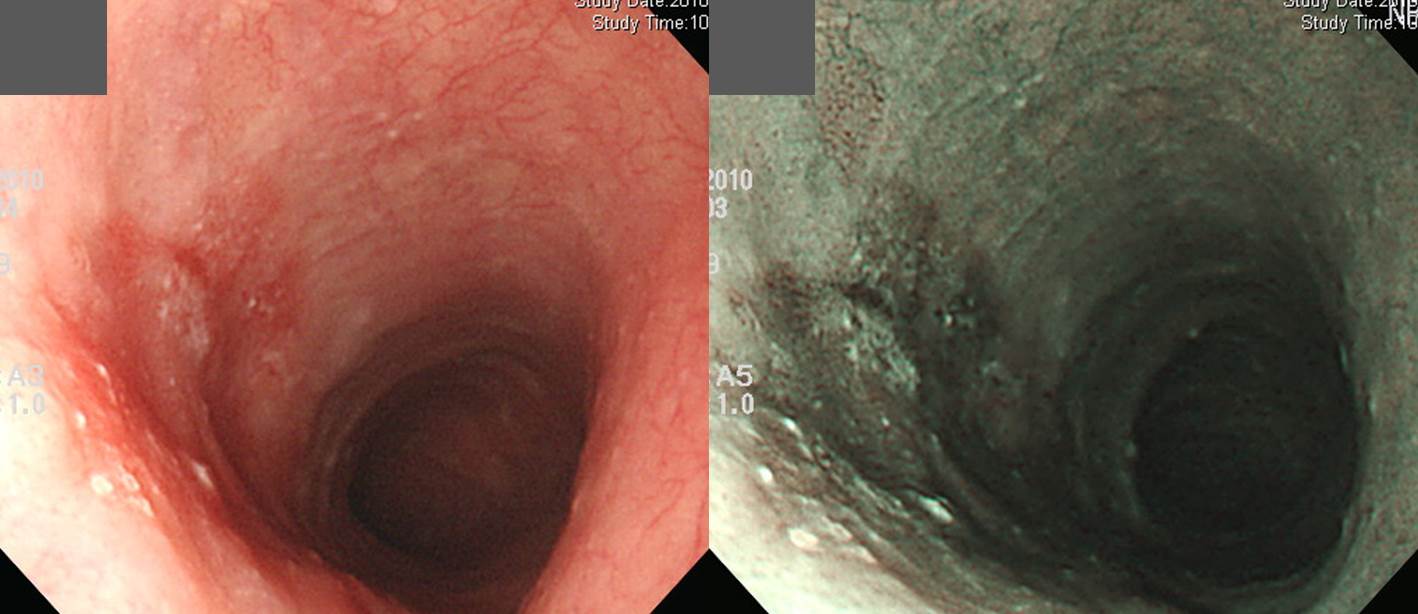 left: white light endoscopy picture, right: NBI (narrow band imaging) picture
left: white light endoscopy picture, right: NBI (narrow band imaging) picture
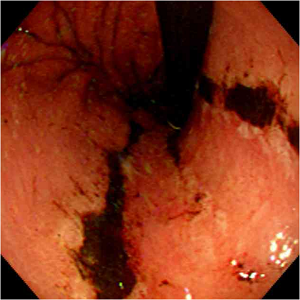
Findings: At mid-esophagus, 2 cm-sized slightly depressed hyperemic area was seen. Edge is slightly irregular and surface is uneven in some areas.
Impression: Superficial esophageal cancer, IIb (or IIc)
[Comment]
Endoscopic findings of superficial esophageal cancer 1) Faint hyperemia
2) Change of microvasculature
3) Eroded/ulcerated
4) Mucosal thickening
5) Coarsening of the mucosa
6) Multiple white mucosal plaquesSurgery was done and final pathology was as follows.
Invasive squamous cell carcinoma, moderately differentiated:
1) tumor size: 2.5x1.5 cm
2) extension to submucosa
3) endolymphatic tumor emboli: not identified
4) perineural invasion: not identified
5) negative resection margins (proximal, 3 cm ; distal, 15 cm)
6) metastasis to one out of 22 regional lymph nodes
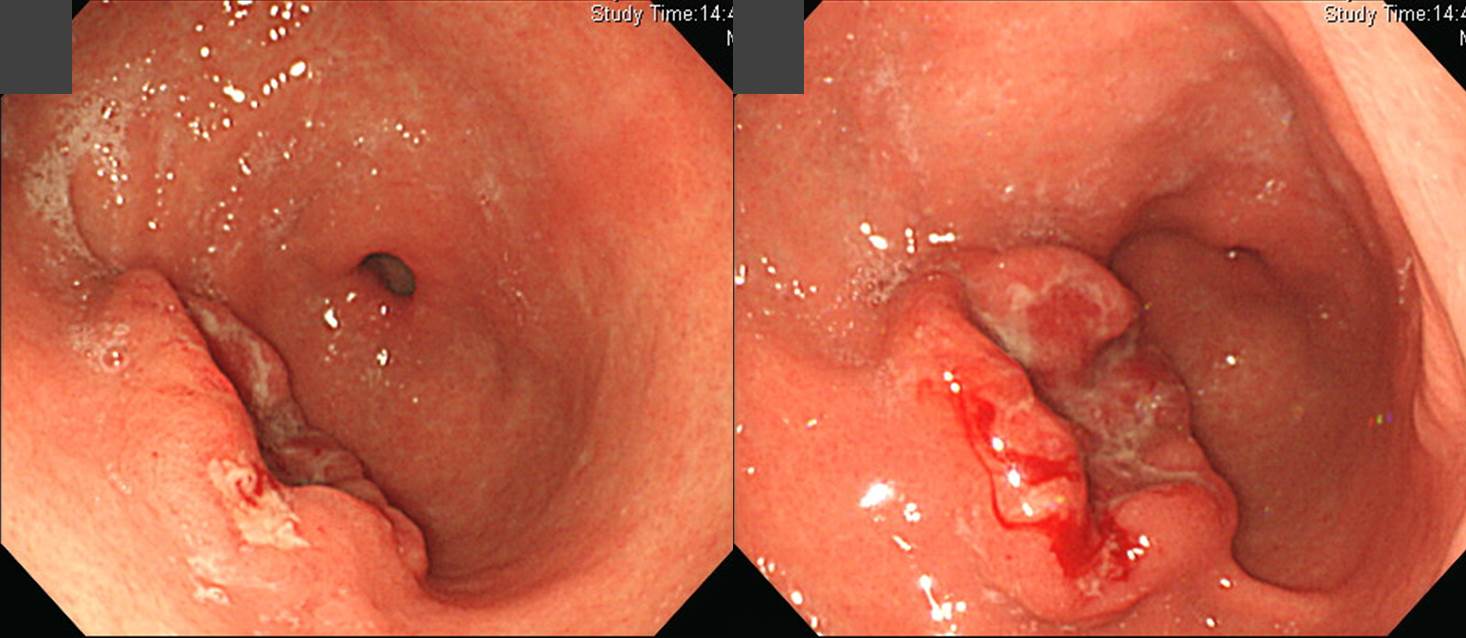
Findings: At antrum, there are multiple variable sized deep and shallow ulcers and erosions. Some of them were convered with dirty exudate and hematin.
Impression: AGML (acute gastric mucosal lesion)
[Comment]
Characteristics of AGML and some more examples
- Focal, acutely developing gastric mucosal defects
- Caused by NSAIDs or severe stress
- Usually less than 1cm, circular, small, multiple
- Located mainly in the stomach and occasionally in the duodenum
- Range in depth from superficial epithelium (erosion) to deeper lesions (ulceration)
- Are not precursors of chronic peptic ulcers
- Unlike peptic ulcer, found anywhere in the stomach, gastric rugal pattern is essentially normal, and the margins and base of ulcer are not indurated, no thickening and scarring of blood vessels



Impression: Multiple benign gastric ulcers, A2 (r/o CMV gastritis, r/o NSAID induced gastritis)
[Comment]
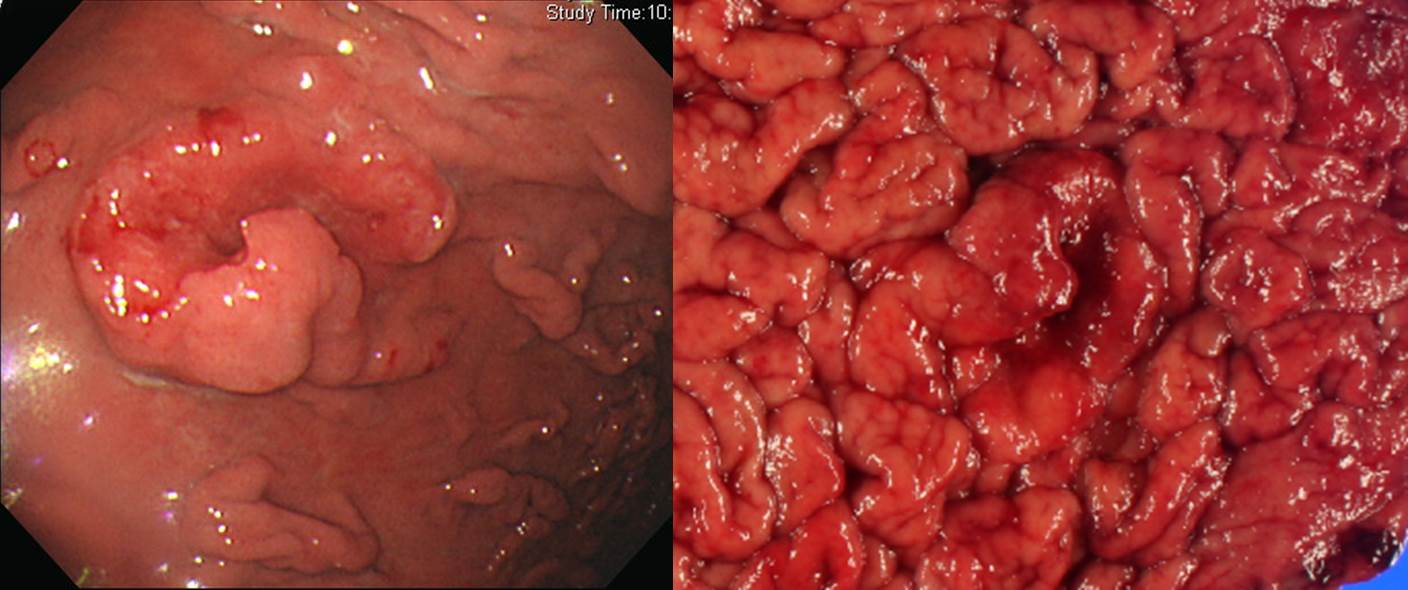
Impression: Early gastric cancer, IIa
[Comment]
ESD was done and the final pathology was as follows.
Stomach, endoscopic submucosal dissection:
. Early gastric carcinoma
1. Location : antrum, lesser curvature
2. Gross type : EGC type IIa+IIb
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size : 2.8x2.3 cm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin: free from carcinoma (safety margin: distal 0.8 cm, proximal 0.8 cm, anterior 0.4 cm, posterior 0.8 cm)
8. Lymphatic invasion : not identified
9. Venous invasion : not identified
10. Perineural invasion : not identified
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
Impression: AGC, type I
[Comment]
Surgery was done. Actually it was EGC with deep SM invasion. The histology was uncommon type.
Stomach, subtotal gastrectomy:
Early gastric carcinoma
1. Location : lower third, Center at antrum and lesser curvature
2. Gross type : EGC type I
3. Histologic type : gastric carcinoma with lymphoid stroma (medullary carcinoma)
4. Histologic type by Lauren : intestinal
5. Size : 3x2.3 cm
6. Depth of invasion : invades submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 17 cm, distal 4.5 cm
8. Lymph node metastasis : no metastasis in 41 regional lymph nodes (pN0), (perinodal extension: absent)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: T1b N0
Wang HH, Wu MS, Shun CT, Wang HP, Lin CC, Lin JT. Lymphoepithelioma-like carcinoma of the stomach: a subset of gastric carcinoma with distinct clinicopathological features and high prevalence of Epstein-Barr virus infection. Hepatogastroenterology. 1999;46(26):1214-9.
METHODOLOGY: Of 379 patients with gastric adenocarcinoma, from 1993 to 1996, 6 of them with lymphoepithelioma-like carcinoma of stomach were retrospectively studied.
RESULTS: Five patients were females and one patient was male. Their age ranged from 51-75 years with a mean age of 61.5 years. Endoscopically, 2 patients were initially diagnosed as early gastric cancer and the other 4 were diagnosed as advanced gastric cancer. Three patients had tumors located in the lower third of the stomach, while the other three tumors were located in the middle and upper third. Two tumors invaded into the serosal layer and the other four lesions were confined at submucosal and muscular layers. Using the in situ hybridization method, all 6 patients (100%) had positive nuclear Epstein-Barr virus-encoded small RNA signals in the tumor cells but not in the surrounding lymphoid stroma and non-neoplastic gastric mucosa. Helicobacter pylori was found in 4 (66.7%) of the cases. The mean follow-up period of the 6 patients was 27 months. Five patients were free of the disease. Lymph node involvement and mesenteric implantation was noted in one patient in which cancer recurred 1 year after gastrectomy.
CONCLUSIONS: Lymphoepithelioma-like carcinoma of stomach in this study revealed a female predominance, preferential localization in the proximal part of the stomach, better prognosis, and a high association with Epstein-Barr virus infection.
Followings are similar cases.
Early gastric carcinoma
1. Location : lower third, center at antrum and greater curvature
2. Gross type : EGC type IIc+IIa
3. Histologic type : lymphoepithelioma-like carcinoma (EBV-positive)
4. Histologic type by Lauren : intestinal
5. Size : 2.5x2x0.5 cm
6. Depth of invasion : extension to submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal, 10.0 cm; distal, 1.8 cm
8. Lymph node metastasis : metastasis to 2 out of 36 regional lymph nodes (pN1)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
Advanced gastric carcinoma
1. Location : upper third, Center at high body and greater curvature
2. Gross type : Borrmann type 2
3. Histologic type : lymphoepithelioma-like carcinoma
4. Histologic type by Lauren : diffuse
5. Size : 4.4x3.2x1.4 cm
6. Depth of invasion : extension to proper muscle (pT2a)
7. Resection margin: free from carcinoma, safety margin: proximal, 5.5 cm; distal, 21 cm
8. Lymph node metastasis : no metastasis in 67 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10.Venous invasion : not identified
11.Perineural invasion : not identified

1. Location : upper third, center at cardia (Siewert III)
2. Gross type : Borrmann type 2
3. Histologic type : Medullary carcinoma (lymphoepithelioma-like carcinoma)
4. Histologic type by Lauren : indeterminate
5. Size : 2.2x2.2 cm
6. Depth of invasion : invades muscularis propria
7. Resection margin: free from carcinoma, safety margin: proximal 1.4 cm, distal 2 cm
8. Lymph node metastasis : no metastasis in 52 regional lymph nodes
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
Findings: Duodenal bulb was deformed due to multiple converging folds. There was no active ulcer crater.
Impression: Duodenal ulcer scar, S2
[Comment]
2019-7.
8. Wide mucosal breaks are converging, so the classification is C or D. Don't forget the hiatal hernia is the underlying cause of this patient's reflux esophagitis. It needs to be mentioned in the impression.
9. The observation is good. You can add the classification such as IIb.
10. At first, it is a diffuse lesion and not likely to be a malignant condition. In addition, clinical information of acute abdominal pain suggests that it is some kind of a acute infectious or inflammatory condition. Ulcers, erosions, hematins, and dirty exudate are mixed. The diagnosis is AGML (acute gastric mucosal lesion), which is a kind of severe gastritis.
11. Yes. Multiple ulcers caused by medications (NSAIDs).
12. IIa would be better, because it is SLIGHTLY elevated lesion.
14. It may be difficult for the beginners. It is duodenal ulcer scar.2017-12-17. A beginner's answer
2024-10-5. An answer from a visiting doctor and my response.
© EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.