 [Risk of lidocaine spray]
[Risk of lidocaine spray]
Previous | Home | EndoTODAY | List | Next
Lidocaine spray 후 중증 methemoglobinemia가 가능합니다. 증례보고 중 다음 문장이 저의 가슴을 아프게 하였습니다. 의사들이 lidocaine spray의 위험성을 몰라서 환자를 위험에 빠지게 할 수 있다는 이야기였기 때문입니다.
It is not generally appreciated that therapeutic doses of most local anesthetics (given topically or intravenously) can produce this condition.
Discussion 부분을 일부 옮깁니다. 꼭 그리고 천천히 읽어보시기 바랍니다.
일단 pulse oxymeter는 methemoglobinemia에서는 소용이 없다는 부분입니다.
The definitive diagnostic test for methemoglobinemia is multiple-wavelength co-oximetry. Co-oximeters measure the light absorption of blood at numerous ultraviolet wavelengths. As a result, these machines are able to determine the percentages of oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin and methemoglobin. A multiple-wavelength co-oximeter is different from a pulse oximeter, which measures ultraviolet absorption at only two wavelengths (940 and 660 nm) to differentiate oxyhemoglobin and deoxyhemoglobin. Pulse oximeters are designed for continuous noninvasive monitoring, whereas co-oximeters require a blood sample and are typically available only at tertiary care centres.
A standard blood gas machine will not detect methemoglobin. Such machines measure oxygen tension (PO2 ) and pH, then calculate oxygen saturation from these values. This approach assumes the absence of abnormal hemoglobin. To complicate matters, pulse oximeters are unreliable in the presence of methemoglobin, because methemoglobin is detected by both the oxyhemoglobin (940 nm) and deoxyhemoglobin (660 nm) sensors of the oximeters. At low levels (<20%), methemoglobin is detected primarily by the deoxyhemoglobin sensor, and a pulse oximeter may show a falsely low oxygen saturation. At high methemoglobin levels (>70%), detection by the oxyhemoglobin sensor predominates, and a pulse oximeter may show a falsely high reading.
환자가 가슴이 답답하고 cyanosis가 온 상황에서 pulse oxymeter로 측정한 산소포화도가 이상이 없으면 바로 methemoglobinemia를 의심해야 합니다.
Clinical findings include cyanosis that is unresponsive to oxygen and cyanosis in the presence of normal (calculated) oxygen saturation. Although pulse oximeter readings are inaccurate in this circumstance, oximeter saturation values that deviate substantially from the clinical picture may suggest the diagnosis. In addition, if the difference between the calculated oxygen saturation from a standard blood gas machine and the reading from a pulse oximeter is greater than 5%, it is likely that the patient has an abnormal hemoglobin (either carboxyhemoglobin, methemoglobin or sulfhemoglobin; cyanohemoglobin does not result in this finding). Some authors refer to this as a "saturation gap," whereas others use this term for the difference between the calculated oxygen saturation from a standard blood gas machine and the measured value from a co-oximeter.
치료는 methylene blue이지만 이보다 앞서 close monitoring과 응급조치가 100배 더 중요합니다. 환자를 평가하고 methemoglobinemia를 의심하고 진단하고 methylene blue를 투여하기 전까지 환자의 vital을 잘 유지해야 하기 때문입니다. 내시경 전처치, 시술, 시술 후 과정에서의 close monitoring이 무엇보다 중요합니다.
Symptomatic patients with methemoglobinemia, particularly those with levels over 20%, should receive methylene blue, which acts as a cofactor for the enzyme NADPH methemoglobin reductase. Electrons are transferred from NADPH to methylene blue, which leads to a reduction of the heme iron, in the form of deoxyhemoglobin.... To reduce delays in administration, our ED has added to ward stock sufficient methylene blue for an initial 2 mg/kg dose.
 55세 남자환자가 외부병원에서 위암으로 진단받고 소화기내과 외래를 방문하였습니다. 환자는 복통이나 체중감소가 없다고 하였습니다. 간단한 신체검진을 한 후 외래에서 내시경재검, 위 CT, Upper GI series, 혈액검사 등을 시행한 후 외과의뢰를 하기로 결정하였습니다.
55세 남자환자가 외부병원에서 위암으로 진단받고 소화기내과 외래를 방문하였습니다. 환자는 복통이나 체중감소가 없다고 하였습니다. 간단한 신체검진을 한 후 외래에서 내시경재검, 위 CT, Upper GI series, 혈액검사 등을 시행한 후 외과의뢰를 하기로 결정하였습니다.
외래가 끝날 무렵 저의 EMR (electronic medical recording) 화면에 CVR (critical value report)가 떴습니다. 조금 전 진료하였던 그 환자의 hemoglobin이 6.8 g/dl이라는 것이었습니다. 급히 환자를 외래로 모셔서 다시 문진을 해 보니 환자는 weakness, dizziness, dyspnea on exertion을 고민하고 계셨습니다. 수혈을 하고 입원하여 검사하는 것으로 계획을 변경하였습니다. 역시 위암은 급만성 출혈을 일으킬 수 있습니다.
진행성 위암은 단순히 수술하는 병으로 생각하고 문진을 소홀히 하기 쉽습니다. 그러나 본 환자에서와 같이 자세한 문진을 누락하면 환자는 상당기간 고생을 하실 수도 있는 일입니다. 내과의사의 기본인 history taking과 physical examination의 중요성을 절감하였습니다.
 [2013-9-3. 애독자 질문] 좋은 교육자료와 제 질문에 항상 답변해주시는 점에 대해 감사드립니다. 최근 methemoglobulinemia에 대한 내용도 잘 보았습니다. 실제적인 의문이 있어 문의드립니다. Methemoglobulinemia의 치료로 antidote인 methylene blue를 투여한다고 하는데, 실제로 methylene blue가 ample로 나오는게 있습니까? 수술시 methylene blue를 종종 쓰곤 하는데, IV로 투여하는 용도는 아닌 것으로 알고 있습니다. 첨부하신 논문에서도 methylene blue를 가져오는데 20분 걸렸다는 내용이 있었습니다.
[2013-9-3. 애독자 질문] 좋은 교육자료와 제 질문에 항상 답변해주시는 점에 대해 감사드립니다. 최근 methemoglobulinemia에 대한 내용도 잘 보았습니다. 실제적인 의문이 있어 문의드립니다. Methemoglobulinemia의 치료로 antidote인 methylene blue를 투여한다고 하는데, 실제로 methylene blue가 ample로 나오는게 있습니까? 수술시 methylene blue를 종종 쓰곤 하는데, IV로 투여하는 용도는 아닌 것으로 알고 있습니다. 첨부하신 논문에서도 methylene blue를 가져오는데 20분 걸렸다는 내용이 있었습니다.
[2013-9-4. 이준행 답변] 과거에는 약제부에서 methylene bule 원료를 구하여 원내제제 형태로 공급해 주었습니다. 저도 아주 드물게 내시경 진단용으로 사용한 경험이 있습니다. 안 쓴지 10년도 넘지만.....
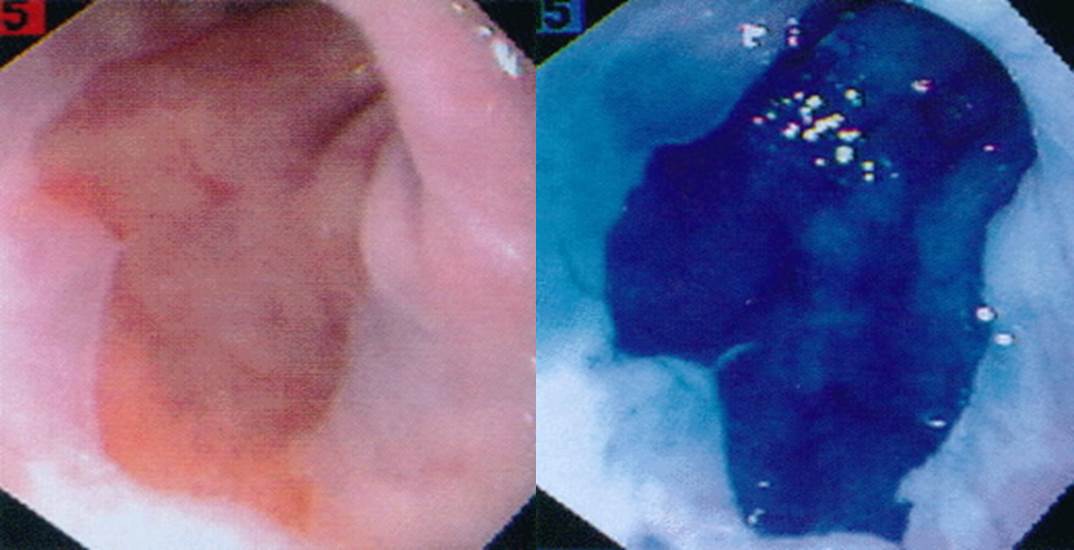
인터넷에서 가져온 사진. Barrett esophagus에서 methylene blue를 사용하면 이렇게 uptake가 된다고 합니다. 실제로 해 보면 이렇게 강하게 염색되지는 않지만...
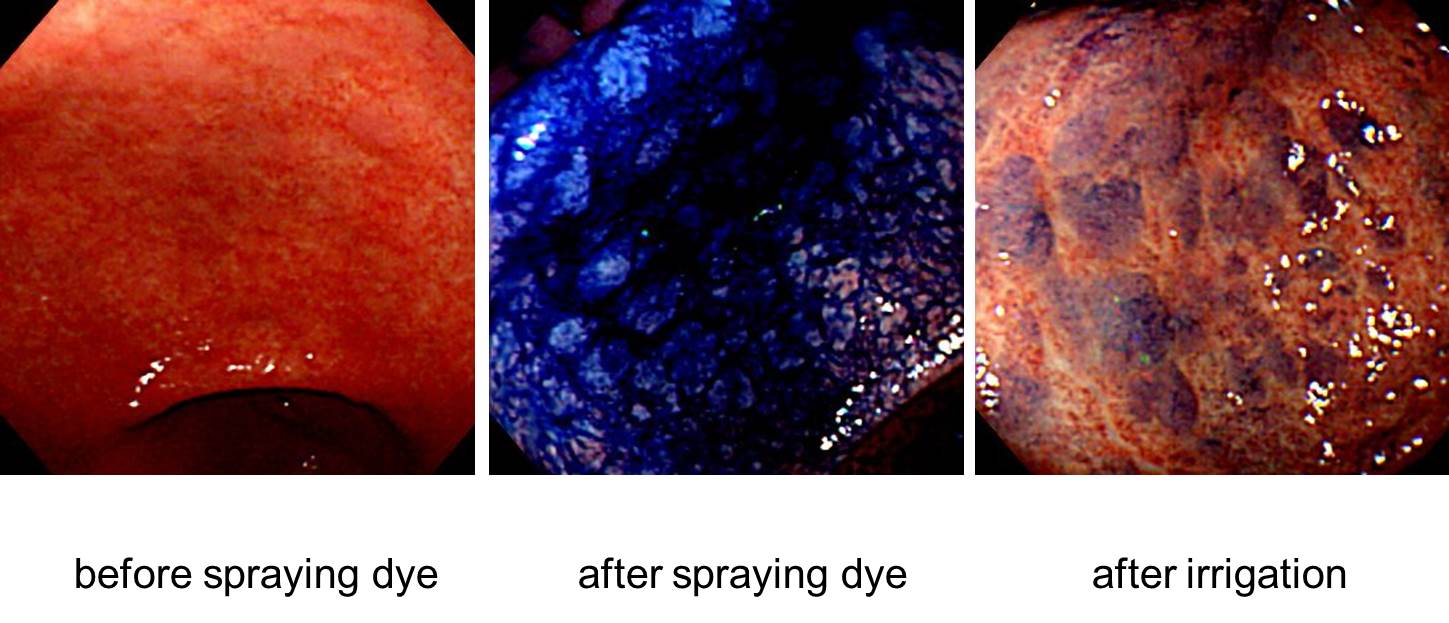
Metaplastic gastritis에서 methylene blue를 사용하여 사진을 찍었습니다. 맨눈으로도 잘 보이는 것을 염색해보면 더 잘 보입니다. 결국 임상적 의의가 없다는 뜻입니다. 한 10년 전에 이 사진을 마지막으로 더 이상 methylene blue를 사용하지 않고 있습니다.
최근에는 내시경실에서 더 이상 methylene blue를 사용하지 않고 있기 때문에 비치하지도 않습니다. 정맥주사용 methylene blue는 비치하려고 해도 불가능합니다. 구할 수 없기 때문입니다. 수년 전까지 삼오제약에서 수입을 하였습니다. 약제부에서도 소량 가지고 있었습니다 (관련 link). 당시 약전에 언급된 효능, 용법, 용량은 다음과 같았습니다.
포장단위: 10 mL 앰플. 효능: 약물에 의한 메트헤모글로빈 혈증, 용법/용량: 메칠렌블루로서 체중 kg당 1~2mg(0.1~0.2mL)을 수분에 걸쳐 매우 천천히 정맥주사한다.
현재는 수입이 중단된 상태입니다. 사용량이 적기 때문인 것 같습니다. 제가 알기로는 현재 국내에서 구입할 수 없습니다. 희귀의약품센터에 문의하는 수 밖에 없는 것 같습니다. 응급 약제를 국내에서 정상 루트로 구할 수 없다니 한심한 일입니다. 비치하고 있는 병원도 거의 없지 않나 싶습니다. 환자가 발생하면 열심히 supportive care하고 저절로 돌아올 때까지 기다릴 수 밖에 없습니다. 한심합니다. 보건복지부는 환자생명과 직결된 필수약 공급이 적절한지부터 살피는 것이 도리 아닐까요? 행정에 녹아있는 인명경시풍토가 한탄스럽습니다.
현재 상황에서 최선의 대책은 무엇인지 개인적으로 좀 더 알아보겠습니다.
[2013-9-4. 추가] Methylene blue 1% 주사 공급에 관해 희귀의약품 센터에 문의한 결과를 전해들었습니다. 황당하기 그지 없습니다.
1) 센터 보유 재고는 없고, 필요시 신청하면 도입까지 2~3주 소요된다고 합니다.
2) 자가치료용이므로, 일반약품처럼 병원에서 발주내서 재고보유하고 있다가 필요시 사용할 수 없고 환자 발생시 환자가 진단서 등 필요서류를 작성하여 희귀의약품센터에 신청하는 경우에만 도입/사용 가능하다고 합니다.
3) 미국에서 수입
4) 공급 요청 case는 매우 드물며, 최근 희귀의약품센터에서 공급해준 경우는 2012. 9월 요청된 경우가 마지막이라 합니다.