 [Percutaneous endoscopic gastrostomy (PEG)]
[Percutaneous endoscopic gastrostomy (PEG)]
EndoTODAY | EndoATLAS | Outpatient Clinic
Parasite | Esophagus | Stomach | Cancer | ESD
Home | Guide | Author | Search | Blog | Links
 [Percutaneous endoscopic gastrostomy (PEG)]
[Percutaneous endoscopic gastrostomy (PEG)]
1. 일시적 혹은 영구적인 연하곤란으로 경구 식이가 불가능한 경우로서 통상 장기간 비위관을 통한 enteral feeding에 의존하는 환자에서 시행한다.
2. 대부분 CVA나 Parkinsonism 등 신경과 환자나 이비인후과 영역의 악성종양을 가진 환자가 대상이 된다. 상기 환자에서 전혀 oral feeding이 되지 않거나 oral feeding이 가능하더라도 흡인성 폐렴이 반복되는 경우에 PEG를 시행하는 경우가 많다.
3. Aspirin, clopidogrel 등 항혈소판제는 보통 3-4일 끊고 시행한다. 시술 다음 날 다시 시작하는 것이 좋다. 와파린도 끊어야 하지만 와파린을 끊는 기간은 담당과과 상의하여 결정한다.
4. PEG는 단지 위로 영양분을 직접 넣어주는 것에 지나지 않기 때문에 기질적 혹은 기능적 폐쇄가 있는 경우는 대상이 되지 않는다. 통상 비위관을 통한 영양공급에 문제가 없는 환자에서 장기간의 enteral feeding을 하고자 할 때 PEG를 시행하는 것이다.
5. PEG는 장기간의 enteral feeding을 도와주는 방법으로 응급시술이 아니다. 환자의 상태가 unstable한 경우에는 절대로 시행하지 않는다.
6. PEG 삽입은 구강을 통하여 튜브가 삽입되기 때문에 aseptic한 시술이 아니다. 따라서 국소 감염증이 자주 발생할 수 밖에 없다. 국소 감염증은 대부분 1일 1-2회 정도의 드레싱과 IV 항생제로 호전되지만, 드물게 튜브를 제거해야 하는 경우도 있다. 이외의 합병증으로는 leak, 출혈, 위식도역류, pneumoperitoneum 등이 가능하다. 합병증 발생시에는 우선 시술의와 상의하여 튜브 및 external anchor의 위치를 확인하는 것이 좋다. 조금 조여주거나 풀어주어서 문제가 해결되는 경우가 많기 때문이다.
7. PEG 삽입을 위하여 시술 전 예방적 항생제를 투여한다 (가장 최근 systemic review)
8. 참고: European guideline은 아래 그림을 click하세요.
9. 참고: Cleveland Clinic의 PEG 환자 설명서
10. 참고: ASGE의 PEG 환자 설명서
12. 참고: YouTUBE 환자 설명 동영상
| 분류 | 기본처방 | 약처방 | 검사처방 |
| Day 1 (입원) | V/S q 8h BR TD --> MNNPO Body weight check Height check Get permission (시술동의서와 수면내시경동의서) |
XDNK2 IV 20gtt | Chest X-ray, 표준 혈액검사 |
| Day 2 (procedure day) | V/S q 8h BR NPO Send to endoscopy room |
XDNK2 IV 20gtt Cefazolin 1g IV (1회 on call) |
. |
| Day 3 | V/S q 8h BR NPO for 24hr after PEG --> 이후 feeding start (아래 참조) Daily dressing |
XDNK2 IV 20gtt | . |
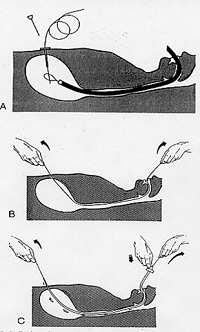
Pull technique을 이용한 표준 삽입법
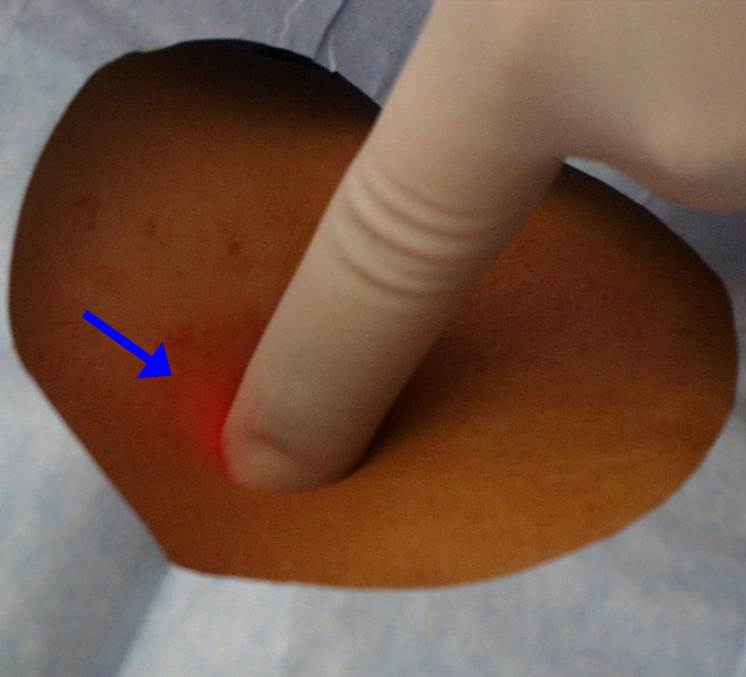
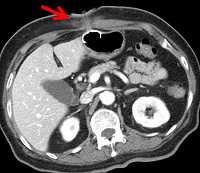
Punture 이전에 transillumination을 확인해야 한다.
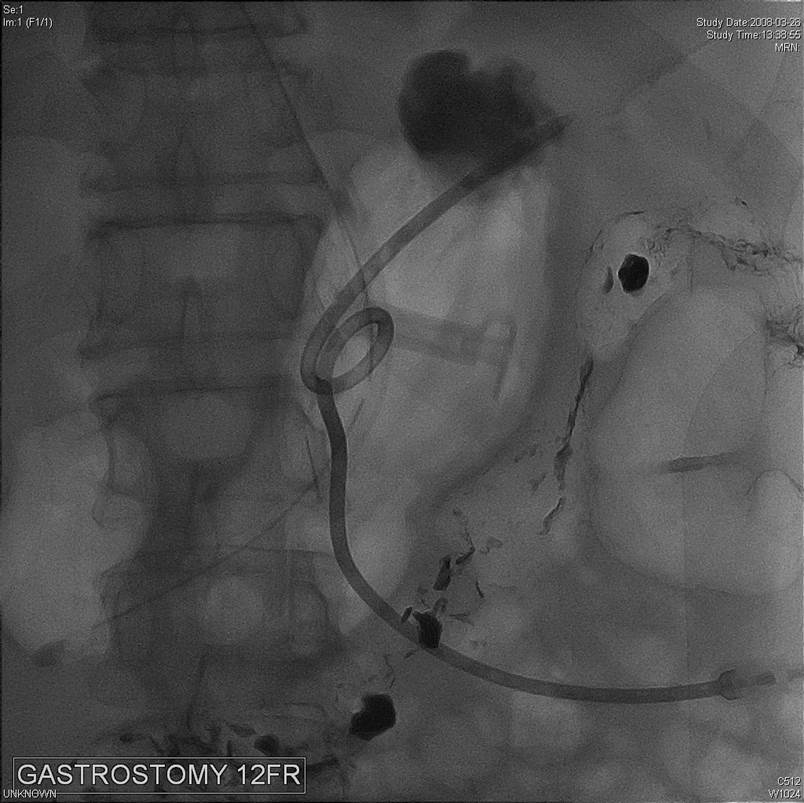
내시경을 삽입할 수 없는 환자에서는 PEG를 할 수 없으므로
, 영상의학과에 의뢰하여 PRG를 해야 한다.
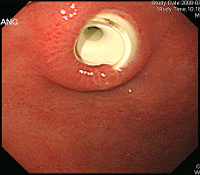
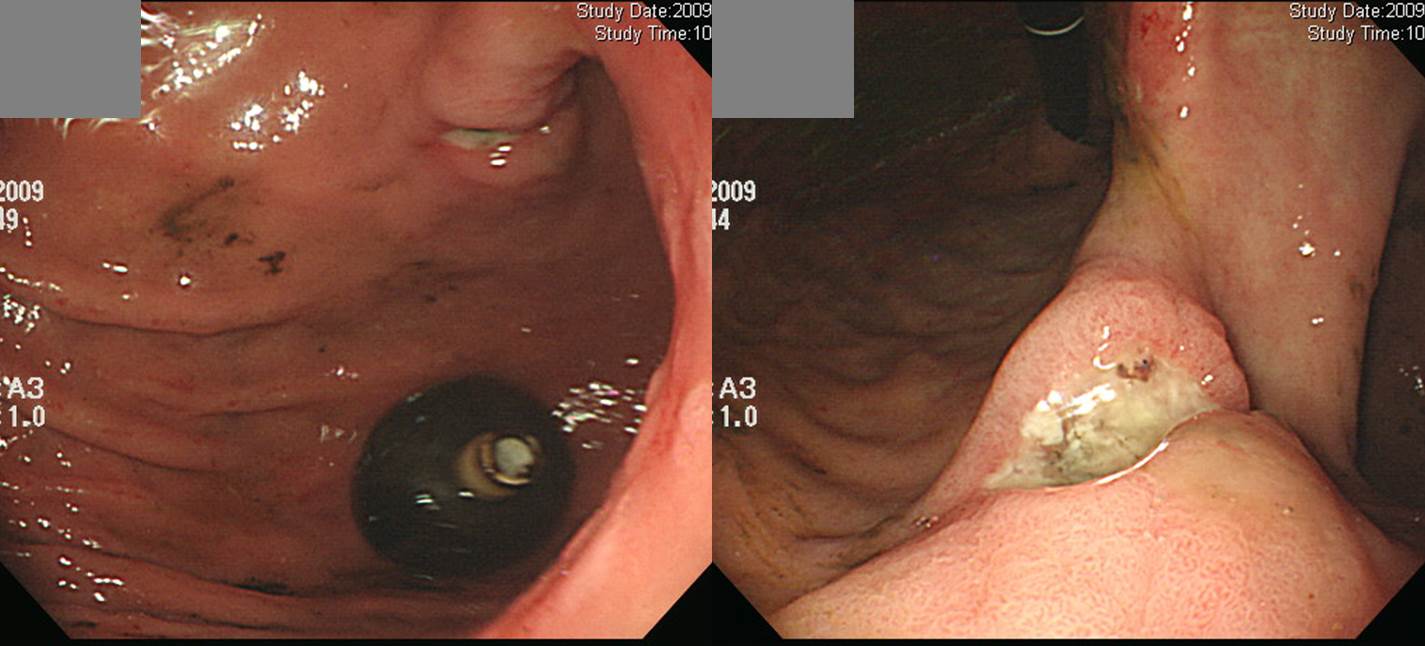
진행성 식도암으로 esophageal obstruction과 tracheo-esophageal fistula가 있어서 covered stent를 넣은 환자입니다. Stent 시술 후에도 지속적인 aspiration이 있어서 경구 식이섭취가 어렵다고 판단되어 PEG 삽입이 의뢰되었습니다. Stent로 인하여 식도가 충분히 넓어지지 않았다면 PEG tube가 식도를 통과하지 못할 가능성이 있는 상황이었습니다. 그러나 다행스럽게도 9.2 mm 외경의 내시경이 저항없이 식도를 통과할 수 있어서 통상적인 방법으로 PEG 시술이 가능하였습니다.
식도 stent에 dirty white한 exudate가 있었고 이 부위를 tube가 통과되었기 때문에 PEG tube의 contamination 정도는 통상보다 높을 수 밖에 없다고 판단되어 최대한 소독을 하였고 1-2일 정도의 IV 항생제 사용을 권하였습니다.
복부팽만이 없고, 장음이 들리면 feeding을 아래와 같은 순서로 시작한다.
1. N/S 50 ml per 1hr (3 times)
2. SFD feeding if aspiration (-) after 4hr
3. SFD 50 ml - water 50 ml to prevent tube obstruction
4. Increase SFD 50 ml every 4hr up to 250 ml
5. SFD every 3hr after 250 ml
6. SFD every 2hr
PEG의 가장 흔하고 중요한 합병증은 wound infection입니다. 제가 fellow이던 시절 이에 관한 짧은 논문을 쓴 적이 있어 소개합니다. 당뇨환자에서는 wound infection이 더욱 많다는 내용이었습니다.
Increased risk of peristomal wound infection after percutaneous endoscopic gastrostomy in patients with diabetes mellitus Dig Liver Dis 2002;34:857-61
Wound infection
Severe wound infection - necrotizing fasciitis

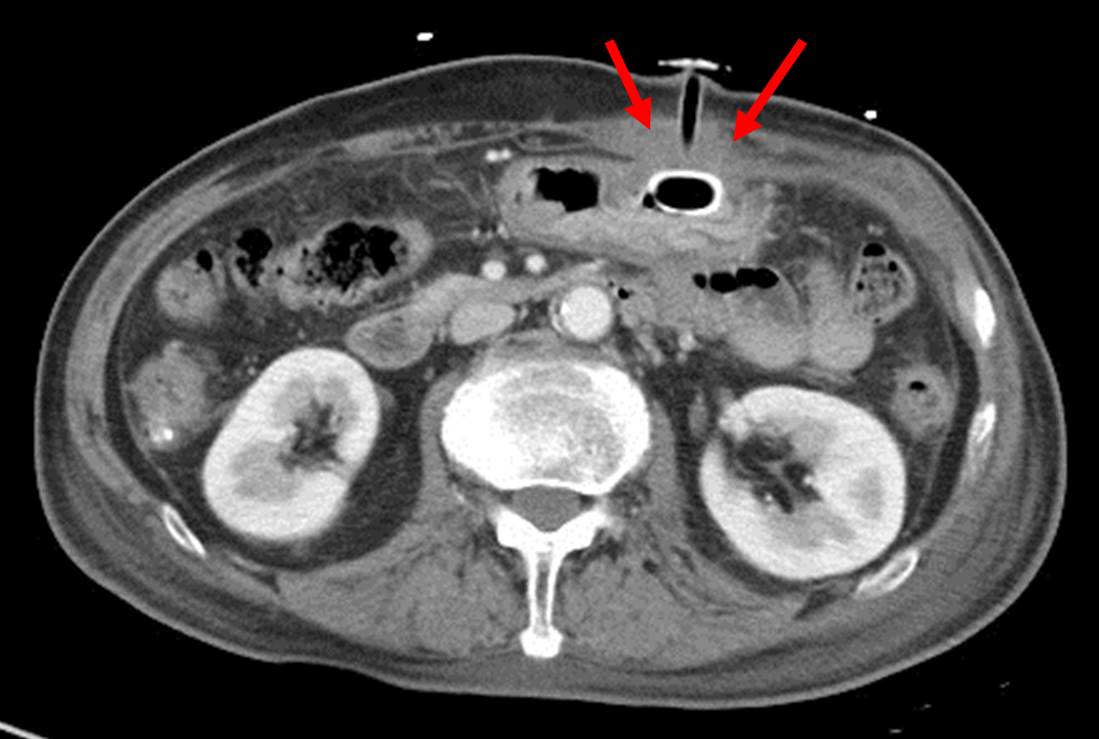
Pneumoperitoneum
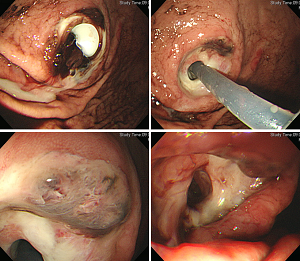
Buried bumper syndrome (partial)
Pressure necrosis
정식 PEG tube가 아닌 Foley catheter를 삽입한 후 내원한 환자에서 발견된 pressure necrosis
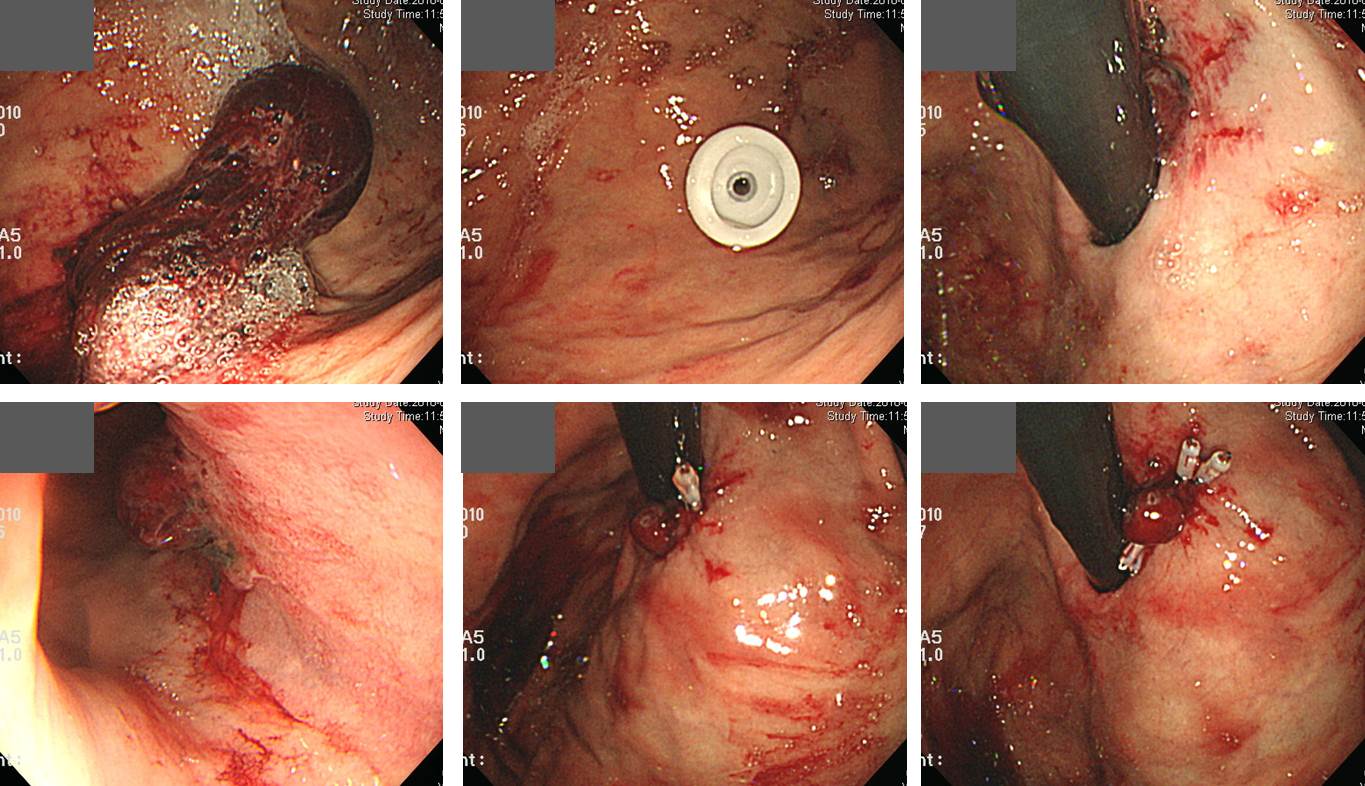
PEG 3일 후 발생한 Mallory Weiss tear
1) PEG 튜브를 삽입하게 된 이유가 소멸된 경우 PEG tube를 제거한다.
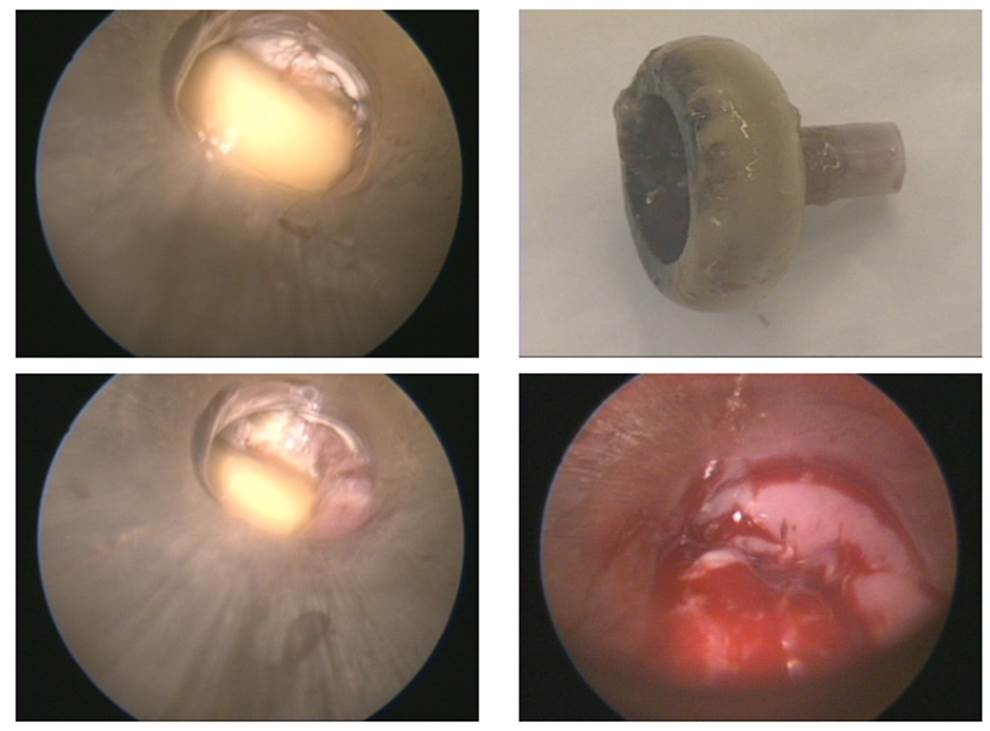
2) PEG 튜브를 제거하는 방법은 두 가지가 있다. (1) Blind한 방법으로 PEG 튜브를 몸 밖에서 당겨서 제거하는 방법, (2) 내시경을 위내에 삽입한 상태에서 몸 밖에서 튜브를 자르고 internal bumper는 내시경을 통하여 수거하는 방법. PEG 튜브를 제거 후 남아있는 fistula opening은 2일 정도 금식하면 대부분 저절로 막힌다. 막히지 않는 경우 histoacryl을 사용할 수 있다.
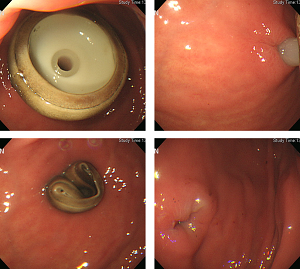 몸 밖에서 PEG 튜브를 당겨서 제거하는 방법
몸 밖에서 PEG 튜브를 당겨서 제거하는 방법
 튜브 제거 직후의 fistula. 대부분 하루 내에 완전히 막힌다.
튜브 제거 직후의 fistula. 대부분 하루 내에 완전히 막힌다.
3) PEG의 교체는 위의 방법에 따라 튜브를 제거한 후 그 자리에서 즉시 fistula tract을 통하여 교체용 튜브를 삽입한다. 그러나 용이하지 않은 경우에는 튜브 제거 수일 후에 약간 옆 부분에 PEG 튜브를 새로 삽입한다.
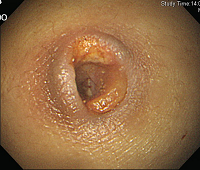
 8. 절단한 PEG tube bumper가 상부식도에 걸린 경우 2예
8. 절단한 PEG tube bumper가 상부식도에 걸린 경우 2예
PEG tube가 필요없게 되면 그냥 힘으로 잡아당기면 빠집니다. 간혹 PEG tract의 손상을 우려하여 internal bumper 2-3cm 상단의 tube를 가위로 절단하여 내시경으로 제거하기도 합니다. 그 과정에서 상부식도에 걸릴 수 있습니다. 한 분은 midazolam 투여 후 제거할 수 있었고 한 분은 이비인후과에 의뢰하여 rigid esophagoscope로 제거하였습니다.
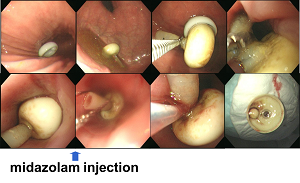
내시경 삽입하에 PEG 튜브를 제거하다 internal bumper가 식도에 걸려 midazolam 투여 후 제거가 가능하였던 경우
이비인후과에 의뢰하여 rigid esophagoscope로 제거한 경우
PEG tube를 뽑으면 tract는 저절로 막힙니다. 그런데 특이하게도 저절로 믹히지 않은 환자가 있어서 조직접합제로 치료한 예가 있었습니다.

위체하부전벽에 PEG가 관찰되며 바로 옆에 약 1mm 크기의 hole이 관찰됨. Injection catheter를 이용하여 histoacryl 0.5ml와 lipiodol 0.5mL를 섞여서 누공 관에 주입함. 시술도중 특별하 합병증이 없는 것을 확인하고 검사 종료
 10. Balloon-type replacement tube 사용설명서와 현실적인 적용
10. Balloon-type replacement tube 사용설명서와 현실적인 적용
 풍선형 교체 튜브
풍선형 교체 튜브
뱃줄(PEG 튜브)을 처음 삽입할 때에는 버섯형 튜브를 쓰지만 변경할 때에는 풍선형을 사용하고 있다. 회사측 사용설명서에는 아래와 같이 씌여져 있다.
Check balloon volume every 7 to 10 days for correct inflation volume using the following steps;
- Discontinue feeding
- Use a luer-tip syringe to completerly evacuate water from balloon
- Discard evacuated water
- Reinflate balloon with appropriate amount of water (20 ml).
For optimal performance, the tube should be replaced every 30 days or as required to ensure balloon patency and unoccluded tube lumen.
[Balloon-type replacement tube 환자 및 보호자에 대한 설명]
풍선형 교환튜브는 처음 삽입한 버섯형 튜브에 비하여 빠질 위험이 높습니다. 회사측 사용 설명서에는 7-10일마다 주사기를 이용하여 이용하여 풍선의 물을 빼고 새 물을 20 ml 넣어주도록 되어 있습니다 (증류수와 주사기는 의료기상에서 개별 구입). 회사측 사용설명서에서는 튜브를 30일 간격으로 교환하도록 권하고 있습니다.
사실 한달마다 튜브를 바꾸는 것은 쉬운 일이 아닙니다. 따라서 교체하지 않고 그냥 사용하다가 막히거나 변색되었을 때 바꾸는 경우가 많습니다. 단 정해진 교환주기보다 오래 사용하는 경우 풍선의 누수로 인하여 튜브가 빠질 위험이 높다는 점은 알고 계셔야 합니다. 만약 튜브가 빠지면 그 즉시 튜브를 다시 밀어 넣고 응급실로 오시기 바랍니다. 수분 이상 지체되면 과거에 만들었던 구멍을 사용할 수 없습니다.
회사의 추천과 현실적인 측면을 고려하여 2주에 한번 물을 바꾸고 3달에 한번 튜브 교체를 추천합니다. 간혹 물을 바꾸지 않고 그냥 쓰시는 분이 계시는데 옳은 방법은 아닙니다.
 11. Non-balloon type replacement tube
11. Non-balloon type replacement tube
수년 전 갑자기 non-balloon type replacement tube가 수입중단되어 balloon형을 사용하고 있었습니다. 2012년 말 우리나라의 한 회사에서 non-balloon type replacement tube를 생산하기 시작하였다고 합니다. 저는 아직 써 본 적은 없습니다.
긴 tube가 없는 button type이라는 것도 있는데 저는 한번도 써 본 적이 없습니다.
[2014-6-28. 애독자 질문] 저는 부산의 종합병원에서 일하고 있는 소화기내과 의사입니다. 병원에서 PEG 시술을 하고 PEG tube를 교체해 주고 있습니다. 잘 사용하다가 tube 옆으로 식이가 새는 경우가 있습니다. 심한 분들은 계속 새어 나와서 경우에 따라 더 큰 직경의 tube로 교체해 주고 있습니다. 제가 알아 본 봐에 의하면 가장 큰 직경의 tube가 24Fr 인데 이것을 하고 있는 분이 새면 어떻게 해 주어야 할지 모르겠습니다. 좋은 방법이 없을까 하여 문의 드립니다.
[2014-6-29. 이준행 답변] 저는 이 부분에 경험이 별로 없어 여러 교수님들께 의견을 여쭈었습니다. 아래 답변들을 참고하시기 바랍니다.
[답변 1] PEG site leak가 있는 경우는 PEG의 외경이 두꺼운 것으로 교체하는 것보다는 기존 PEG를 제거하고 closure를 시킨뒤 새로 PEG stomy를 만들어야 한다고 배웠던 것 같습니다. 교체와 새로 만드는 것을 비교한 RCT를 본 적은 없습니다. PEG leak가 한번 생기면 어떻게 해도 호전이 없어서 결국 기존 PEG를 제거하고 새로운 자리에 PEG를 만든 적이 서너번 있습니다.
[답변 2] PEG leakage의 경우 회사에 알아보면, 24Fr 보다 큰 것이 있습니다. 저도 이전에 24 Fr에서 28, 30 Fr까지 교환해 본 적이 있습니다. 큰 것으로 바꾸는 것을 기다리는 동안 며칠 NPO 하다 보면, PEG site가 좁아져서 오히려 더 작은 것으로 삽입할 수도 있습니다. 2-3일 내에 바로 막히지는 않고, 많이 좁아집니다. 금식하고 매일 dressing하면서 PEG site를 관찰하는 것이 좋습니다. 3일 정도 지나면 막힐 수도 있습니다.
[답변 3] PEG leakage가 있는 경우 원래보다 작은 관을 넣어야 직경이 줄어들면서 leak가 좋아집니다. 큰 튜브를 넣으면 점점 커집니다. 작은 tube로 넣으면 주변이 새기때문에 금식을 시키고 항생제를 사용하면서 상처가 좋아지기 기다립니다. 대부분 감염이 되면서 상처가 나빠지기 때문입니다. 맞는 것이 없어 저는 Foley tube를 사용하면서 했어고 지지할 수 없어서 튜브 끝에 saline bag을 달아 약간 당겨지게 하였었습니다. 관건은 작은 튜브를 넣고 금식하여 상처주변에 지저분한 분비물이나 음식물 위액이 덜 나오도록 하면서 상처가 나아야 구멍이 작아집니다.
[답변 4] Leakage가 있다고 구경이 큰 것으로 교체하면 더 넓어져 오히려 악화될 수 있어 추천하지 않습니다. 자주 dressing하고 gauze를 갈아주어 말리는 것이 최선의 방법이라고 생각합니다. 그래도 안되면 제거하고 다른 곳에 새로 해볼 수 있으나 반복될 가능성이 높습니다.
[답변 5] 이론적으로 복압을 낮추는 것이 도움이 됩니다. 허리를 느슨하게 하는 옷을 입게 하고 가스차는 음식을 좀 줄이고 식사양을 조절하여 너무 빠르게 투여되지 않게 하는 것들이 필요할 것 같습니다.
[답변 6] 특별히 염증이 있거나한 문제가 없다면 저 같은 경우 새로 튜브를 교체해보고도 음식이 새어나오면 4시간 정도 제거를 했다가 재삽입을 합니다. 두 번 밖에 해보지 않았지만 모두 이후 leakage가 없었습니다. 제거 시간은 튜브와 누공의 이격에 따라 조금 조절해보면 되지 않을까 생각합니다. 두 번 다 balloon type 으로 넣었습니다 (이전에도 balloon type 으로 가지고 있었던 분들이었습니다). 느슨해졌던 것이 조금 촘촘해진 정도의 느낌이었고 다행히 큰 무리없이 들어갔습니다. 만약 너무 좁아져서 안들어가면 dome-type tube로 넣어야 하겠고.. 그래서 시간이 중요할 것 같습니다. 저도 4시간 기다리면서 약간 걱정은 되었었지만 대부분 괜찮지 않을까 생각됩니다. "4시간은 완전히 저의 단순 결정이었습니다." 그리고 효과가 모자라다 싶으면 ballloon type 이니 부담없이 6시간 빼보고 다시 넣는 등으로 하면 되지 않을까 생각됩니다.
[답변 7] PEG 시술 후 겪게 되는 가장 곤란한 경우중의 하나가 peristomal leakage인 것 같습니다. 이론적으로는 percutaneous gastrostomy가 형성된 상태이므로 leakage가 있다고 문제가 될 것은 없지만 여간 불편한 것이 아니며, 일부 환자들은 시술이 잘못된 것으로 오해하기도 하는 것 같습니다. 특별한 예방 방법이 없이 시술 당시에 신경을 써서 절개가 튜브 직경에 비해 너무 크게 되지 않도록 약간 꼬옥 끼이는 느낌으로 시술하고 있습니다. 처음에 약간 끼이는 느낌이 있어도 시간이 지나면 야간 느슨해지는 경험을 많이 했기 때문입니다. 특히, 처음 절개가 크지 않더라도 시술 초기에 tract maturation이 되기 전에 tube가 많이 움직이거나 (환자가 기침을 하는 경우 등) 피부의 탄력과 피하지방이 적어서 적절하게 완충시켜주지 못하는 환자들에서 많이 발생하는 것 같습니다. 일단 발생하면 좀더 큰 직경의 tube로 교체해 본다거나, tract 주위 염증과 피부 진물이 아물때까지 dry up 시킨 후 다시 tube를 재투여해 보고, 그래도 leakage가 호전되지 않는다면 다른 위치에 다시 tract을 만들고 새로운 tube를 삽입하는 방법을 사용하고 있습니다. 정답이 없는 문제인 것 같아 개인적인 경험을 몇 자 적어봤습니다.
[답변 8] 대개 PEG 는 2차 병원에서 많이 하게 되지요. 제 경험으로는
1. 기존의 PEG tube 제거하고, dressing 만 하면서 previous site 가 거의 아물때까지 기다립니다. 이때 foley catheter 등 다른 이물질로 기존의 site를 유지하려고 노력하실 필요가 없습니다. 이물질이 있는 한 피부 병변은 healing 되기 어려운 것 같습니다.
2. 이때 tube site cultre 를 하고, 항생제를 사용하기도 합니다. persistent leaking 이 되는 경우 일차적으로 혹은 이차적으로도 감염이 문제가 되기 때문입니다.
3. 기존의 tube site 가 pin-point 혹은 거의 맞물리면, 그때 새로운 gastrostomy 를 처음과 같은 방법으로 넣어주면 됩니다. 이때 좁혀둔 기존의 tube site 는 knife로 넓히지 않고도 쉽게 확장됩니다.
최대 2주 정도까지 환부가 아물기를 기다린 적도 있는데, 이때는 infection 이 같이 있었습니다. 대개는 1주 정도 기다리면 환부가 좁아지고, 이 기간동안은 입원하여 금식 & 수액치료 하고 있습니다. 너무 느슨하여 leaking 이 심한 경우는 외과와 상의하여 피부연부조직까지 국소적으로 stitch한 경우도 있습니다.
교과서적인 내용이 없는 개인적 경험이지만 도움이 되셨기를 바랍니다.