 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [점막하침윤. SM invasion] - 終
[점막하침윤. SM invasion] - 終
(1) 조직검사 점막하침윤. submucosal invasion in forceps biopsy (2) 점막하암에 대한 ESD. ESD for suspected submucosal cancer. 2025-9-22
정상 성인의 위 점막하층의 두께는 얼마일까요? 어디에도 정확히 씌인 곳이 없어서 늘 궁금했는데 이번 논문에 명확히 나와 있습니다. 중앙값이 2.1 mm 라고 합니다. 평균은 2.6 mm입니다.
The mean full thickness of the submucosa (±standard variation) was 2,605 um (±1,760) and the median thickness (range) was 2,100 um (20-13,000).
점막하층 침윤의 깊이를 측정하는 기준은 어디일까요? 아쉽게도 아직까지는 병리학자들 사이에서도 통일된 규정이 없는 모양입니다. 이 논문의 discussion에는 이런 부분도 있습니다. "Standardization in measuring submucosal invasion is needed for and objective application of the expanded indication for ESD." 따라서 다른 병원에서 제시한 기준을 이용하여 ESD 적응증이나 ESD 후 수술 적응증을 정하는 것은 위험천만한 일입니다. 자기병원 병리학자가 어떤 기준을 가지고 있는지 알아야 합니다. 만약 기준이 두개라면 submucosal invasion 깊이가 깊게 나오는 것을 판단에 이용하는 안전할 것 같습니다. 즉 어떻게 재면 400 um, 다른 방법으로 재면 700 um가 나오는 상황이라면 700 um로 판단하는 것이지요. 즉 수술을 보내는 것입니다. 아직 expanded indication에 대한 명확한 근거가 없는 상황이므로 안전하게 가는 것이 좋지 않을까요?
The depth of submucosal invasion was the length (in um) from the lower border of the muscularis mucosae to the point of the deepest tumor penetration. When the continuity of muscularis mucosa was disrupted due to tumor infiltration or ulcer formation, or only a small fragment separately remained in the upper submucosa, the length was measured on the virtual line of the muscularis mucosae, based on the remaining adjacent layer, to the point of the deepest tumor penetration.
아래 그림을 보시면 submucosal invasion 깊이를 측정하는 것이 만만한 일이 아님을 느낄 수 있습니다.
2023년 발표된 위암병리 가이드라인에서는 "use the lowest surface of the original, unmodified muscularis mucosase as the reference point"라는 언급과 함께 아래 그림이 제시되었습니다.
 3. 500 um를 기준으로 하는 expanded indication에서 림프절 전이의 빈도는?
3. 500 um를 기준으로 하는 expanded indication에서 림프절 전이의 빈도는?
점막하암은 expanded indication에 속하더라도 점막암에 비하여 ESD 후 재발 위험이 높다는 임상 경험을 이야기 하는 의사가 많습니다. 이야기하는 의사는 많은데 논문으로 내는 의사는 적습니다. Extragastric recurrence에 대한 보다 많은 연구가 필요하다고 생각합니다. 오래 전 점막하암의 림프절 전이 위험에 대한 논문들이 유행처럼 발표되던 때가 있었습니다. 김태세 교수님께서 정리한 내용을 소개합니다. 림프절 전이 위험이 생각보다 높습니다.
한 연구(?)의 discussion은 아래와 같은 문장으로 시작하고 있습니다. 즉 Gotoda 등의 초기 연구와 달리 expanded indication에 해당하는 위암에서도 림프절 전이가 종종 발견된다는 것입니다. 이번 연구에서는 3.9%였습니다.
Since Gotoda et al. reported no lymph node metastasis in minute submucosal cancer, a 'depth of submucosal invasion of 500 um' has become a key criterion for the curability of ESD. However, higher incidences of lymph node metastasis were reported in several Korean studies, and the 500 um criterion has been debated. The present study also shows 3.9 % of lymph node metastasis in minute submucosal cancer, and evaluated the validity of the 500 um criterion using ROC curve analysis. As a result, the highest negative predictive value was observed at a cutoff value of 300 um.
따라서 저자들은 새로운 cutoff를 검토하였고 500 um가 아니라 300 um가 더 적당하다고 제안하고 있습니다. 여하튼 expanded indication에 대해서는 조심, 조심, 또 조심 하는 수 밖에 없다고 생각합니다.
딱 500um라는 결과가 나오면 수술을 권해야 할지 말아야 할지 고민입니다.
2022 KGCA 가이드라인은 500 um이하까지는 경과관찰이 가능하다고 씌여져 있습니다. 500이면 수술하지 않아도 좋다는 의견이라고 보입니다.
환자에게 설명하기도 어렵습니다. 어떤 예입니다.
 5. 대장암 점막하침윤. Submucosal invasion in colon cancer
5. 대장암 점막하침윤. Submucosal invasion in colon cancer
내시경으로 절제한 대장암의 침윤깊이 평가는 제법 까다롭습니다. 대장암 병리보고서 기재방안 표준화 2판(PDF, 2019)에서 제시된 기준에 따르면 pedunculated tumor와 sessile tumor에서 서로 다른 기준이 제시되어 있습니다. 유경성 폴립은 Haggitt level의 neck (level 2)이 침윤을 측정하는 기준입니다.
대장암 병리보고서 기재방안 표준화 2판(PDF, 2019)에서 제시된 기준
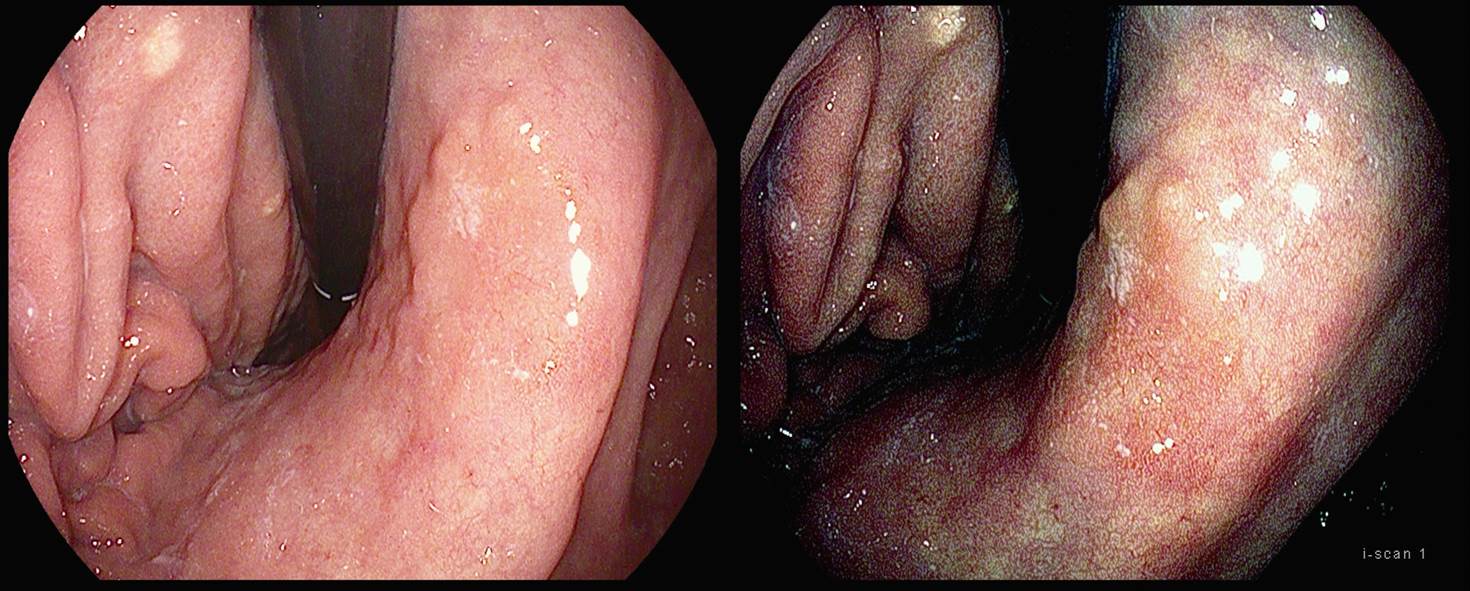
[조직검사에서 점막하침윤이 나온 증례, Submucosal invasion in forceps biopsy]
(1) 조직검사 점막하침윤. submucosal invasion in forceps biopsy (2) 점막하암에 대한 ESD. ESD for suspected submucosal cancer. 2025-9-22
[위암 512]
위암 내시경 치료 후 일부 환자에서 expanded criteria에 해당하는 소견이 나옵니다. 크기 3cm 이하이고 minute submucosa invasion이 있는 경우는 expanded criteria에 만족하여 추적관찰을 권하는 것으로 되어 있습니다.
This is a very famous table for expanded indication. Three boxes in group B are expanded indications for ESD. However, the yellow box, group C, is considered to be an expanded indication by some endoscopists. So, there are two different definitions for expanded indications of ESD. Only B versus B and C. We need to be very careful when we read literatures on expanded indications.
There is an important thing that we sometimes forget. Indications are different from criteria. Indication is something that we consider before the treatment. Criteria is something we consider after the treatment. In this regard, selection of patients for ESD can be different from selection of patients for additional surgery after ESD.
This is an algorithm from a Japanese literature. ESD candidates are selected by the absolute indications. Expanded indications are not considered for ESD in this flowchart. After ESD and histological assessment, you can see the concept of expanded criteria. When the lesion is slightly over the standard guideline criteria, you can choose close follow-up rather than additional surgery. So this group of patients was originally considered as an absolute indication, but after ESD they were changed into expanded criteria. So, indication and criteria is different in terms of the timing. Indication is before ESD, criteria is after ESD. We should not confuse them. But until now, the two terminologies are used interchangeably. I don’t like it.
저는 2-3cm 사이는 약간 조심스럽게 접근하고 있습니다. 최대한 자세히 설명하고 환자의 판단을 존중한다는 입장을 가지고 있습니다. 증례입니다.
Stomach ESD
Early gastric carcinoma
1. Location : angle, lesser curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 22 mm (2) vertical diameter, 19 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 100 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N), safety margin : distal 7 mm, proximal 5 mm, anterior 4 mm, posterior 10 mm, deep 200 ㎛ (sm only)
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
저는 환자에게 아래와 같이 설명을 하였습니다.
내시경 시술 후 최종 병리결과를 확인하기 위한 외래 방문입니다. 내시경으로 절제한 조직에 대한 병리결과에서는 세포형, 깊이, 범위, 림프관/혈관 등을 관찰합니다. 최종 결과에 따르면 다른 것은 큰 문제가 없는데 깊이에 있어서 점막하층(위벽 4층 중 제 2층)에 아주 약간 (0.5 mm 이하) 들어간 것으로 나왔습니다. 확대적응증이라고 부르는 범위에 속하는 상황입니다. 표준적인 적응증을 다소 초과한 상황이라는 의미입니다. 이 정도에서는 적극적으로 수술을 권하지는 않는 것이 상례입니다. 수술하지 않고 경과관찰을 하는 경우 재발률은 5% 전후로 보고 있습니다. 위내에 재발하는 경우도 있고 드물게 원격 전이를 보이는 경우도 있습니다.
물론 수술을 하게 되면 재발률을 약간 줄일 수 있다는 의견도 있습니다만 수술은 수술입니다. 위를 최소한 2/3 정도 잘라야 하고 주변 림프절까지 박리하기 때문에 수술에 따른 합병증과 수술 후 삶의 질 저하를 함께 고려해야 합니다. 전신마취의 위험도 무시할 수 없습니다. 이러한 내용을 모두 종합할 때, 즉 수술의 득과 실을 고려할 때 현재는 수술보다는 경과관찰이 다소 유리할 수 있는 상황입니다.
저희는 충분히 설명하고 환자의 의견을 존중한다는 입장입니다. 이런 경우는 보통 생각할 시간을 드리고 있습니다. 1주일 후 외래를 잡아드리겠으니 충분히 생각한 후 의견을 주시기 바랍니다.
1주일 후 경과관찰을 결정하시면 인공 궤양은 다 아물었는지, 잔류병소는 없는지 확인하기 위하여 2-3개월 후 내시경 검사를 하고 있습니다. 퇴원시 이미 예약되어 있을 것입니다. 이후는 3년 동안은 6개월 간격으로, 그 이후는 검사 간격을 조금 늘리고 있습니다. 가급적이면 1년 정도는 본 병원에서 검사받으시기 바랍니다. 그 이후는 원하시면 가까운 의료기관으로 되의뢰 소견서를 작성하여 옮겨드리고 있습니다. 싱겁게 드시고 균형되고 건강한 식생활을 권합니다. 술과 담배는 좋지 않습니다.
보통 2달 정도 약이 필요한데 남은 약은 충분하십니까?
계획: 1주일 후 외래
고령 환자에서는 절대적응증을 약간 초과한 경우 내시경 절제술을 시도하기도 합니다. 그런데 최종 병리과 아래과 같이 나오면 수술을 권하지 않을 수 없습니다.
1) EndoTODAY 점막하침윤 submucosal invasion
© 일원내시경 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.