 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Ampullary adenoma and adenocarcinoma. 유두부 선종과 유두부 암] - 終
[Ampullary adenoma and adenocarcinoma. 유두부 선종과 유두부 암] - 終
3. Ampullary adenomas 유두부 선종
4. Ampullary cancers 유두부 암
7. FAQs
8. References
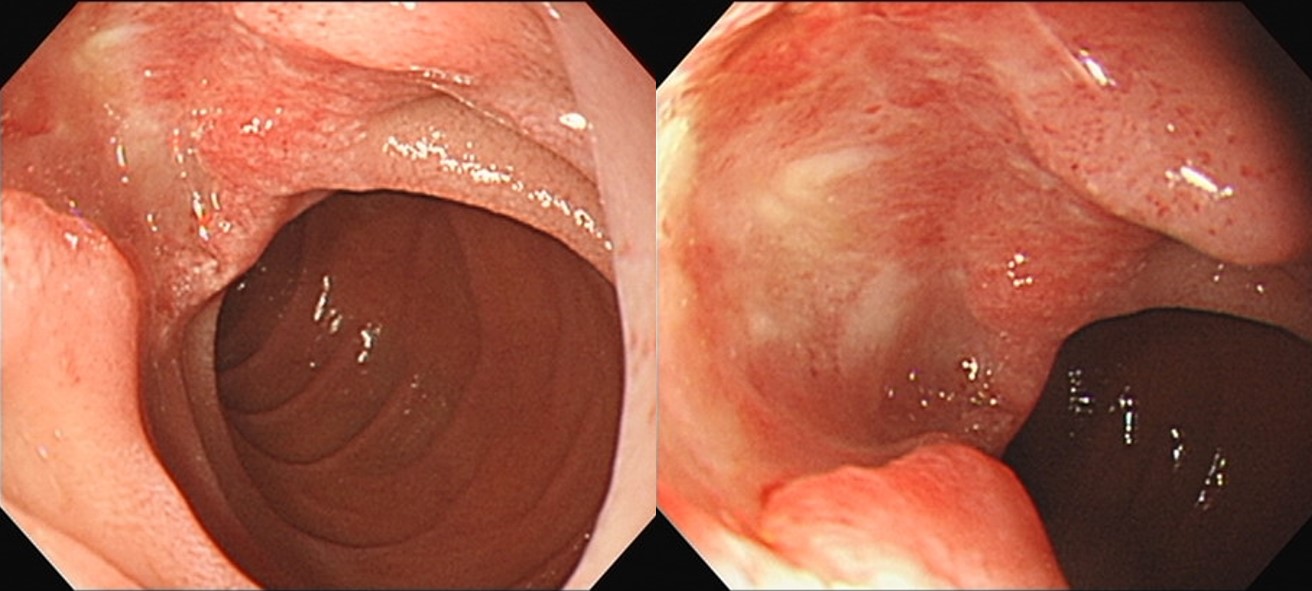
Pentax IMAGINA로 관찰한 정상 유두부
직시경과 측시경을 모두 다룰 수 있으면 좋습니다. 상부내시경에서 ampullary lesion이 의심되어 즉시 측시경으로 내시경을 바꿔 조직검사하여 ampullary cancer를 발견하여 의뢰주신 환자입니다. 대단합니다. ERCP 의사가 아니더라도 측시경에 좀 더 관심을 갖기 바랍니다.
[2016-8-2. Web-seminar 질문]
진단 내시경에서 십이지장 유두부를 모든 환자에서 확인하시는지요?
[이준행 답변]
상부위장관 내시경 검사의 범위는 십이지장 제2부까지가 맞습니다.
2주기 검진기관평가 기준 1.2 과정평가(위내시경) 항목에 "1.2.6 항상 십이지장까지 삽입하고 영상기록(화상 8번; 십이지장 2부)을 남기는가?"라는 언급도 있습니다 (참고자료).
문제는 십이지장 2부에 들어가는 일, 유두부를 찾고 관찰하는 일이 늘 쉬운 것은 아니라는 점입니다. 10명에 9명 정도는 쉽고 빠르고 자연스럽게 십이지장 2부에 들어갈 수 있지만, 간혹 조금 복잡한 조작을 해야만 들어갈 수 있는 경우도 있고, 아주 어려운 경우도 있습니다. 십이지장 2부에 들어갔으나 유두부를 정확히 찾고 상세히 관찰하기 어려운 경우도 많습니다.
저는 무증상 성인의 검진 내시경에서 십이지장 2부와 유두부는 '가능하면 보되 무리하지는 않는다' 정도로 생각하고 있습니다. 십이지장 2부와 유두부를 보려고 너무 많은 시간을 사용한 후 막상 중요한 위를 자세히 관찰하지 못한다면 무슨 소용이 있겠습니까?
뭔가의 증상이 있어 시행하는 내시경은 전혀 다릅니다. 빈혈, 황달, 복통 등에서는 십이지장 2부와 유두부를 면밀히 관찰해야 합니다.
빈혈로 시행한 내시경 검사에서 발견된 AoV cancer (마지막 내시경: 6개월 전)
일반 내시경 끝에 cap을 장착하면 십이지장 유두부를 조금 더 잘 관찰할 수 있습니다 (Abdelhafez M. Am J Gastroenterol 2017). 모든 환자에게 필요할 것 같지는 않고, 유두부를 자세히 관찰해야 할 필요가 있는 환자에서 적용해 볼 수 있을 것 같기도 합니다. 아예 처음부터 측시경을 사용하는 것도 한 방법이기는 합니다만.
[2021-3-28. 애독자 질문]
53세 남성입니다. 무엇보다 등이 아파서 잠을 자기가 어렵다고 내원했습니다. 내시경을 보면 십이지장 구부 이하로 진입자체가 불가능합니다. 이 환자는 2년마다 정기적인 공단위암검진을 착실히 받아오던 분이었습니다. 하지만 안타깝게도 직전 2년전 사진을 보면 구부만 촬영되어 있고 제2부에 진입하지 않았습니다. 당시 이 환자의 검사를 시행하였던 선생님은 원내에서 "fast hand"로 유명하신 분이었습니다. 위내시경의 첫 사진부터 끝 사진까지 60초가 걸리지 않고, 대장내시경에서도 맹장의 遠景사진부터 끝사진까지 절대 5분을 넘기지 않습니다. 병원 경영진이나 간호사들이 좋아했던 이상적인 내시경 의사상이었습니다.
이 환자의 4년, 6년전 사진들을 보면 다른 선생님들은 AOV를 촬영은 했지만 정면상을 보지는 못했습니다. 저 역시 이보다 더 잘찍을 자신은 없습니다. 어떻게 하면 AOV를 잘 볼 수 있을까요? 복부를 눌러 보는 방법은 어떤가요? AOV를 보지 못했거나 내가 본게 major 인지 minor papilla인지 구분이 안된다면 그 사실을 수검자에게 알려줘서 3차기관에서 side scope으로 재검사를 받도록 권고해야 될까요? 십이지장의 굴곡이 심한 수검자들에서 정면상의 AOV를 보려 노력하다보면 스콥으로 인한 트라우마로 점막출혈이 생기고, 검사후 복통의 원인이 되는것 같습니다.
이 환자는 이후 대학병원에서 십이지장암과 국소전이로 수술, 담즙누출로 재수술, 9차에 걸친 항암치료를 받으면서 아직 병마의 손아귀에서 힘들게 지내고 있습니다.
[2021-3-28. 이준행 답변]
1
'Fast hand'는 바른 내시경이 아닙니다. 검진 위내시경 검사의 적절한 검사 시간은 5분입니다. 잘못된 검사에 대하여 저는 할 말이 없습니다. 정도를 지킵시다.
2
무증상 성인의 검진 위내시경에서 십이지장 제2부, 특히 유두부를 꼭 보아야 하는지는 논란의 여지가 있습니다 (EndoTODAY 위내시경에서 유두부를 꼭 관찰해야 하는가?). 저는 무증상 성인의 검진 내시경에서 십이지장 2부와 유두부는 '가능하면 보되 무리하지는 않는다' 정도로 생각하고 있습니다.
검진 위내시경의 목적은 위암의 조기 진단입니다. 검진 위내시경에서 아주 작은 식도암과 아주 작은 십이지장 암까지 모두 발견해야 한다는 것은 지나친 기대입니다. 사실 의학적인 근거도 없습니다. Screening이 필요한 암도 있고 screening의 효과가 입증되지 않은 암도 있습니다. 저는 무증상 성인께서 검진 윈내시경에서 식도의 악성 질환이 발견되어 식도 수술을 받고 합병증으로 곧 사망한 예도 보았습니다. 그 분에서 검진 내시경이란 무슨 의미가 있었던 것일까요?
모든 검사는 specificity와 sensitivity가 있습니다. 십이지장 질환에 대한 상부내시경의 sensitivity는 상당히 낮습니다. 2년 전 검사에서 십이지장 제2부를 보지 못한 것은 안타까운 일이나 이 환자에서 십이지장 제2부를 보지 않았다고 검사하셨던 선생님을 탓하기는 어려울 것 같습니다. 2년 전에는 전혀 병이 없었을 수도 있습니다. 다만 모든 환자에서 십이지장 제2부를 관찰하지 않는 습관이 있다면 조심스럽게 검사 pattern을 바꾸시도록 권하는 것이 어떻겠습니까? 위내시경의 바람직한 검사 시간이 5분이라는 것도 주지시켜 주시면 좋겠습니다. 서로 좋은 방향으로 간섭하는 것이 바람직한 전문가 사회의 모습일 것입니다.
[2017-5-13. 이준행 추가] Ampulla of Vater 근처에서 조직검사 할 때에는 늘 pancreatitis를 주의해야 합니다. 어느 책에서 흥미로운 그림을 보았기에 아래에 옮깁니다.
 2. Ampullary neoplasm의 내시경 분류 (자료제공: 부산대학교 강대환 교수님)
2. Ampullary neoplasm의 내시경 분류 (자료제공: 부산대학교 강대환 교수님)
건진 내시경의 본질은 위암의 조기진단입니다. 건진개념으로 시행한 상부위장관 내시경에서 유두부 선종이 간혹 발견됩니다. 무증상 유두부 선종을 모두 치료해야 하는지 저는 알지 못합니다. 치료에 따른 합병증 위험이 상당하기 때문에 무증상 성인의 유두부 선종을 치료해야 하는지 면밀한 검토가 필요합니다. 2010년 현재 유두부 선종이 발견되면 치료하는 것이 통례입니다. (EndoTODAY 20101002)
Ampulla of Vater adenoma. 직시경으로 검사할 무렵 diverticulum을 보지 못했으나, ERCP 팀에서 papillectomy를 할 때 AoV옆에 diverticulum이 있음을 확인하였음.
Transduodenal ampullectomy, Tubulovillous adenoma, high grade dysplasia, 1) tumor size: 2.8x2.5 cm, 2) negative resection margin
Ampullary hyperplastic polyp으로 의뢰되었으며, outside slide review에서 villous adenoma로 나와 endoscopic papillectomy 시행하였고 최종 병리결과는 tubulovillous adenoma with focal high-grade dysplasia였음.
2020년 9월 10일 내시경집담회에서 나지은 선생님께서 리뷰하신 내용입니다.
F/70 (2018)
Histopathologic Diagnosis: Ampullary Carcinoma
-Type of surgery: pylorus preserving pancreaticoduodenectomy (PPPD)
(1) Histologic type: Adenocarcinoma
(2) Histologic Grade: G2 (moderately differentiated)
(3) Tumor extent
- tumor size: greatest dimension: 2.6x2 cm
- epicenter: papilla of Vater
- Intra-ampullary adenoma (IAPN): absent
- involvement of pancreatic duct: present (intraductal spread of adenoma)
(4) T3a: Tumor invades pancreas (up to 0.5 cm) with pancreato-duodenal groove soft tissue
(5) N0: No regional lymph node metastasis ( 0 / 17 : "LN #12", 0/6 ; "LN #6", 0/1 ; "LN #8", 0/2 ; "LN #7", 0/3 ; peripancreatic, 0/5 )
(6) Margin status
- Retroperitoneal surface: negative
- Duodenal margin: negative
(7) Perineural and neural invasion: absent
(8) Lymphovascular invasion: not identified
(9) Tumor necrosis: absent
(10) ICD code: M8500AoVca
Pylorus preserving pancreaticoduodenectomy (PPPD): Ampullary Carcinoma
(1) Histologic type: Adenocarcinoma
(2) Histologic Grade: G2 (moderately differentiated)
(3) Tumor extent
- tumor size: greatest dimension: 1.8x1.5 cm
- epicenter: intra-ampullary
- Intra-ampullary adenoma (IAPN): absent
- involvement of pancreatic duct: absent
(4) T3b: Tumor invades pancreas (up to 0.5 cm), duodenum, and pancreatoduodenal groove soft tissue
(5) N2: Regional lymph node metastasis (≥4) with extranodal extension (largest one: 6 mm)
( 4/24 : LN12, 0/1 ; LN8, 0/4 ; LN7,9, 0/7 ; LN16, 0/6 ; peripancreatic, 4/6 )
(6) Margin status
- Retroperitoneal surface: negative
- Duodenal margin: negative
(7) Perineural and neural invasion: present
(8) Lymphovascular invasion: present
(9) Tumor necrosis: absent
(10) ICD code: M8500AoVca
R0: complete resection with grossly and microscopically negative resection margins
AJCC stage (2018, 8th ed) Stage IIIB T3 N2 M0
30대 남자에게 황달이 오면 간염부터 생각하게 됩니다. 그러나 드물게 악성질환인 경우도 있습니다. 이 환자는 Ampulla of Vater cancer였으며 PPPD 수술을 하였고 아래와 같은 결과였습니다. 3년 후 multiple hepatic metastasis를 보였습니다.
Adenocarcinoma, moderately differentiated
(1) T1 : Tumor limited to AoV or sphincter of Oddi (extension to submucosa)
(2) Involvement of pancreas and duodenum : absent
(3) Extension to distal common bile duct : absent
(4) N0 : No regional lymph node metastasis (0/28: pericholedochal, 0/21; peripancreatic, 0/7)
(5) M0 : No distant metastasis
(6) Negative (pancreas, common bile duct, retropancreatic) resection margins
내시경 조직검사에서 adenoma with HGD and suspicious carcinomatous transformation으로 나와 papillectomy를 시도하였으나 non-lifting sign을 보여 PPPD 수술을 하였습니다.
Ampullary Carcinoma arising from IAPN
(1) Histologic type: Adenocarcinoma
(2) Histologic Grade: G2 (moderately differentiated)
(3) Precursor lesion: Adenoma
(4) Invasive tumor size: greatest dimension (0.5cm) (S/N)
(5) T1b Tumor invades into perisphincteric and duodenal submucosa
(6) N0: No regional lymph node metastasis (0/13: LN8, 0/5; LN12, 0/3; periductal, 0/5)
(7) cM0: Clinically No distant metastasis
(8) Involvement of portal vein: absent
(9) Margin status; Bile duct margin : negative; Retroperitoneal margin: negative; Duodenal margin: negative (safety margin: 4cm)
(10) Perineural and neural invasion: absent
(11) Lymphovascular invasion: not identified
측시경 소견. Fever/chill로 CT를 먼저 찍고 ampullary cancer 의심하에 의뢰되어 ERBD 후 수술. 림프절 전이 있어서 adjuvant chemotherapy
Histopathologic Diagnosis: Ampullary Carcinoma
-Type of surgery: pylorus preserving pancreaticoduodenectomy (PPPD)
(1) Histologic type: Adenocarcinoma
(2) Histologic Grade: G2 (moderately differentiated)
(3) Tumor extent
- tumor size: greatest dimension: 1.2 cm
- epicenter: intra-ampullary
- Intra-ampullary adenoma (IAPN): present (arising from IAPN)
- involvement of pancreatic duct: absent
(4) T1b: Tumor invades into perisphincteric and duodenal submucosa
(5) N1: Regional lymph node metastasis (1-3) with / without extranodal extension (largest one: 4 mm) ( 1 / 11 : LN7,9, 1/4 ; LN8, 0/1 ; LN12, 0/1 ; peripancreatic, 0/5 )
(6) Margin status
- Retroperitoneal surface: negative
- Duodenal margin: negative
(7) Perineural and neural invasion: absent
(8) Lymphovascular invasion: present
(9) Tumor necrosis: absent
(10) ICD code: M8500AoVca
NSAID 복용중 발생한 epigastric pain으로 시행한 EGD에서 ampulla of Vater cancer가 발견되어 수술
AoV cancer with multiple liver metastasis
 5. Neuroendocrine carcinoma of ampulla of Vater involvement th multiple liver metastasis
5. Neuroendocrine carcinoma of ampulla of Vater involvement th multiple liver metastasis
황달로 시행한 내시경에서 십이지장 제2부에 융기부가 있었습니다. 측시경으로 바꿔 검사한 바 병소가 잘 관찰되었습니다. EST를 조금 넣은 후 조직검사를 시행하였습니다.
PPPD 후 내시경 소견은 환자마다 다르고 상당히 어렵습니다. 저도 아직 머리에 잘 그려지지 않습니다. 혹시 잘 설명해 주실 선생님 안 계십니까?
[2014-10-17. 애독자 질문]
Duodenum ampulla lesion에 대해서 문의드립니다. 개인적으로 저는 ampulla 모습도 사람에 따라 참 다양하다 느끼는데 최근 건진쪽에만 계속 있다보니 ampulla adenoma 가 있는 모습과 정상인 모습이 분간이 모호하다 생각이 들어 교수님 께서는 어느 때 생검을 하게 되는지 궁금합니다. 사실 저는 cost 등을 생각하면 꼭 필요할때 아니면 하지 말자는 생각이 들어 필요한 것이 아니면 잘 안하게 되는데, 이렇게 생각하는 제가 이상한 것인가 하는 생각이 요즘 듭니다. 교수님의 고견을 부탁드립니다.
[2014-10-20. 이준행 답변]
무척 중요한 질문입니다. 그런데 저도 답이 없습니다. Ampulla of Vater는 사람마다 다르게 생겼으니까요. 그리고 무엇보다도 직시경으로 정면상을 볼 수 없기 때문에 어렵습니다.
언제 생검해야 하는지 문의하셨는데요... 저는 그냥 '왕창 튀어나왔으면 조직검사 한다' 정도로 생각하고 있습니다. 메일 주신 것처럼 애매하면 안 한다는 전략도 나쁘지 않다고 생각합니다. Ampulla of Vater adenoma 과잉진단에 따른 폐해도 적지 않을 것이기 때문입니다. 뾰족한 답을 드리지 못하여 죄송합니다. 혹시 다른 애독자께서 선생님의 답변에 대답을 주실 수 있다면 감사하겠습니다.
문득 예전에 어떤 애독자께서 보내주신 메일이 생각나서 옮깁니다. 내시경을 하다가 웃는 얼굴을 만나서 놀랐다는 일화입니다.
[애독자 편지 2013-4-3] 안녕하세요? 누구나 다 그렇겠지만 바쁜 일정 속에 시간을 따로 내어 공부하기란 쉽지 않은데 교수님의 Endotoday를 받아보면서 많은 도움을 받고 있습니다. 늘 감사드립니다. 오늘 보내 주신 십이지장 관련 내용을 보면서 문득 과거에 참 재미있는 사진이라 생각되어 저장해 두었던 십이지장 유두부 사진이 생각났습니다.
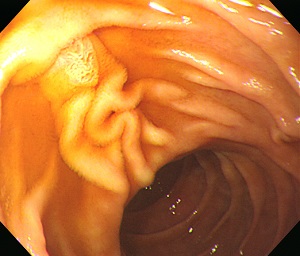

십이지장 제2부로 들어가 주유두부를 확인하는 순간 깜짝 놀랐습니다. 그 곳에는 사람의 얼굴이 있었습니다. 지금은 그저 웃고 넘길 일이지만 당시에는 해외토픽에 가끔 나오는 예수님 얼굴 형상을 발견한 것처럼 놀랐습니다. 학문적인 내용은 아니지만 바쁘고 지치신 일상 속에 한번 웃으시라고 사진 보내드립니다.
[2020-2-24. 애독자 질문]
십이지장 2부에 prominent ampulla 소견으로 보이는데요, 가끔 이렇게 보이는 경우 조직검사를 해야 할지 고민입니다.
이 환자는 협조도 잘 되지 않아 조직검사를 하기에도 무리가 있어 관찰만 하고 검사를 마쳤습니다. 내시경 소견을 리뷰하면서 정상 variation인 것 같은 느낌이 들긴 하지만 조직검사를 하지 않은게 조금 마음에 걸립니다. 이런 경우 언제 다시 추적검사를 하는게 나을지 고민입니다. 교수님의 의견을 듣고 싶습니다.
[2020-2-24. 이준행 답변]
안녕하십니까. 사진 몇 장으로 정확히 평가하기는 어렵습니다. 그래서 일반론으로 답변을 대신합니다.
Ampulla of Vater는 황달이나 복통 등 상복부 증상이 있는 환자의 symptom evaluation endoscopy의 관찰대상입니다. 무증상 성인의 screening endoscopy에서 ampulla of Vater를 꼭 보아야 하는지, 본다면 어느 정도 자세히 평가해야 하는지 고민이 아닐 수 없습니다.
무증상 성인의 screening endoscopy에서 애매하게 보이는 ampulla of Vater의 조직검사에서 의미있는 병이 나와 멋지게 치료된 환자는 많지 않을 것 같습니다. (물론 뚜렷한 병소가 있으면 조직검사를 통하여 진단해야 합니다. 2018년 한 애독자께서 발견한 ampulla of Vater의 드문 cancer 증례를 보시기 바랍니다.) 반대로 이 부위 치료를 하다가 엄청 고생한 환자도 여러번 보았습니다. 아시다시피 이 부위의 치료는 내시경이나 수술이나 모두 간단한 일이 아닙니다.
여하튼 biliary tract나 ampulla of Vater는 검진 영역은 아닙니다. 검진대상이 아닌 부위에 대한 적절한 검사나 치료 수준을 결정하는 것은 쉬운 일이 아닙니다. 저는 무리하지 않는 쪽이 낫다고 생각하는 편입니다. 감사합니다.
[2021-7-15. 애독자 편지]
교수님 안녕하십니까? 엔도투데이로 공부하는 내과 개원의입니다. 요즘 십이지장에 AoV, minor papilla 가 prominent 할 경우, Adenoma, SET 감별에 위해 종병 의뢰여부 판단에 어려움 있습니다. 몇몇 케이스는 종병에 의뢰해도 괜찮은 것으로 나왔습니다. ?
AoV, minor papilla 내시경 소견에 대해 아틀라스 책을 사서 공부를 하고 싶은데, 책 검색을 해봐도 그 부분만 나오는 내시경 사진 책은 못 찾겠습니다. AoV, minor papilla 에 대한 내시경 아틀라스 책이 혹시 나와 있는지 해서 고민하다가 문의드립니다. 교수님, 감사합니다.
[2021-7-15. 이준행 답변]
출판 강국 일본을 따라갈 나라가 없습니다. 저는 일본어를 배우지 못했으나 한자는 조금 알고 히라카나와 가타카나를 조금 익혀서 일본 내시경책을 참고하고 있습니다.
우리나라 의사들도 책을 많이 내면 좋을 것 같습니다. 저도 작은 책 하나 쓰고 있습니다. BOXIM과 DEX에 대한 내용입니다. 내년 초 발간이 목표입니다.
[2022-1-10] 드디어 나왔습니다. 참고하시기 바랍니다.
1) ERCP in surgically altered anatomy 2023년 KSGE Webinar. 아주대학교 양민재. Log-in 要 - 참고: Surg Endosc 2022
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.