 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
How many biopsies do you take for suspected advanced gastric cancer (AGC)? I would recommend 6 biopsies for AGC. Four biopsies from the edges and two biopsies from the bottom is usually enough for pathological diagnosis. The more the better? No, I don't think so. Too many biopsies are not efficient in terms of the cost and the labor.
@ 2012-7-2. 이준행
How many biopsies do you take for suspected early gastric cancer (EGC)? If the EGC lesion is large and/or deep, I would recommend 4-6 biopsies.
Careful targeting is important for small EGC. In candidate cases for ESD (endoscopic submucosal dissection), I would recommend no more than 3 biopsies. Too many biopsies can make significant submucosal fibrosis, which makes the ESD procedure difficult.
When a patient with EGC is referred with good endoscopic pictures, I would not repeat endoscopy before ESD. Abdominal CT scan and the review of outside slides usually give enough information.
@ 2012-7-3. 이준행
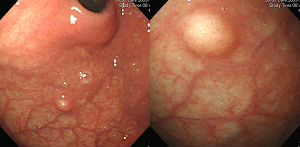
 3. Erosive gastritis and single erosion
3. Erosive gastritis and single erosion
In erosive gastritis, taking biopsies from all the erosions is impossible. It is not even necessary. If you take biopsies from 10 erosions and one of them is cancer in pathology report, you may not localize the cancerous lesion in the repeat endoscopy. So, careful examination is more important than numerous biopsies.
When malignancy is not suspected in erosive esophagitis, you don't need to take a biopsy. If you are not sure about the findings, take some time to select most suspicious lesions and then take biopsies only from them. In practice, I usually don't take biopsy from more than 3 locations.
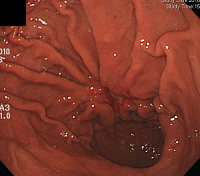
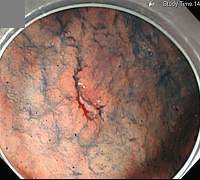
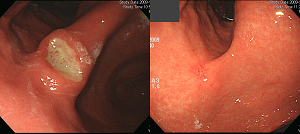
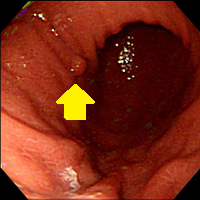
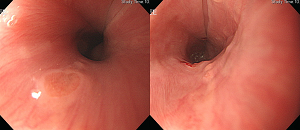
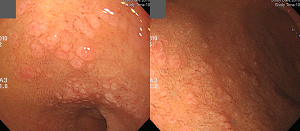
However, a small gastric cancer may be hidden among many erosions. Careful examination of every aspect of the gastric mucosal surface is important. In the following case, there were a lot of erosions at the lower body and the proximal antrum. In addition, a single large erosion with irregular edge was found at the anterior wall of the antrum. Two biopsies were taken and the result was signet ring cell carcinoma.
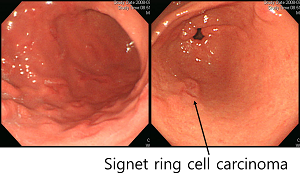
Single erosion may be benign or malignant. I recommend 2 biopsies for a single erosion. It is difficult to make a reliable pathological diagnosis with a tiny biopsy specimen. Two pieces of biopsy for one lesion may be better.
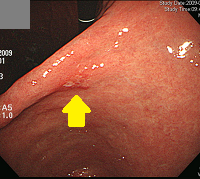 early gastric cancer
early gastric cancer
@ 2012-7-4. 이준행
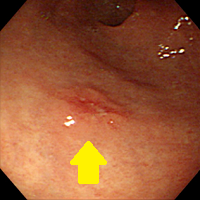
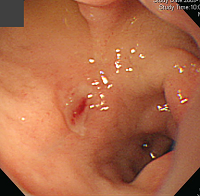
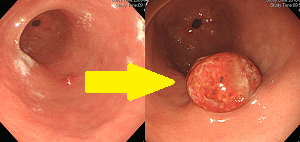
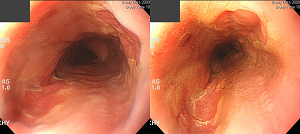
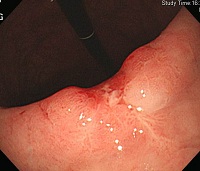
After a successful hemostasis for bleeding ulcers, many endoscopists don't take biopsies from the ulcer. However, some malignant ulcers may bleed.
When the second-look endoscopy was commonly recommended, there was a chance to take biopsies the next day. However, second-look endoscopy is not recommended anymore. Therefore, biopsies should be taken in the first endoscopy. When you are careful, the risk of bleeding from biopsies must be very low.
Recommendation: After the endoscopic hemostasis, take 2 or 3 biopsies from the ulcer edge for histology and do the CLOtest.
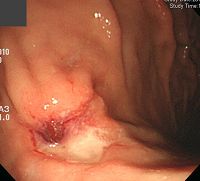
EGC, presenting with hematemesis
@ 2012-7-6. 이준행
 5. First follow-up endoscopy after treatment of gastric ulcer
5. First follow-up endoscopy after treatment of gastric ulcer
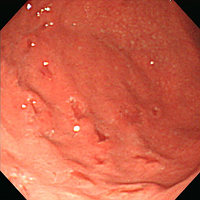
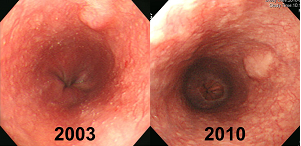
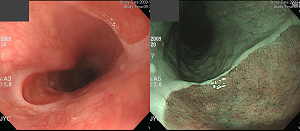
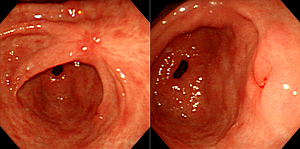
The sensitivity of biopsy for gastric cancer is not 100%. I usually tell the patient that the sensitivity of biopsy is about 80-90%. Follow-up endoscopy with biopsy is strongly recommended.
Recommendation: In the first follow-up endoscopy for benign gastric ulcer, take 2 or 3 biopsies from the ulcer. It is the same for ulcer scars.
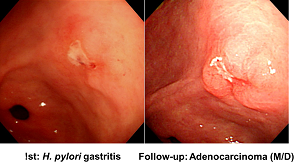
The first biopsy for this lesion was benign. Malignancy was diagnosed in the first follow-up endoscopy a few weeks later.
@ 2012-7-7. 이준행
 6. Second or later follow-up endoscopy after treatment of gastric ulcer
6. Second or later follow-up endoscopy after treatment of gastric ulcer
In patients with BGU, yearly endoscopic follow-up is usually recommended. I am not sure whether this kind of tradition is really valid.
Do we need to take biopsies in the second or third follow-up endoscopy? When the ulcer is completely healed (scar stage), no further biopsy is required in the yearly endoscopy.
Please don't take biopsy from the ulcer scar every year. It's unnecessary and the patient don't like it.
@ 2012-7-8. 이준행
 7. Biopsies for Helicobacter pylori
7. Biopsies for Helicobacter pylori
Histological examination of the Giemsa-stained tissue is one of the most common diagnostic methods for Helicobacter infection. However, there is no standard guideline for the location and the number of biopsies.
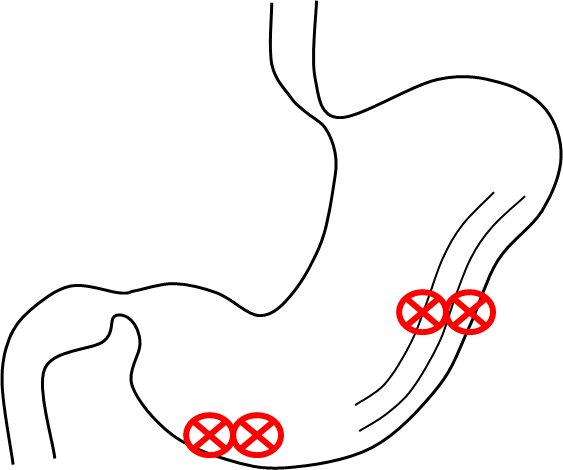
Recommendation: For the histological diagnosis of H. pylori infection, take two biopsies each from the greater curvature of the body and the greater curvature of the antrum.
@ 2012-7-9. 이준행
 8. CLOtest instead of histology
8. CLOtest instead of histology
For the diagnosis of H. pylori infection, the sensitivity and specificity of the histology and the CLOtest is comparable. Because the CLOtest is much easier than the histology (quick and no pathology slip), I would recommend the CLOtest instead of the histology.
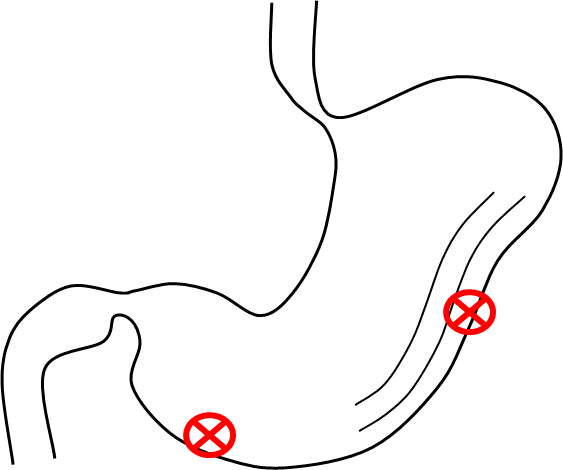
For the best CLOtest, take one biopsy each from the antrum and body, and then put the two samples into the one well of the CLOtest kit.
@ 2012-7-10. 이준행
 9. H. pylori in bleeding peptic ulcer
9. H. pylori in bleeding peptic ulcer
I previously recommended to take biopsies after the endoscopic hemostasis for bleeding peptic ulcer. In addition, you need to do CLOtest or Giemsa staining for H. pylori. I would do CLOtest in every patient with bleeding or non-bleeding peptic ulcer.
 Bleeding duodenal ulcer in an aspirin user. CLOtest is recommended in the first endoscopy.
Bleeding duodenal ulcer in an aspirin user. CLOtest is recommended in the first endoscopy.
@ 2012-7-11. 이준행
When you see a polyp for the first time, you need to take 1-2 biopsies from it. In the follow-up endoscopy, however, no more biopsy is required for a hyperplatic polyp.
There are some exceptions. Take biopsies in the follow-up endoscopy, if (1) the polyp increased significantly (>30% in diameter), or (2) malignant change is suspected.
@ 2012-7-12. 이준행
 11. Esophageal submucosal tumor (SMT)
11. Esophageal submucosal tumor (SMT)
The majority of small esophageal SMTs are benign. When a small esophageal SMT is found for the first time, 1-2 biopsies are sufficient. When the esophageal SMT is smaller than 5 mm, no biopsy may be OK in some cases. If there is no significant change, you don't need to take biopsy in the follow-up.
The most common esophageal SMT is the leiomyoma of the far distal esophagus. They are benign.
 r/o esophageal leiomyoma (histology is unavailable).
r/o esophageal leiomyoma (histology is unavailable).
Most of the biopsies for esophageal SMTs are reported as normal esophageal mucosa. One rare exception is granular cell tumor.
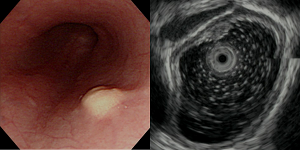 Esophageal granular cell tumor
Esophageal granular cell tumor
@ 2012-7-13. 이준행
 12. Gastric submucosal tumore (SMT)
12. Gastric submucosal tumore (SMT)
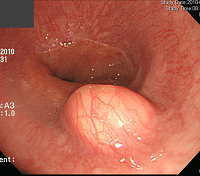
The clinical significance of the gastric SMTs is quite different from the esophageal SMTs. It's because of gastric GIST, SMT-like cancer and other important lesions. However, the majority of small gastric SMTs are clincally benign. When a small gastric SMT is found for the first time, I recommend to take 2 biopsies. If there is no significant change in the follow-up endoscopy, you don't need to take biopsy anymore. You should focus on the comparison of the size and the shape.
If there is a change in the size or the shape, I would recommend to re-evaluate the gastric SMT including endoscopic biopsies.
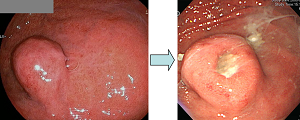 An ulcer developed in the follow-up endoscopy.
An ulcer developed in the follow-up endoscopy.
@ 2012-7-14. 이준행
Inlet patch (= heterotopic gastric mucosa) is located at just below the upper esophageal sphincter. It is usually round, flat or slightly depressed, hyperemic, columnar mucosa. Sometimes there are two inlet patches at the same level ("kissing"). Ulcer or cancer may develop from the inlet patch, but they are extremely rare. Biopsy from the inlet patch is very difficult for doctors and patients alike.
Recommendataion: If there is no specific findings like ulcer or nodule, you don't need to take biopsies from the inlet patch.
@ 2012-7-15. 이준행
 14. Gastric heterotopia of the duodenal bulb
14. Gastric heterotopia of the duodenal bulb
Gastric heterotopia is irregular, flat or nodular, usually multiple mucosal lesion of the duodenal bulb. Some authors said that an ulcer may develop from the gastric mucosa. However, it is not a precancerous lesion.
Recommendataion: When the gastric heterotopia is found for the first time, take two biopsies. In the follow-up endoscopy, however, you don't need to take biopsy.

@ 2012-7-16. 이준행
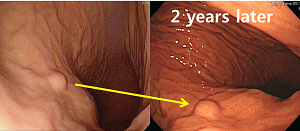
 15. Biopsies after ESD for EGC
15. Biopsies after ESD for EGC
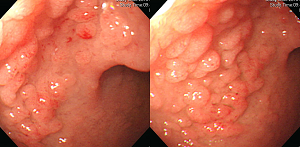
The role of endoscopy after ESD is to find the recurrence. There are two kinds of recurrence that can be found in the endoscopy: (1) local, (2) metachronous.
In patients with ESD induced ulcer, surveillance biopsy is very important to find early recurrence in ESD site. The overall incidence of metachronous recurrence is 4.7% to 8.2% during 5 years after ESD. Endoscopists have to keep in mind chance of metachronous recurrence during endoscopic surveillance.
 Local recurrence
Local recurrence
 Metachronous recurrence
Metachronous recurrence
Recommendations:
(1) Within 3 years of ESD: If the local recurrence is not suspected, take 2 biopsies from ESD-induced ulcer. If the local recurrence is suspected (such as nodular change), take 2 or more biopsies from that area. Take pictures immediately after the biopsy to document the exact biopsy site.
(2) After 3 years of ESD: If the local recurrenc is not suspected, you don't need to take biopsy.
@ 2012-7-17. 이준행
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.