 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [이질아메바 (Entamoeba histolytica). 아메바 장염. Amenic colitis] - 終
[이질아메바 (Entamoeba histolytica). 아메바 장염. Amenic colitis] - 終
1. Introduction - 이질아메바. 아메바 장염
2. 아메바 장염의 진단
3. 아메바 장염의 치료
4. Cases
5. FAQ
6. References
 1. Introdcution - 이질아메바. 아메바 장염
1. Introdcution - 이질아메바. 아메바 장염
이질아메바는 전세계 인구의 10%가 감염되어 있으며 이 중 90%는 무증상입니다. 기생충 질환중 아메바증은 schistosomiasis와 말라리아에 이어 3번째로 많은 사망원인입니다.
소화관에 기생하는 아메바는 이질아메바, 대장아메바 (Entamoeba coli), 왜소아메바 (Endolimax nana), 요드아메바(Iodoamoeba butschii) 등이지만 병원성이 뚜렷한 것은 이질아메바 뿐입니다.
주로 음식을 통하여 매개됩니다. 음식물의 이질아메바 씨스트가 원입니다. 급성아메바증의 대표적인 증상은 감염 2-6주경 시작되는 이질인데 설사변은 주로 점액과 혈액이고 fecal material은 별로 없습니다. tenesmus, 하복부의 동통과 더불어 변소 내왕이 하루에도 10-12회에 이르며 대변은 생선 내장의 썩은 냄새가 납니다. 감염이 오래되면 변비, loose stool, 복부팽만감, 하복부의 둔통등 비특이적인 증상으로 변하는 경향이 있습니다.
아메바 장염의 대장내시경 초기소견은 small ulcers with heaped up margins and normal intervening mucosa입니다. 병소의 위치는 주로 cecum입니다. 드물게 cecum과 rectum에서 동시에 병변이 발견되기도 합니다. Rectum에만 병소가 있는 경우는 거의 없는 것 같습니다. 교과서적으로 궤양은 점막하층으로 extension되어 플라스크 모양의 궤양(undermining ulcer)을 형성한다고 되어 있으나 사실 flask 모양의 증례는 거의 없습니다. 조직검사에서는 inflammatory cell이 거의 관찰되지 않는데 이는 아메바의 효소가 neutrophil을 파괴하기 때문이다. Trophozoite만 대거 관찰되기도 합니다.
아메바 장염의 내시경 소견. 지저분하고 얕은 여러 궤양이 산재된 소견이었습니다.
조직검사 소견. 붉은 화살표로 표시된 연하고 희끄무레한 큰 세포가 이질아메바 trophozoite입니다. 그 안의 붉은 것은 hemophogocytosis를 한 적혈구가 collapse된 것입니다.
혈관이나 림프계를 따라 간, 복막, 뇌, 피부, 폐 등 다른 장기에서 장외아메바증을 일으키기도 하는데 간농양이 가장 흔하며 96%가 간의 우엽에 위치합니다.
대변검사상 heme test 양성, paucity of neutrophils, presence of Charcot-Leyden crystal protein(double pyramid-shaped crystals normally found in the cytoplasm of eosinophils)등의 소견이 가능하지만 명확한 진단은 영양형(급성기)과 씨스트(만성기)를 찾으면 붙일 수 있습니다. 급성시에는 혈액과 점액이 묻어 있는 대변의 일부를 따서 되도록 빨리 (30분이상 경과하면 거의 확인할 수 없다) 현미경으로 영양형을 확인해야 한다. 백혈구와 거의 비슷한 모양을 가지고 있으나 활발히 움직이는 위족과 세포질 내의 탐식된 적혈구 등을 참조하여 동정할 수 있습니다.
큰 병원에서는 환자의 검체를 검사실에 접수하여 결과를 기다리는게 상례인데 이 경우에는 거의 아메바의 영양형을 확인할 수 없으므로 의사가 직접 검체를 들고 검사실로 달려가야 한다. 아메바의 영양형은 물, 건조, 바륨 등에 의하여 쉽게 파괴되므로 3회 이상의 검사가 필요할 수 있습니다. Six daily consecutive stool을 추천하기도 합니다.
Tissue agent와 luminal agent로 치료합니다. Tissue agent는 metronidazole이나 tinidazole입니다. Tissue agent 단독으로 치료하는 예가 많습니다.
Luminal agent(diloxanide furoate, paromomycin, iodoquinol)에 대해서는 다소 불명확합니다. 과거부터 tissue agent와 함께 luminal agent를 사용하는 것이 표준적인 치료였고, 아직도 감염내과 전문가들은 luminal agent를 쓰는 것이 좋다는 의견을 가지고 있습니다. 그러나 예전에는 국내에서 luminal agent를 구할 수 없어서 metronidazole만으로 치료하였는데, 재발 예는 많지 않았습니다. Luminal agent인 paromymycin은 희귀의약품센터에서 구할 수 있습니다. Luminal agent를 사용하지 않으면 재발률이 다소 높은 모양입니다.
제가 몇 분의 감염내과 전문가에게 물어보았습니다. 모든 환자를 희귀의약품센터에 보낼 수도 없는 일이므로, 일단 tissue agent (metronidazole)로 치료하고 재발의 치료에는 tissue agent와 함께 luminal agent를 쓰는 모양입니다.
Chronic diarrhea with episodes of hematochezia
혈변으로 내원하였고 cecum과 rectum에 병변이 있었음.
2015년 대한내시경학회 제주지회 심포지엄. 송현주 교수님 증례

2017-11-16. 전북개원내과심포지엄. 변정식 교수님 강의. 아메바 장염
만성 경한 설사로 대장내시경 후 Pentasa 오래 드셨으나 호전이 없어서 의뢰되어 시행한 대장내시경에서 아메바 장염으로 진단됨.
3달 전부터 시작된 배변시 출혈, 잦은 배변과 설과, 복통. 외부병원에서 궤양성 대장염 의심하여 치료 (EndoTODAY 애독자 증례 편지 41)
최근 하루 5회의 혈성 점액변. 해외 여행 여러 차례, 최근 중국 여행 (EndoTODAY 애독자 증례 편지 41)
무증상 건진 내시경. 여행력 없음. 텃밭 가지고 계신 분. 복부 초음파는 정상 (EndoTODAY 애독자 증례 편지 41)
7개월 전부터 혈변, 점액변, tenesmus. 외부병원서 nonspecific proctitis, ulcerative proctitis 의심하에 치료받은 바 있음 (EndoTODAY 애독자 증례 편지 41)
[2024-5. 대한장연구학회 소식지에 소개된 증례] Psoriasis로 ixekizumab (IL-17 inhibitor) 사용 후 발생한 설사로 amebic colitis 진단된 증례. Ixekizumab은 염증성장질환을 유발 혹은 악화시킬 가능성이 있으며 위장관 감염증을 증가시킬 수 있으므로 주의가 필요합니다.
[2014-8-19. 애독자 질문]
이준행 선생님 안녕하십니까? 휴가는 잘 다녀오셨습니까? 내시경을 하면서 초반에 가장 문제가 되는 것이 어떻게 병변을 describe하느냐 이었는데, 제게는 amoebiasis가 대표적인 것이었습니다. 교과서를 읽어보면 flask shape의 ulcer라고 되어 있었는데 도대체 flask shape의 ulcer라는 것이 어떤 것인지에 대한 감이 잘 오지 않았습니다. 물론 지금도 마찬가지입니다. 동양과 서양의 관념이 달라 사용하는 형용사를 어떻게 해석할 것인지가 실질적으로 중요할 것 같습니다. 선생님은 이 flask shape의 ulcer라는 것을 어떻게 번역하시는지요? 오래전 부터 이것이 궁금하였습니다.
[2014-8-20. 이준행 답변]
아시다시피 flask는 삼각형 모양의 실험도구입니다. 따라서 flask-shaped ulcer는 궤양은 궤양인데 lumen 쪽의 점막조직 결손보다 점막하층 조직결손의 범위가 큰 경우를 말합니다. 즉 궤양의 입구는 좁은데 아래 쪽이 넓은 경우입니다. 점막하층을 파고 들었기 때문에 undermining ulcer라 부르기도 합니다.

Flask-shaped ulcer는 병리 소견입니다. 아메바 장염의 병리소견 사진 두 개를 소개합니다. 아! 이래서 flask-shaped ulcer라고 하는구나.... 금방 느낄 수 있습니다.
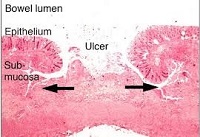

Histopathology of a typical flask-shaped ulcer of intestinal amebiasis CDC/Dr. Mae Melvin (출처)이들 궤양을 내시경으로 본다고 생각해 봅시다. Flask-shaped ulcer (= undermining ulcer)로 보일 것 같습니까? 아닙니다. 그냥 보통 ulcer로 보입니다. 제 경험과 생각으로는 amebic colitis에서 flask-shaped ulcer('플라스크모양 궤양'으로 번역해야 하지 않을까요?)를 내시경으로 관찰하기는 어려울 것 같습니다. Ginsberg 내시경책을 옮깁니다 (page 322). 더러운 점액이 부착된 다발성의 크고 작은 궤양인 경우가 많습니다. 경계는 뚜렷할 수 있고 뚜렷하지 않을 수도 있습니다.
"Amebic colitis is a protozoan infection that primarily affects the large bowel. It is most often seen in patients who recently immigrated from developing countries and who recently traveled to developing countries. Symptoms can vary from none to explosive diarrhea, tenesmus, fever and abdominal cramps.
Colonoscopic appearance during the acute phase resembles ulcerative colitis, but in the chronic phase it appears more like Crohn’s disease. The most common segments involved are the cecum and right colon, with the rectum and sigmoid less often involved. Toxic megacolon may develop in severe cases of amebiasis.
Colonoscopy reveals granular, friable, and erythematous mucosa with discrete large ulcers covered by yellowish, mucopurulent exudates. Biopsies of the margins of the ulcers provide a 60% to 90% yield of trophozoites to make the diagnosis."
Amebic liver abscess (ALA) 환자의 colonoscopy 소견을 기술한 논문이 있어서 소개합니다 (Ann Gastroenterol 2014;27: 156-161).
Colonic involvement in the form of erythema and ulceration was seen in 62 (77.5%) patients of amebic liver abscess (ALA) whereas no abnormality was seen in 18 (22.5%) patients. Cecum (70.9%) was the most common site of colonic involvement followed by lesions involving both right colon with transverse colon (35.4%) and isolated ascending colon (22.5%). There were no cases of isolated transverse colon involvement, but involvement of right colon was present in all patients with colonic involvement. Colonic lesions were more commonly seen with multiple than solitary ALA (Table 3). In patients with solitary ALA, cecum involvement (46.4%) was seen most commonly followed by isolated in the ascending colon (17.9%) and right plus transverse colon (7.1%). Most of the patients with multiple ALAs had involvement of the transverse and right colon (75%), while isolated right colon was involved in 16.6% patients. Among the 18 patients of multiple ALAs with lesions involving transverse colon, 16 had cecal lesions and two had lesions in the ascending colon. A significant involvement of the right and transverse colon was seen in cases of multiple ALAs compared to solitary ALA (P<0.0001). Histological analysis of the colonic biopsy was done in all subjects with colonic lesion; flask-shaped ulceration and acute inflammatory cells were seen commonly but trophozoite invading the lamina propria was seen in only 10 (16.1%) patients.
인터넷에서 구한 amebic colitis 내시경 사진 몇 개를 모았습니다. 어느 것도 flask-shpaed ulcer는 아니군요.
아메바 장염.
아메바 장염.
간혹 Behcet colitis에서 large undermining ulcer가 발견되는데 오히려 이를 flask-shaped ulcer라고 부를 수 있지 않을까요? 홍성노 선생님께서 제공해주신 Behcet colitis 사진 3개를 소개합니다.
2017-11-16. 변정식 교수님 강의록에서. 베체 장염에 의한 큰 undermining ulcer
그런데 곰곰히 들여다보면 이들 또한 그다지 flask 같지는 않습니다. 첫번째와 두번째 사진은 그냥 large punched out ulcer라고 부르는 것이 낫겠습니다. 세번째는 약간 underminig 하는 부분이 있기는 합니다만... 여하튼 flask-shaped ulcer는 내시경 소견이라기보다는 병리소견이라고 보는 것이 타당할 것 같습니다.
요약합니다. Amebic colitis의 내시경 소견은 flask-shaped ulcer가 아닙니다.
2) 아메바장염 대한소화기학회 교육자료 2025.5.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.