 [Description exercise 7 해설] - 終
[Description exercise 7 해설] - 終
 [Description exercise 7 해설] - 終
[Description exercise 7 해설] - 終
대장 description 연습은 처음이라 그런지 다들 어려워 했습니다. Fighting!!!
위만 공부했고 대장은 처음인지라 아래와 같은 궁금증을 갖는 모양입니다. 극히 정상입니다.
[2026-1-23. 질문] Stomach에서는 impression이 adenoma, EGC, AGC 등으로 작성했는데, colon에서는 adenoma나 polyp에서 sessile이나 pedunculated같은 형태도 적어주어야 하는지 궁금합니다.
[이준행 답변] Polyp Is 또는 Polyp Ip와 같이 간단히 써도 무방합니다. Sessile polyp, semipeduculated polyp, pedunculated polyp이라고 써도 안 될 일은 없으나 시간을 아끼기 위하여 짧게.
[2026-1-23. 질문] 대장질환에 대해 공부하다보면서 SSL과 같은 진단명도 있었는데, 이것도 impression에 적을 수 있는 것인지 궁금합니다.
[이준행 답변] 당연히 serrated lesion이라는 진단명을 써도 됩니다. Impression이니까요.
[2026-1-23. 질문] 대장 종양에서는 (염증성장질환을 제외하고) impression이 주로 polyp, LST, adenoma, early colon cancer, advanced colon cancer인데요, 이 정도 안에서 진단명을 붙이는 것인지 궁금합니다.
[이준행 답변] 예. 맞습니다. 공부를 많이 하고 경험이 쌓이면 보다 많은 진단을 impression으로 붙일 수 있게 됩니다. 그러나 처음에는 이 정도로 시작하는 것도 나쁘지 않습니다.
아래 대장질환 동영상을 꼭 보시기 바랍니다.
★ 증례를 중심으로 한 강의 동영상을 많이 보시기 바랍니다. EndoTODAY 온라인세미나 
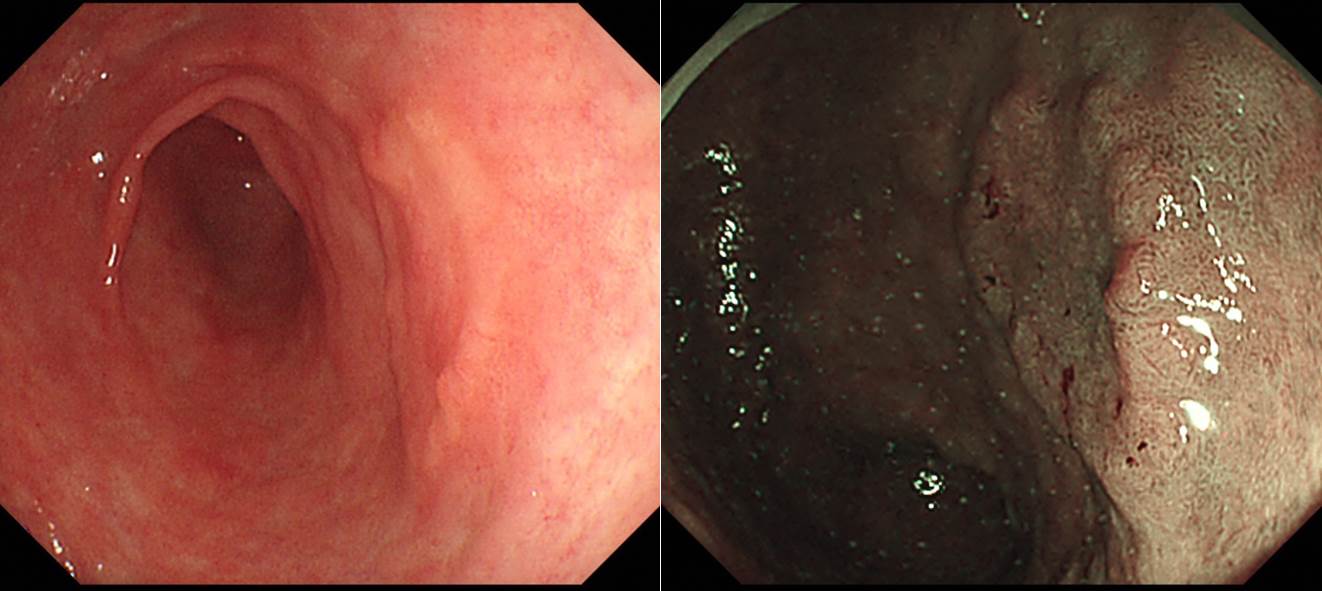
소견 (findings): 직장에 약 1.5cm 크기의 flat ovoid nodular elevated lesion이 관찰되며 경계(edge)는 분명합니다. 중앙에 약간 발적된 함몰부가 있고, 그 경계에서 spontaneous bleeding이 동반되어 있습니다.
내시경 진단 (impression): LST, pseudo-depressed type (R/O early colorectal cancer with deep submucosal invasion)
[이준행 comment]
내시경 크기 측정은 늘 대강입니다. 그러니 간단히 쓰는 것이 낫습니다.
최종 병리: ESD를 시행하였고 1.3 cm, adenocarcinoma (W/D) arising from high grade adenoma. Extension to SM 1,750 um, involvement of deep margin으로 나와 수술을 하였고 lymph node 전이가 있었습니다 (3/26).
이 정도 납작한 모양은 용종은 용종인데 LST라는 specific한 이름이 있습니다. Specific한 용어가 있으면 사용해봅시다.
LST의 subtype이 애매한데요... LST는 주로 granular와 non-granular로 나누는데... 그렇게 따지만 granular에 가깝다고 할 수도 있습니다. 그러나, 이 병소의 주된 특징은 (비록 병소의 바깥쪽 half는 granular하지만) 중앙의 약간 함몰된 소견이므로 저는 pseudodeprssed type으로 붙일 것을 제안합니다.
아래 사진 (d)를 보더라도 pseudodepressed type으로 분류되었는데 병소의 바깥쪽 부분이 약간 granular한 것을 알 수 있습니다. 완전히 매끈하면서 중앙이 함몰된 경우도 있지만 그렇지 않은 경우도 많다고 생각해 주시기 바랍니다.
제가 pseudodepression을 강조하는 이유는 아무래도 점막하 침윤이 많기 때문입니다. 림프절 전이도 많겠지요. 주의해야 한다는 뜻입니다. 조기위암도 마찬가지입니다. 그냥 EGC IIc보다 EGC IIa+IIc가 점막하 침윤과 림프절 전이가 많습니다.
비슷한 증례 하나 소개합니다. EMR로최종 병리는 점막에 국한된 선종이었습니다.
아래는 이번 quiz 문제와 매우 비슷한 모양의 위암입니다. EGC IIa + IIc도 생각보다 심달도가 깊은 경우가 많습니다. 60대 남자였습니다.
Early gastric carcinoma
1. Location : antrum, posterior wall
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 16 mm (2) vertical diameter, 14 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 400 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N), safety margin : distal 10 mm, proximal 12 mm, anterior 12 mm, posterior 12 mm, deep 250 ㎛ (sm only)
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent요즘 인터넷에는 의학 관련 강의가 넘치지만 질 좋은 강의는 많지 않습니다. 아주 훌륭한 강의를 소개합니다. ANBIIG 세미나에서 아산병원 변정식 선생님께서 강의한 내용입니다. Best of best입니다. 꼭 보시기 바랍니다. LST 부분에서 시작하도록 link를 걸었습니다만... 시간이 되면 전체를 다 보시기 바랍니다.
* 참고: EndoTODAY 대장 LST와 조직검사
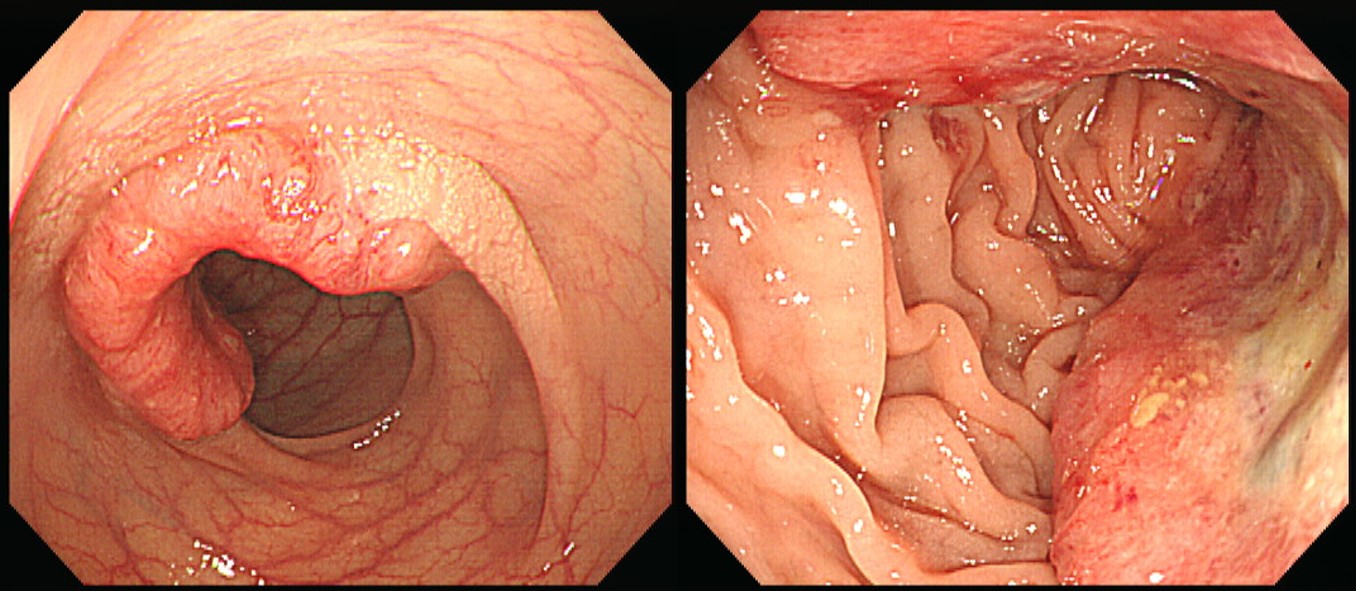
소견 (findings): Poximal A-colon에 약 3cm 크기의 polypoid mass가 있음. 병변의 oral side로는 발적을 동반한 함물부가 있음. 함물부 주변에는 점막주름이 끌려오는 소견이 관찰됨.
내시경 진단 (impression): Advanced colon cancer, type III
[이준행 comment]
이 병소를 fungating이라고 표현하신 분이 계시는데, fungating은 너무 지저분한 느낌이 나기 때문에 사용을 피하도록 권합니다. 자세한 내용은 EndoTODAY 내시경 용어 - fungating을 참고하시기 바랍니다.
수술을 시행하였고 아래의 결과였습니다.
Ascending colon, cecum, appendix, and terminal ileum, right hemicolectomy:
Adenocarcinoma, moderately differentiated
1. Location: ascending colon
2. Gross type: ulcerofungating
3. Size: 2.7x2.5 cm
4. Depth of invasion: invades muscularis propria(pT2)
5. Resection margin: free from carcinoma: safety margin: proximal, 6 cm ; distal, 25 cm ; radial, > 10.0 mm
6. Regional lymph node metastasis : no metastasis in all 24 regional lymph nodes(pN0)
7. Lymphatic invasion: not identified
8. Venous invasion: not identified
9. Perineural invasion: not identified
10. Tumor budding : positive (>=10)
11. Pathologic staging: pT2 N0 Mx또 다른 증례를 소개합니다.
Colon, anterior resection : Adenocarcinoma, moderately differentiated
1. Location: sigmoid colon
2. Gross type: ulceroinfiltrative
3. Size: 4.8x3.7 cm
4. Depth of invasion: invades pericolic adipose tissue(pT3)
5. Resection margin: free from carcinoma, safety margin: proximal, 4 cm ; distal, 7 cm ; circumferential, > 10 mm
6. Regional lymph node metastasis : Metastasis to 2 out of 18 regional lymph nodes(pN1b) (2/18: pericolic, 2/18), Number of Extramural Tumor Deposits: 1
7. Lymphatic invasion: present
8. Venous invasion: not identified
9. Perineural invasion: not identified
10. Tumor budding : positive (5-9)
11. Micropapillary component: no
12. Tumor border: infiltrative
13. Pathologic staging: pT3 N1b
소견 (findings): Rectum에 5cm 이상 크기의 내강 절반 이상을 encircling하는 mass with deep ulceration이 관찰됨. 표면에서는 dirty exudates, 불규칙한 발적 및 궤양, spontaneous bleeding 이 관찰됨.
내시경 진단 (impression): Advanced rectal cancer, type III
[이준행 comment]
종양성 병소는 아무리 커도 크기를 cm로 써 주는 습관을 가집시다. 예를 들어 ' 5cm 이상의 mass' 정도면 좋을 것 같습니다. 보만 4형 진행성 위암에서도 크기를 써 달라는 것도 같은 이유입니다. 보만 4형 진행성 위암이고 크기 짐작이 되지 않으면 10cm 라고 쓰도록 권한 것처럼...
2005년 환자였습니다. RT 후 수술을 시행하였습니다. 요즘 같아서는 chemoRT 후 수술을 했겠지요. 여하튼 수술은 잘 되었고 10년 이상 재발 없이 잘 지내고 계십니다.
Rectum, low anterior resection:
. Status concurrent radiotherapy
. Ulcerative carcinoma,
. Mucinous adenocarcinoma;
1) tumor size: 4.2x2.5 cm
2) extension to pericolic adipose tissue
3) endolymphatic tumor emboli: not identified
4) perineural invasion: not identified
5) negative resection margins (nearest, 2.2 cm; opposite, 8 cm; radial, 1.6 cm)
6) no metastasis in 3 perirectal lymph nodes (0/3)
 Case 46. Diarrhea. Sigmoid colon
Case 46. Diarrhea. Sigmoid colon
소견 (findings): 대장점막에 경계가 명확하고 약간 융기된 2-5mm 크기의 yellow plaque들이 관찰되며 주변점막은 비교적 정상이거나 edematous 합니다.
내시경 진단 (impression): Pseudomembranous colitis
[이준행 comment]
크기 언급을 안 하신 분들이 많았습니다. 가능하면 늘 크기와 내시경 분류를 쓰는 연습을 해 봅시다.
똥색이라고 쓰지는 마세요.^^ 똥색 맞기는 하지만...
Yellow plaque라는 표현이 좋을 것 같습니다. Plaque는 약간 융기된 병소, patch는 flat한 병소를 부르는 용어입니다.
2026년 2월 어떤 선생님의 답변 (주소견 : multiple white patches, 부소견 : 크기가 1-2mm 정도로 비교적 균일하며 전반적으로 산재되어 있다. 융합되어 보이는것도 있으며, 건드리면 떨어질 것 같다. 진단 : Pseudomembraneous colitis)에 아래와 같은 comment를 보냈습니다.
"(1) Patch는 크고 flat 한 것을 말하므로 부적절합니다. 작고 약간 융기되었으므로 papule이나 plaque가 좋습니다. 크기 기준으로 papule이 맞는데 plaque라고 쓰는 관행이 있습니다.
(2) Pseudomembraneous colitis → Pseudomembranous colitis. 즉 'e'가 없습니다. 철자법 주의!"
* 참고: EndoTODAY pseudomembranous colitis (CDI)
 Case 47. Massive hematochezia (multiple myeloma로 치료받던 환자임)
Case 47. Massive hematochezia (multiple myeloma로 치료받던 환자임)
소견 (findings): 하행결장에 점막의 심한 발적과 취약성과 함께 점막하 출혈 및 혈종이 관찰되며 심한 부종이 동반되어있음. 중간중간 삼출물과 표재성 궤양이 있음. 직장 점막은 정상으로 관찰됨.
내시경 진단 (impression): Ischemic colitis
소견 (findings): 직장에 약 5mm 크기의 정상 상피로 덮힌 노란색의 dome-like 융기형 병소가 관찰됨.
내시경 진단 (impression): Rectal SMT (r/o carcinoid tumor)
[이준행 comment]
초보자들은 그냥 polyp이라고 답하는 경우가 많았습니다. Polyp도 틀린 표현은 아니지만, 표면이 맨들맨들하고, 투명한 느낌이고, 약간 노랗게 비치고 있으므로 SMT로 답하는 것이 더 좋겠습니다.
EMR을 시행하였고 점막과 점막하층의 carcinoid tumr (well-differentiated neuroendocrine tumor)로 확인되었습니다.
* 참고: EndoTODAY 직장 유암종
소견 (findings): 대장점막에 무수히 많은 다양한 크기의 용종들이 관찰됩니다.
내시경 진단 (impression): Familial adenomatous polyposis
* 참고: EndoTODAY FAP
[2016-11-23. 홍성노 교수님께 드리는 질문]
1) 언제 LST라는 용어를 쓰고, 언제 Is라고 써야 할까요? 구분의 기준은 무엇입니까? LST의 정의가 궁금합니다.
2) 진행성 식도암, 진행성 위암, 진행성 대장암 모두 내시경 분류는 Borrmann type을 적용하도록 가르치고 있습니다. 파리 분류 (Paris classification)에서도 Borrmann type을 준용하고 있으니까요. 그런데 '진단: Colon cancer, Borrmann type II'와 같이 썼더니 영 어색하기는 합니다. 진행성 대장암 분류를 위한 더 좋은 방법은 없을까요?
[2016-11-25. 홍성노 교수님 답변]
질문 1에 대한 답변:
의학 용어는 의료진간 communication을 원할하게 하는 목적이 큽니다만, 임상적인 특징(발생 병태생리, 진단, 치료의 방침과 예후 등)을 반영하기도 합니다.
파리 분류는 동서양의 다양한 표현을 통일하기 위해서 advanced cancer의 경우는 Borrmann 분류, superficial tumor의 경우는 Yamada 분류, 일본 EGC 분류, 일본 early colorectal tumor 분류 등을 적절히 혼합하여 전문가들의 consensus를 이룬 것입니다. Type 0, 1, 2, 3, 4, 5로 나누고 type 0은 아래와 같이 세분하고 있습니다. 실제로 형태학적 communication에 촛점을 맞춘다면 파리 분류가 가장 정확한 분류라고 생각됩니다.
하지만, 내시경의 해상도가 좋아지고 표재성 병변의 진단율이 높아졌습니다. 일본에서는 구도 선생님 등에 의하여 과거의 저해상도 내시경으로 발견이 어려웠던 depressive type 병변이 polypoid 병변보다 악성화 위험성이 높음을 알게 되었습니다. 또한 superficial speading type에 대한 ESD가 가능해지면서 형태에 따라 치료법이 달라지게 되었습니다. 즉 임상적인 특징을 반영하는 표현이 중요하게 되었습니다.
병태 생리, 심달도, 예후 등을 예측하고 적절한 치료 방침을 세울 수 있기 때문에 일정한 형태학적 특징을 가진 병소는 LST라는 별도의 이름으로 부르고 이를 더욱 세분하는 것입니다 (LST를 granular type과 non-granular type으로 분류하고 homogenous type, nodular mixed type / flat elevated type, pseudo-depressed type으로 세분하고 있습니다). Laterally spreading tumor (LST)는 10mm가 넘으면서 측방으로 발육성장을 위주로 하는 superficial lesion을 말합니다. Width가 height보다 넓은 경우를 말하는데 정확하게 얼마나 넓어야 하는지 의견은 다양합니다. Width가 height보다 수배는 길어야 한다는 것부터 넓기만 하면 된다는 등 다양한 의견이 있습니다.
파리 분류는 치료 내시경이 활발한 국내에서는 잘 정착되지 않는 것 같습니다. 우리병원 stomach 파트에서도 Borrmann type, EGC type등을 사용하는 것으로 알고 있습니다. 파리 분류가 아닌 듯 합니다.
질문 2에 대한 답변:
진행성 대장암의 type을 써야 한다면 파리 분류 type 1, 2, 3, 4라고 하면 될 것 같습니다. 저라면 그냥 colorectal cancer, polypoid type, ulcerative type, ulceroinfiltrave type, diffuse infiltrative type 이라고 하겠습니다.
[2016-11-25. 이준행 답변]
자세한 답변 감사합니다. Pure하게 접근하면 파리 분류가 가장 깔끔하지만, 임상적 유용성을 고려하면 LST라는 용어를 함께 사용하는 것이 좋다는 정도로 이해됩니다.
1. 형태학적으로 가장 명료한 분류인 파리 분류 혹은 일본 분류를 기본으로 하되 LST의 전형적인 특징을 보이는 경우는 LST라고 붙이는 것으로 정리하겠습니다. 결국 원래 우리 병원에서 사용하던 아래의 표를 그대로 쓰는 셈입니다.
2. Advanced colorectal cancer는 Borrmann type I으로 쓰면 어색하므로 그냥 'type 3'와 같이 쓰던지 아니면 'ulceroinfiltrative type'과 같이 쓰도록 정리하겠습니다.
* 참고: EndoTODAY 진행성 대장암 내시경 분류
 [2018-1-7. 3월부터 fellow 생활을 시작하시는 한 선생님의 7회 description exercise에 대한 답변]
[2018-1-7. 3월부터 fellow 생활을 시작하시는 한 선생님의 7회 description exercise에 대한 답변]
XXX 선생님.
답변 잘 받았습니다. 고민한 흔적이 느껴져 반가웠습니다. ‘과연 반이나 맞았을지 자신이 없다’고 하셨지만 진단은 다 맞았습니다. 100점. 내시경실 근무에 앞서 내시경으로 진단할 수 있는 여러 질병을 배우고 익히자는 저의 생각을 따라주셔서 감사합니다. 저는 '내시경 선행학습주의자’입니다. 미리 공부한 후 내시경을 잡아야 합니다. 공부와 훈련을 하지 않고 내시경 시술을 하는 것은 환자에 대한 부도덕한 행위라고 생각합니다.
대장 질환이 어려운 것은 당연합니다. 처음 배우는 것 아닙니까. 이 또한 배우고 익히다보면 위내시경과 비슷해집니다. 저는 위내시경이 더 어렵다고 생각합니다. 대장내시경을 하면 크고 중요한 질병은 대강 발견할 수 있는데, 위내시경은 종종 심각한 질병도 놓치기 때문입니다. 내시경을 배운지 올해로 26년이지만 저는 여전히 보만 4형 진행성 위암을 놓칠까 늘 걱정합니다. 특히 잔위의 보만 4형 진행성 위암은 매우 두렵습니다.
지금까지 내시경 기술법 연습을 통하여 병소를 묘사하는 실력이 상당히 좋아졌습니다. 대장내시경은 사진만으로 어딘지 정확히 알기 어렵습니다. 답변을 보니 위치를 너무 자세히 쓰려고 노력한 나머지 다소 부자연스럽게 느껴진 부분이 있었습니다. 過猶不及.
43번. 조기 직장암은 맞고 IIa+IIc라고 쓴 것도 타당합니다. 그러나 높이에 비하여 상당히 넓은 이런 병소-빈대떡같다고 할까요?-는 LST(laterally spreading tumor)라는 보다 specific한 이름이 있습니다. LST에 대하여 공부해보세요.
44번. Fungating이라는 표현은 원래 ‘곰팡이같은’이라는 뜻이므로 가급적 쓰지 말도록 권하고 있습니다 (EndoTODAY Fungating). 기존의 내시경 책에서 fungating이라는 쓰인 질환은 대부분 large polypoid라고 바꿔도 좋습니다. 진행성 대장암도 보만 분류를 붙입니다만, 구태여 보만 3형이라고 쓰면 다소 어색합니다. 그냥 ‘진행성 대장암, 3형’이라고 진단하는 것이 자연스럽습니다. 식도암도 마찬가지입니다. (이준행 style?)
46번. Papule이라는 표현에 대하여 고민해봅시다. 맞습니다. 내시경 용어의 뿌리인 피부과 자료에는 papule을 "circumscribed elevation of skin which are palpable with no visible fluid and diameter is less than 5 mm or upto 10 mm in diameter at the widest point”로 설명하고 있으니 분명히 맞는 표현입니다. 피부과에서는 0.5-1cm이하의 융기는 papule, 그 이상은 plaque 맞습니다. 그러나 내시경 영역에서는 크기 기준을 이보다 낮추는 경향입니다. 딱히 정해진 것은 없습니다. 아마도 내시경 자체가 확대 영상을 보는 것이기 때문인 것 같습니다. 다른 측면도 있습니다. 오랜 관행같은 것 말입니다. Candida esophagitis와 pseudomembranous colitis의 소견은 plaque로 표현하는 관행이 있습니다. 내시경 기술법을 처음 배울 때, 소견을 자세히 쓰고 그에 근거하여 내시경 진단을 붙인다고 들으셨을 것입니다. 그러나 전문가 영역에서는 소견과 진단이 서로 영향을 줍니다. 딱 보고 pseudomembranous colitis면 소견도 그에 어울리는 용어를 사용하는 것이 자연스럽습니다. 이는 모든 전문 영역에서 나타나는 현상입니다.
49번. 수백여개 --> 수백개
 [2026-1-31. 3월부터 fellow 생활을 시작할 선생님의 quiz 답변에 대한 comment]
[2026-1-31. 3월부터 fellow 생활을 시작할 선생님의 quiz 답변에 대한 comment]
43. 좋습니다. wide, flat elevated lesion with central depression 표현 중 wide는 그 의미가 명확하지 않아서 차라리 빼는 것이 어떨까요?
44. Fungating이라는 표현에 대한 의견은 다양합니다. SMC에서는 잘 쓰지 않고 있습니다. http://endotoday.com/endotoday/terminology_fungating.html
44, 45. 위암과 비슷하게 1,2,3,4형을 붙이는 것은 좋은데 Borrmann은 빼기 바랍니다. 빼는 것이 관행입니다. Borrmann은 위(胃)에서는 붙이고 다른 곳에서는 뺀다.
46. PMC. 좋습니다. 그런데 내시경 결과는 소화기내과 의사만 보는 것이 아니므로 가급적 impression에 약자를 쓰지 말기 바랍니다. 간호사도 보고 학생도 보고 경우에 따라서는 일반인도 보기 때문입니다. EGC, AGC, FAP 정도만 약자로 쓰고 다른 약자는 피하는 것이 무방합니다.
47. Amyloidosis도 가능한데 일부만 침범하고 일부는 침범하지 않은데 주목해 보세요.
 [2025 EndoTODAY On-line seminar]
[2025 EndoTODAY On-line seminar]
2025년도에는 기록적으로 많은 온라인세미나를 진행하였습니다. 2026년도부터는 대학보직을 하게 되어 weekly seminar를 할 수 없어 저도 안타깝게 생각하고 있습니다.
 2025-83. Gastric cancer/adenoma and ischemic heart disease
2025-83. Gastric cancer/adenoma and ischemic heart disease
 2025-81. Diffuse large B cell lymphoma. Candida in biopsy. Various GI lymphomas.
2025-81. Diffuse large B cell lymphoma. Candida in biopsy. Various GI lymphomas.
 2025-80. Learning ESD skills and interpreting the outcome. ESD workshop at Taiwan.
2025-80. Learning ESD skills and interpreting the outcome. ESD workshop at Taiwan.
 2025-78. AGC staging. Mucosal cancer with lymphatic invasion. NSAIDs-associated ulcer
2025-78. AGC staging. Mucosal cancer with lymphatic invasion. NSAIDs-associated ulcer
 2025-77. 이런저런 6. SMT-like cancer. MALToma. Esophageal foreign body
2025-77. 이런저런 6. SMT-like cancer. MALToma. Esophageal foreign body
 2025-76. 은퇴하신 교수님을 좌장으로 모시고 세미나를 진행하였습니다.
2025-76. 은퇴하신 교수님을 좌장으로 모시고 세미나를 진행하였습니다.
 2025-75. D-DDW. GERD and gastritis. 4814명이 함께 해 주셨습니다. 기록입니다. 감사합니다.
2025-75. D-DDW. GERD and gastritis. 4814명이 함께 해 주셨습니다. 기록입니다. 감사합니다.
 2025-74. 答釜山質問. 제23회 부산시내과의사회 종합연수강좌에서 나왔던 질문에 답합니다.
2025-74. 答釜山質問. 제23회 부산시내과의사회 종합연수강좌에서 나왔던 질문에 답합니다.
 2025-73. Two cases of gastric cancers
2025-73. Two cases of gastric cancers
 2025-72. 이런저런 5. (1) Cardia cancer (2) BGU bleeding, (3) Gastric inverted hamartomatous polyp
2025-72. 이런저런 5. (1) Cardia cancer (2) BGU bleeding, (3) Gastric inverted hamartomatous polyp
 2025-71. (1) 조직검사 점막하침윤. submucosal invasion in forceps biopsy (2) 점막하암에 대한 ESD. ESD for suspected submucosal cancer
2025-71. (1) 조직검사 점막하침윤. submucosal invasion in forceps biopsy (2) 점막하암에 대한 ESD. ESD for suspected submucosal cancer
 2025-70. 내시경 증례를 통해 확인하는 알쏭달쏭 Q&A
2025-70. 내시경 증례를 통해 확인하는 알쏭달쏭 Q&A
 2025-69. Kolkata Apollo 병원 강의. Endoscopic treatment of early gastric cancer in Korea (우리말 요약)
2025-69. Kolkata Apollo 병원 강의. Endoscopic treatment of early gastric cancer in Korea (우리말 요약)
 2025-68. 이런저런 4. 위암 5 증례 (Kolkata 녹화)
2025-68. 이런저런 4. 위암 5 증례 (Kolkata 녹화)
 2025-67. 이런저런 3. (1) 식도암 수술 후 소견 (2) 항암치료가 필요합니까 (3) 소장 림프종.
2025-67. 이런저런 3. (1) 식도암 수술 후 소견 (2) 항암치료가 필요합니까 (3) 소장 림프종.
 2025-66. 이런저런 2. (1) 위 SET와 GIST (2)아스피린 사용자의 hematin (3) 저도선종.
2025-66. 이런저런 2. (1) 위 SET와 GIST (2)아스피린 사용자의 hematin (3) 저도선종.
댓글: 저런 엉터리 검사를 비싼돈 내고 받아야하는 미국인들이 안타까운건지, 위암 선진국형의 검사를 하면서도 시간과 수가에 쫓겨야 하는 한국 의사들이 안타까운건지 생각이 많아집니다.. 유익한 강의, 늘 감사드립니다.
 [2025-9-5] SMC ESD Training Week 기간입니다. ESD seminar, ex vivo pig stomach ESD, ESD pathology conference, ESD bookreading, live pig ESD를 짧은 기간에 집중적으로 진행하고 있습니다. 한 신문사에서 seminar 현장 리포트를 하였습니다. 교육을 통한 질향상. 저의 신념입니다.
[2025-9-5] SMC ESD Training Week 기간입니다. ESD seminar, ex vivo pig stomach ESD, ESD pathology conference, ESD bookreading, live pig ESD를 짧은 기간에 집중적으로 진행하고 있습니다. 한 신문사에서 seminar 현장 리포트를 하였습니다. 교육을 통한 질향상. 저의 신념입니다.
지난 2000년 국내 도입된 내시경 점막하 박리술(endoscopic submucosal dissection, ESD)은 조기위암 치료에 있어 환자 삶의 질을 완벽하게 보존하는 최소 침습적 치료법으로 평가받고 있다. 국내 인구 중 매년 2만 5000명~3만명이 위암으로 진단받고 있는 가운데, 진단 환자 중 95%는 수술 및 ESD를 통해 조기 치료가 가능하다. 95%의 환자 중 2/3는 위암 절제술를 통한 치료가 이뤄지고, 1/3이상은 ESD가 시행되고 있다. 특히 조기위암의 경우 내시경으로 최소침습을 통한 병소만 타깃해 치료하기 때문에 환자 신체에 부담이 덜하다는 장점이 있어 조기위암 치료의 대표적 치료법으로 자리매김했다. 하지만, 국내 의료현장은 ESD를 제대로 수련받는 곳이 많지 않은 실정이다.
어깨 너머로 배우는 수련 현장, 제대로된 수련 프로그램 필요
삼성서울병원 소화기내과 이준행 교수는 ESD를 통한 조기위암 치료 수련 프로그램을 개발, 후학 양성에 힘쓰고 있다. 이 교수가 개발한 ESD 교육 프로그램은 3단계로 진행된다. 매년 교육 프로그램을 진행하고 있지만, 특히 봄, 여름, 가을에 집중적으로 교육하는 기간이 있다. 그 집중적인 교육 프로그램이 ‘SMC ESD Training week’다. 핸즈온 트레이닝, 북리딩 및 저널리뷰 세미나, 증례 토의 등 3가지가 삼성서울병원이 갖춘 ESD 트레이닝 시스템이다. 첫번째는 핸즈온 트레이닝, 두번째는 교과서 및 저널 리뷰를 통한 세미나, 세번째는 실제 임상현장에서 발생하는 증례 토의로, 술기와 지식, 실제 임상 대응 역량을 함양하는 3단계 프로그램이라는 것이다. 핸즈온 Training은 엔도젤이라는 인공 위점막을 이용해 훈련하는 EndoGEL ESD, 절제된 돼지 위를 이용하는 Ex vivo pig stomach ESD, 살아 있는 돼지를 이용한 훈련인 Live pig ESD, 그리고 Real patient ESD 등 단계적 과정으로 구성돼 있다. 이 교수는 “ESD 교육에서 증례 토의를 가장 중요하게 생각한다”며 “하지만, 증례 토의는 환자 개인정보 보호를 위해 온라인으로 교육할 수 없다. 현장 교육으로만 가능하다”며 “가감없는 임상현장의 증례를 통해 ESD 시술 시 순간순간 어떤 판단으로 환자를 치료했는지, 합병증은 없었는지, 치료 후 결과를 어떻게 해석하고 추가 치료 여부를 어떻게 결정했는지 등 리얼하게 토론하는 것이 중요하다”고 강조했다.
이준행 교수는 “한국의 교육 시스템은 국민의 눈높이에 맞지 않은 부실한 교육이 이뤄지고 있다”며 “의과대학 역시 의대생들이 의사국가고시 합격을 위해 학원을 다니는 실정”이라고 전했다. 이어, “교육이 부실하면 훌륭한 인재를 양성할 수 없고, 결국 그 피해는 국민에게 돌아간다”며 “의학교육은 매우 중요하다. 자본주의 표본이라는 미국조차도 전공의 교육과 응급의료체계, 중증진료체계를 유지하기 위해 정부가 공적 자금을 투입하고 있다”고 한국 의학교육의 현실을 비판했다. 국내 의학교육은 레지던트 과정에서 술기를 배우고, 부족한 것은 팰로우를 거치면서 배운다. 팰로우 이후부터는 진료현장에서 환자를 진료하면서 배운다. 이 교수는 “지금 제가 위암 내시경 진단 및 치료를 40년째 하고 있지만, 제가 하는 진료의 90%는 10년 내 배운 것들”이라며 “의대생부터 30년간 배웠던 내용은 다소 시대에 뒤떨어진 것들이 많다”고 말했다. 즉 의료현장은 끊임없이 새로운 술기와 지식을 배워야만 최신 진료를 할 수 있다는 것이다. 그는 “새로운 술기와 지식을 배우기 위한 과정은 매우 어렵다”며 “그 이유는 교육 시스템이 없기 때문”이라고 토로했다.
의대교수, 후학 교육,평점 없이 불이익만 받아 교육 부실 원인
전공의와 팰로우들은 소속기관에서만 술기와 지식을 배울 수밖에 없는 상황이다.질 좋은 교육 프로그램이 제공되지 않으면 3, 4년 수련기간이 지나도 헛발질에 불과하다는 것이 이 교수의 지론이다. 그는 “수련과정을 거쳤는데도 배운 것이 없다. 최근에는 외과 전문의가 됐지만 개복술을 잘 못한다는 이야기도 있다”고 씁쓸한 웃음을 보였다. 이준행 교수는 교수들의 전공의 및 팰로우 교육이 부실해지는 원인을 왜곡된 정책과 제도에서 찾았다. 이 교수는 “현재 제도에서는 교수들이 교육을 열심히 한다고 해서 보상이 주어지지 않는다. 오히려 불이익을 받게 된다”며 “교육과 연구, 진료를 잘해야 훌륭한 의사로 인정받지만, 교육을 열심히 하게 되면 연구 성과와 진료량이 낮아질 수밖에 없다. 하지만 병원과 사회는 교육의 중요성을 인정하지 않고 있다”고 토로했다. 특히 의대교수들의 교육행위에 대한 평점 부여가 이뤄지지 않아 제대로된 평가를 받지 못하고 있다는 것이다.
이런 상황에서 이준행 교수는 자신이라도 제대로된 교육 시스템을 개발해야겠다는 마음을 먹었다는 것. 그는 “1999년 인터넷이 처음 도입됐을 때부터 천리안 시스템을 이용해 개인 홈페이지를 개설, 26년째 꾸준히 의학교육 관련 포스팅을 하고 있다”며 “수 년 전부터는 저술 작업도 하고 있지만 쉽지 않다”고 말했다. 이 교수는 ESD가 국내에 도입된지 20년이 넘어가지만, 국내 어디에도 체계적으로 ESD를 배울 수 있는 시스템을 찾기 어렵다며, 체계적인 수련 코스가 필요하다는 생각에 SMC ESD Training Week를 개발, 운영하고 있다고 강조했다. 이준행 교수는 2일 삼성서울병원 암병원 내시경실 회의실에서 'SMC ESD Training Week 2025, ESD seminar'를 진행했다.
SMC ESD Training Week 2025, ESD seminar 진행
한편, 이준행 교수는 지난 2일 삼성서울병원 내시경실 회의실에서 SMC ESD Training Week 2025 첫 교육 프로그램인 교과서와 저널을 리뷰하는 ESD seminar을 진행했다. 이날 프로그램은 △ESD for EGC with undifferentiated type histology(조직학적 미분화 조기위암에서 ESD, 이형석 임상강사) △ESD in high risk patients(고위험 환자에 대한 ESD, 김지연 임상강사) △Indications of additonal surgery after ESD(ESD 이후 추가 수술 적응증) △ESD for EGC with uncommon pathology(흔하지 않은 병리를 가진 조기위암에서 ESD, 김태세 교수) 발표와 토의가 진행됐다. 조직학적 미분화 조기위암에서 ESD 주제를 발표한 이형석 임상강사는 ESD를 시행할 수 있는 조건으로 병소 크기가 2cm 이하일 때, 점막암일 때, 궤양이 없을 때 가능하다고 설명했다. 하지만, 이준행 교수는 병소 크기를 2cm보다 더 엄격하게 적용해야 한다며, 1cm~1.5cm 이하일 때 ESD를 시행하는 것이 안전하다고 의견을 제시했다. 이 교수는 또, “undifferentiated type histology EGC의 내시경 치료는 아직도 매우 조심스럽게 진행돼야 한다고 생각한다”며 “아주 조금이라도 마음에 걸리는 요소가 있으면 현재의 표준치료인 수술을 권하는 것이 맞다고 생각한다”고 강조했다. 김지영 임상강사는 고령환자와 심장질환·당뇨·고혈압·뇌혈관질환 등 기저질환을 가진 고위험 환자들의 조기위암 치료를 위한 ESD 시술을 발표했다. 김 임상강사 발표 후 이 교수는 고위험 환자들은 크고 작은 합병증이 발생할 수 있어 합병증 예방을 위한 방법과 합병증이 발생했을 때 최대한 신속하게 치료하는 방안을 가지고 있어야 한다고 강조했다.
후학 교육이 사명이라고 말하는 이준행 교수는 “교육은 봉사”라며 “후배들에게 좋은 정보와 교육 기회를 제공함으로써 국민들이 훌륭한 의사들로부터 질 좋은 의료서비스를 받도록 기여하는 것이 보람”이라고 역설했다.
 2025-65. 이런저런 1. (1) 식도암, (2) Tube 암, (3) 날문 용종, (4) 폐암 대장 전이, (5) 아메바 장염
2025-65. 이런저런 1. (1) 식도암, (2) Tube 암, (3) 날문 용종, (4) 폐암 대장 전이, (5) 아메바 장염
 2025-64. Autoimmune gastritis and gastric cancer
2025-64. Autoimmune gastritis and gastric cancer
Abstract: As Helicobacter seropositive rate is decreasing in Korea, interests in Helicobacter pylori negative gastric cancer is increasing. Autoimmune gastritis is a non-self-limiting, chronic inflammatory disorder of the stomach. There has been a controversy in the relationship between autoimmune gastritis and gastric adenocarcinoma. Gastric cancers in AIG is often found in older individuals. Tumors are located in the upper body and greater curvature, and the rate of synchronous and metachronous tumors are high. The relationship between autoimmune gastritis and Helicobacter infection is still controversial both in the pathogenesis and in the development of gastric neoplasms. It is not clear wheter it triggers or inhibits gastric carcinogenesis. Our team at Samsung Medical Center evaluated the incidence of autoimmune gastritis in Korean patients with gastric cancers. Parietal cell antibody was tested in 612 consecutive patients with gastric cancer. Among them, 5.5% tested positive for anti-parietal cell antibody. Helicobacter serology positive rate was not different between parietal cell antibody negative and positive groups. Seventy eight versus seventy five. In PCA positive groups, pepsinogen 1 level was lower and serum gastrin was higher. Eight cases were classified as AIG group by our definition. Five out of eight were female. Helicobacter serology positive rate was not different between two groups. Pepsinogen 1 and 1:2 ratio was significantly lower in AIG group. In 6 out of 8 gastric cancers with AIG, helicobacter serology was positive. In the remaining 2 cases, both Helicobacter serology and histology were negative. Without Helicobacter infection, the risk of gastric cancer is lower than previously thought. However, it is too early to exclude AIG from risk factors for Helicobacter-negative gastric cancer. In some recent studies, there is an unexpected finding that Helicobacter infection may decrease gastric cancer in AIG patients. Further data from prospective studies in different populations are strongly required.
 2025-62. Gastric adenoma in autoimmune gastritis
2025-62. Gastric adenoma in autoimmune gastritis
 2025-61. (1) Aspirin 관련 출혈 환자의 장기 유지요법, (2) 위 MALT 림프종 (3) AMI 환자의 조기위암 내시경치료
2025-61. (1) Aspirin 관련 출혈 환자의 장기 유지요법, (2) 위 MALT 림프종 (3) AMI 환자의 조기위암 내시경치료
 2025-60. 위암 5 증례 토의 (2). BGU 후 AGC. LELC. Pyloric ring cancer
2025-60. 위암 5 증례 토의 (2). BGU 후 AGC. LELC. Pyloric ring cancer
 2025-59. 대장암과 구분이 어려운 게실염. Acute diverticulitis mimicking colonic neoplasm
2025-59. 대장암과 구분이 어려운 게실염. Acute diverticulitis mimicking colonic neoplasm
 2025-57. 내시경 5 증례 토의. 1. FBFB in vallecula, 2. Biopsy negative gastric cancer, 3. Appendix mucocele, 4. Gastric recurrence of small bowel DLBCL, 5. Appendiceal metastasis from gastric cancer
2025-57. 내시경 5 증례 토의. 1. FBFB in vallecula, 2. Biopsy negative gastric cancer, 3. Appendix mucocele, 4. Gastric recurrence of small bowel DLBCL, 5. Appendiceal metastasis from gastric cancer
 2025-56. 헬리코박터 제균치료 comment (Journal club)
2025-56. 헬리코박터 제균치료 comment (Journal club)
 2025-54. 점막하종양과 유사한 위암. SMT-like cancer
2025-54. 점막하종양과 유사한 위암. SMT-like cancer
 2025-53. 식도암 수술 후 gastric tube 위선종/위암의 내시경치료 ESD for gastric tube neoplasms
2025-53. 식도암 수술 후 gastric tube 위선종/위암의 내시경치료 ESD for gastric tube neoplasms
 2025-52. AMI로 PCI 후 지혈술 하였던 환자의 조직검사는 언제 하는 것이 좋을까요?
2025-52. AMI로 PCI 후 지혈술 하였던 환자의 조직검사는 언제 하는 것이 좋을까요?
 2025-50. 잘 낫지 않는 궤양. MALT 림프종 의증으로 의뢰된 진행성 위암. Lymphoepithelioma-like carcinoma (LELC). Adenocarcinoma with lymphoid stroma
2025-50. 잘 낫지 않는 궤양. MALT 림프종 의증으로 의뢰된 진행성 위암. Lymphoepithelioma-like carcinoma (LELC). Adenocarcinoma with lymphoid stroma
 2025-49. 소화기 내시경의 이해 (2025) - 학생 강의
2025-49. 소화기 내시경의 이해 (2025) - 학생 강의
 2025-48. 위염과 위궤양 (2025) - 학생 강의
2025-48. 위염과 위궤양 (2025) - 학생 강의
 2025-46. Obstruction 증상으로 생애 첫 내시경에서 발견된 진행성 위암
2025-46. Obstruction 증상으로 생애 첫 내시경에서 발견된 진행성 위암
 2025-45. 직장경 두 증례. Right-sided colon cancer with hepatic metastasis. Neuroendocrine tumor with lymph node metastasis
2025-45. 직장경 두 증례. Right-sided colon cancer with hepatic metastasis. Neuroendocrine tumor with lymph node metastasis
 2025-43. ulcer, ulceration, ulcer finging
2025-43. ulcer, ulceration, ulcer finging
마지막장 두번째 줄을 "얕은 ulcer는 점막암일 가능성이 있으므로 ESD를 시도한다."로 정리합니다. 혼선을 드려서 죄송합니다.
Ulcer finding은 연구마다 그 빈도가 다릅니다. 판정 기준이 다르다는 이야기입니다.
 2025-42. 학회 사진사께서 오래된 동영상 clip을 보내주셨습니다. Paraesophaeal hernia는 mixed type이다.
2025-42. 학회 사진사께서 오래된 동영상 clip을 보내주셨습니다. Paraesophaeal hernia는 mixed type이다.
 2025-41. 학회 사진사께서 오래된 동영상 clip을 보내주셨습니다. Fasciola hepatica 약이 없었던 시대가 있었습니다. 소가 먹는 약만 있고 사람이 먹는 약이 없다?
2025-41. 학회 사진사께서 오래된 동영상 clip을 보내주셨습니다. Fasciola hepatica 약이 없었던 시대가 있었습니다. 소가 먹는 약만 있고 사람이 먹는 약이 없다?
 2025-38. 내시경 증례를 통해 확인하는 속 시원~한 Q and A. 이준행, 이선영, 김태세
2025-38. 내시경 증례를 통해 확인하는 속 시원~한 Q and A. 이준행, 이선영, 김태세
 2025-35. 식도 위 정맥류 출혈. White nipple sign. Hypopharyngeal perforation due to overtube
2025-35. 식도 위 정맥류 출혈. White nipple sign. Hypopharyngeal perforation due to overtube
 2025-33. Endoscopic staging of gastric cancer. IGCC2025. Amsterdam
2025-33. Endoscopic staging of gastric cancer. IGCC2025. Amsterdam

2025-5-8. Subnote
 2025-32. (1) EGC-like AGC, (2) Duodenal MALToma, (3) 훌륭한 의뢰서
2025-32. (1) EGC-like AGC, (2) Duodenal MALToma, (3) 훌륭한 의뢰서
 2025-31. ESD complications. 오영은/이준행
2025-31. ESD complications. 오영은/이준행
 2025-30. (1) MALToma 의증, (2) 날문 위암
2025-30. (1) MALToma 의증, (2) 날문 위암
 2025-27. 조기위암 내시경치료, 미분화조직형 위암의 치료법 선택, BGU 토혈, 아메바 장염 등
2025-27. 조기위암 내시경치료, 미분화조직형 위암의 치료법 선택, BGU 토혈, 아메바 장염 등
 2025-25. Bowel preparation. 김민지
2025-25. Bowel preparation. 김민지
 2025-24. Cardia EGC with SM invasion and gastritis cystica profunda (Cancer 724/ECR 035)
2025-24. Cardia EGC with SM invasion and gastritis cystica profunda (Cancer 724/ECR 035)
 2025-23. 진행성 위암 증례 토의. 매우 아나로그한 결과지
2025-23. 진행성 위암 증례 토의. 매우 아나로그한 결과지
 2025-22. Sentinel polyp. 보초용종 (EndoTODAY 보초 용종)
2025-22. Sentinel polyp. 보초용종 (EndoTODAY 보초 용종)
[2025-3-4. 이준행 Facebook 공개 질문] Sentinel polyp이라는 용종이 있는데 이 종류가 왜 보초 용종이라고 불리게 되었는지 저는 알지 못합니다. 알고 계신 분은 저에게 연락주시기 바랍니다.
[2025-3-4. 김용성 원장님 답변] Reflux esophagitis와 연관되어 fold thickening or polyp을 내시경으로 관찰하고 명명했다고 하는데, 왜 그렇게 붙였는지 찾기는 어렵네요. Esophagogram에서 보이는 모양이 보초가 서 있는 것 같기도 하고요. (Abdom Radiol 2021)
ChatGPT의 설명이 더 그럴듯 해보이기도 합니다.^^ "Sentinel polyp 용어의 역사적 유래: 이 용어는 원래 항문(anal fissure)에서 발견되는 sentinel tag(또는 sentinel pile)에서 유래했습니다. 항문 주변에서는 만성적인 균열(anal fissure)이 있으면 항문 가장자리에 보호 반응으로 섬유성 조직(fibrous tissue)이 증식하면서 작은 결절 형태의 병변이 형성되는데, 이를 **sentinel pile(polyp)**이라고 불렀습니다. 이러한 개념이 식도의 만성 손상에서도 비슷한 병리학적 양상이 나타난다는 점에서 식도에서도 sentinel polyp이라는 용어가 적용된 것으로 보입니다."
[2025-3-5. 이준행 답변] 김용성 원장님. 좋은 comment 감사합니다. 아, 그렇구나. AI에 물어봐야지.... 생각이 들어서 저도 제미니에게 물어보았습니다. 이런 답변을 받았습니다. "센티넬 폴립은 만성 치열이나 항문 궤양의 결과로 항문 주변에 나타나는 작은 피부 돌출물입니다. Sentinel이라는 이름은 '보초병'이라는 뜻으로, 이 폴립이 항문 질환의 '보초병' 역할을 한다는 의미에서 붙여졌습니다." 사실 저는 컴맹입니다. 저를 컴퓨터 귀신으로 아는 분도 계시는데 완전히 컴맹입니다. 컴퓨터 분야에서는 도무지 새로운 것을 시도하지 않고 있습니다. 1999년 군의관 시절 동료였던 최진호 군의관 (현 삼성서울병원 응급의학과 교수)로부터 배운 HTML을 아직도 메모장을 이용하여 작성하고 있을 뿐입니다. 그런데 ChatGPT를 이용한 선생님의 답변과 오늘 제미니에게 물어본 저의 경험으로 이제 저도 AI 시대에 맞게 변신해야 할 것 같다는 생각을 하게 됩니다. 은퇴준비에 바쁜 요즈음 (사실 20여년 전부터 은퇴준비를 하고 있습니다만...) AI라는 새로운 흥미거리가 생겼습니다.
[2025-3-5. 김용성 원장님 추가 comment] 이번에 찾아보기 전에 막연하게 염증을 시사하는 indicator라는 의미로 sentinel을 받아들였는데 GTP가 비슷한 답을 줬습니다. 제미니도 동일한 답변을 하는 게 여러가지로 놀랍네요. 동일한 레퍼런스를 어선가 보고 답하는 것이지. 그런 의미에서 pubmed에서 찾은 esophagoram의 이미자와 보초가 서있는 모습의 유사성에 대해서는 AI가 언급을 안해줬다는 것이 특정 전문분야에서 전문가가 나름의 툴을 사용해 검색하는 것은 여전히 추가적인, 혹은 독특한 정보를 찾아낼 수 있는 것 같아서 위안이 되었습니다. AI를 보조적으로 잘 사용하면서 전통적인 검색을 열심히 해야겠다는 생각이 드네요.
[2025-3-6. 애독자 답변] 교수님. 유튜브 영상을 보다가 궁금해서 찾아보았습니다. Sentinel polyp의 어원에 대해서 설명이 잘 되어 있는 것 같아서 교수님께도 공유드립니다. "Just as a sentinel is defined as a “soldier or guard who job is to stand and keep watch” (Fig. 1) and medically as “an indicator of the presence of disease” [4], the sentinel polyp and fold serve as indicators of hyperplastic polyps most commonly caused by gastroesophageal reflux resulting in esophagitis." (Abdominal Radiology 2021;46:2255) 처음 명명 당시에 gastroesophageal reflux와 esophagitis를 나타내는 indicator 처럼 Sentinel polyp이 사용되었던 것 같습니다.
 2025-21. 위선종으로 의뢰된 환자에서 발견된 대장암
2025-21. 위선종으로 의뢰된 환자에서 발견된 대장암
 2025-20. Endoscopic findings of gastric MALToma. 위 MALT 림프종 내시경 소견
2025-20. Endoscopic findings of gastric MALToma. 위 MALT 림프종 내시경 소견
[2025-3-1. 애독자 질문] Polypoid type 으로 소개해 주신 증례 중 세번째 증례는, 위치도 그러하고 varix 와 감별이 어려워서 조직검사를 하기에 망설여졌을 듯 합니다.. 조직검사 전 ct 를 시행해 보는 등의 방법이 도움이 될지요?
[2025-3-2. 이준행 답변] 매우 좋은 질문입니다. 말씀주신 바와 같이 fundus의 융기부는 gastric fundal varix의 가능성을 고려하여 조직검사를 하기 전에 잠시 고민해 보는 것이 좋습니다. Think twice. 간혹 작은 SMT라고 생각하고 조직검사 한 후 대량 출혈을 보인 경우가 있습니다 (모든 SMT를 처음 발견하였을 때 꼭 조직검사를 해야 한다는 것은 과거의 헛된 주장입니다. http://endotoday.com/endotoday/situation.html#biopsy의 상부위장관 점막하종양 부분 참고). 그러나 이 환자에서는 vascular한 특성이 전혀 없었으며 과거보다 점차 자라는 양상으로 볼 때, 간질환의 소견이 전혀 없다는 것을 고려할 때 gastric fundal varix의 가능성은 낮아서 조직검사를 했던 것 같습니다. 조금이라도 gastric varix가 의심되면 혈액검사와 CT를 먼저 해 보는 것은 어떤지 문의하신 내용에 동의합니다.
 2025-19. MALToma. MALT 림프종. 100% 암이라도 듣고 오셨던 환자에 대하여
2025-19. MALToma. MALT 림프종. 100% 암이라도 듣고 오셨던 환자에 대하여
[2025-2-25. 애독자 질문] Maltoma에서 PET CT는 꼭 필요하다고 보시는지요?
[2025-2-25. 이준행 답변] 제 의견은 No입니다. Diffuse large B cell lymphoma에서는 PET 검사를 자주 시행하고 있습니다. 그러나 gastric MALToma에서 PET을 시행하지 않습니다. (1) 필요하지 않습니다. CT로 평가하면 충분합니다. (2) 심평의학에서 PET/CT 검사 시행을 허용하고 있는지 모르겠습니다. 과거에는 CT에서 뭔가 이상 소견이 있으면 추가로 PET/CT를 할 수 있는 것으로 되어 있었습니다. 자꾸 바뀌는 것 같고, 어짜피 필요하지 않아서 현재는 어떻게 되고 있는지 잘 모르겠습니다. 죄송합니다. (3) NCCN 2025년 가이드라인을 다시 찾아보았습니다. CT or PET/CT로 되어 있었습니다. CT를 하면 PET/CT를 할 이유가 없다고 생각됩니다. 요컨데 routine하게 검사하는 것은 권하지 않고 CT 유소견이나 기타 다른 이유가 있을 때에 한하여 selective하게 PET/CT를 하고 있습니다. (사실 거의 하지 않음)
[2025-2-26. YouTube 질문]
교수님께서는 대장내시경 진행 시에도 미다졸람만 사용하시는 건가요? 프로포폴 병합요법 없이..? 그럼 미다졸람+페치딘 사용하시는 걸까요? 미다졸람만 사용하면 환자분 고통 문제가 있지 않아 싶어서요
[2025-2-27. 이준행 답변]
좋은 질문 감사합니다. 저는 대장내시경에서 미다졸람과 페치딘을 함께 사용하고 있습니다. 위내시경에서는 페치딘을 사용하지 않는 경우도 많지만 대장내시경에서는 아무래도 통증 우려가 있어서 대부분 페치딘을 사용하고 있습니다.
여러 의료 환경에서 위내시경이나 대장내시경 과정에서 프로포폴이 유용하게 사용되고 있는 것은 잘 알고 있습니다. 미다졸람과 프로포폴 병합요법도 무척 매력적입니다. 그러나 제가 근무하는 환경이 교육병원인 관계로 환자의 편의와 함께 환자의 안전도 놓칠 수 없는 목표입니다. 향후 변경을 고려하고 있습니다만, 아직까지는 프로포폴은 마취가 의사만 쓰도록 하고 있습니다. ESD 등 치료내시경에서는 마취과 의사를 모셔서 프로포폴 등 다양한 약제를 사용할 수 있지만, 일단 진단내시경이나 대장 용종절제술 등에서는 미다졸람과 페치딘을 쓰고 있습니다. 대강의 용량을 정해놓고 (http://endotoday.com/endotoday03/20220804_03.jpg) 환자상태에 따라서 가감하여 적용하고 있습니다.
 2025-18. 유문선 선종. Pyloric gland adenoma
2025-18. 유문선 선종. Pyloric gland adenoma
[2025-2-18. 이준행] 아주 특별한 강의 영상입니다. 며칠 전 닥터빌에서 강의를 했을 때 한 분께서 질문을 주셨습니다. 강의 후 Q and A 였으므로 간단히 답하였습다. 다음 날 내시경 사진과 함께 메일로 상세한 질문이 도착하였습니다. 저도 메일로 짧게 답하였지만 아무래도 부족한 것 같아 동영상을 만들었습니다.
[2025-2-14. 애독자 질문] 교수님. 안녕하십니까. 어제 닥터빌에서 pyloric gland adenoma로 질문 드렸던 XXX입니다. 고령의 여자분이셨고 fundus와 upper body에 걸쳐 4~5cm 가량의 mass-like elevated lesion이었고 발적성 점막 변화와 일부는 두꺼워진 점막 변화를 보이며 겸자에 조직이 뭉텅이로 부스러지듯이 떨어지는 양상에 antrum에 비하여 body와 fundus의 위축성 변화가 현저한 소견이었습니다. 조직 검사에서는 focal HGD로 확인되었고 지역거점 대학 병원에서 수술을 권유 받았습니다. 이제까지 봤던 암들과는 상당히 다른 모습이라고 생각되었던 병변이라 질문을 드려보았고 특별하지는 않다는 교수님의 답변을 듣고, 엔도투데이도 한 번 더 찾아보았습니다. 올해도 건강하시고, 항상 좋은 가르침을 주고 계셔서 늘 감사하고 있습니다.
[2025-4-14. 이준행 답변] 예. 저도 좀 더 확인하여 update 하겠습니다. 1. 일반적으로 adenoma의 subtype에 따른 치료 원칙의 차이는 없습니다. 2. 암이 아닌 이상 수술보다는 비록 incomplete resection이라도 내시경으로 어떻게 해 보는 것을 좋아하는 분들도 계십니다. 감사합니다.
[2025-2-17. 애독자께서 강의 영상을 보신 후 주신 댓글] 교수님. 질문 드렸던 애독자입니다. 사소한 질문일텐데 이렇게 빨리 피드백 해 주셔서 감사 드립니다. 많은 공부가 되었습니다.
 2025-17. 내시경 증례를 통해 확인하는 알쏭달쏭 Q&A 8탄
2025-17. 내시경 증례를 통해 확인하는 알쏭달쏭 Q&A 8탄
 2025-16. EUS for EGC. EUS는 ESD 전 침윤깊이 평가에 도움이 되는가
2025-16. EUS for EGC. EUS는 ESD 전 침윤깊이 평가에 도움이 되는가
 2025-15. 헬리코박터 강의를 듣고. Helicobacter 제균치료 강의를 듣고 느낀 점 두 가지
2025-15. 헬리코박터 강의를 듣고. Helicobacter 제균치료 강의를 듣고 느낀 점 두 가지
 2025-14. 뒤늦게 발견된 위암 대장전이. Colonic metastasis from gastric cancer
2025-14. 뒤늦게 발견된 위암 대장전이. Colonic metastasis from gastric cancer
 2025-13. 폐암 위전이. Gastric metastasis from lung cancer
2025-13. 폐암 위전이. Gastric metastasis from lung cancer
 2025-12. 날문 궤양. Pyloric ring ulcer
2025-12. 날문 궤양. Pyloric ring ulcer
 2025-11. 미분화 조직형 조기위암 내시경 치료. ESD for EGC with undifferentiated type histology
2025-11. 미분화 조직형 조기위암 내시경 치료. ESD for EGC with undifferentiated type histology
[2025-2-3. 애독자 질문] 교수님 항상 강의 잘 듣고있습니다. 한가지 질문이 있습니다. LN2개 미만인경우는 수술을 하더라도 항암 없이 Obsevation아닌지요? 이 경우에서도 수술과 ESD가 생존률 차이가 있을 것이라고 예상하시는지요?
[2025-2-3. 이준행 답변] 좋은 질문 감사합니다.
1) 위암 수술 후 보조항암치료는 림프절 전이 여부로 결정하는 것이 아니고 staging으로 결정합니다. 2기 이상에서 보조항암치료를 합니다. 예를 들어, AJCC 7판으로 점막암이고 림프절이 2개 양성이라면 T1a, N1이고 stage 1b입니다. 보조항암치료를 하지 않습니다. Subserosa암이고 림프절 전이가 없다면 T3, N0이고 stage 2a입니다. 보조항암치료를 합니다. 림프절 전이 여부로 항암치료를 하지 않고 depth of invasion과 림프절 전이를 모두 고려하여 결정한다고 생각하시기 바랍니다. 점막하암이고 림프절이 2개 양성이라면 T1b, N1이고 stage 1b입니다. 이런 환자 중 나름대로 공부하고 여기 저기 알아본 후 보조항암요법을 받고 싶다고 찾아오는 경우가 있습니다. 그런데 stage 1b에서 보조항암요법을 투약할 수 있는 방법이 없습니다. 심평의학 공화국인 우리나라에서는 불가능합니다. 예외는 없습니다. 외국에 가셔야 합니다.
2) "이 경우에서도 수술과 ESD가 생존율 차이가 있을 것이라고 예상하시는지요?" 부분은 조금 tricky한 질문입니다. 조기위암이고 림프절 전이가 1-2개인 환자가 수술을 받았다면 R0 resection이고 stage 1b이므로 보조항암요법 없이 장기 생존을 기대할 수 있습니다. 그런데 이 환자가 ESD를 받았다면 stomach wall의 local control은 되었더라도 림프절 전이는 그대로 놔 두는 것입니다. R1 또는 R2 resection입니다. 아직 절제가 다 된 것이 아닙니다. 장기적으로 보다 큰 전이를 일으킬 것입니다. Complete resection이 된 후 재발을 걱정하는 것(수술)과 처음부터 아예 complete resection이 되지 못하고 전이 림프절이 남이있는 것(ESD)은 전혀 다른 상황입니다. 보조항암요법을 하느냐 하지 않느냐와 ESD 적응증이냐 아니냐는 전혀 다른 범주입니다.
[2025-2-3. 애독자 질문] pathology에서 awd with apd 같은 병리 보고를 주시는 경우가 있는데 이러한 경우에는 분화암과 미분화암 어떻게 구분해서 치료 방향을 결정하여야 하나요? (AWD with pcc component 20% 같은 분화암과 미분화암을 같이 적어주는 경우)
[2025-2-3. 이준행 답변] Adenocarcinoma, well differentiated with poorly cohesive carcinoma 20%와 같은 병리 소견은 혼재형 (mixed type)으로 보고 있습니다. 예후는 분화 조직형 > 미분화 조직형 > 혼재형이라는 즉 혼재형이 가장 나쁘다는 것이 일반적인 견해입니다. 몇 % 이상이 혼재형인지 정의가 없고, 혼재형에 대한 ESD 적응증이 확립되어 있지 않으므로 보통 미분화 조직형에 준하여 치료법을 선택하고 있습니다. 전문가에 따라서 5% 이하의 미분화 조직형 component는 무시하기도 합니다. 저는 내시경 소견과 병리 소견을 모두 재검토합니다. 시대가 바뀌고 있습니다. Digital pathology가 보급되고 있습니다. 이제는 내시경 의사도 병리의사가 써 준 결과를 text로만 볼 것이 아니고 애매하면 직접 병리 사진을 보는 것이 좋다고 생각합니다. 직접 병리 슬라이드를 볼 수 있는 digital pathology 환경이 아니라면, 대신 병리과 의사에게 전화해 보실 것을 권합니다. Text에 없는 이야기를 듣게 되는 경우도 적지 않습니다.
 2025-10. Metachronous cancer after ESD for cardia EGC
2025-10. Metachronous cancer after ESD for cardia EGC
 2025-9. 소화성 궤양 추적내시경에서 PPI를 중단해야 하는가?
2025-9. 소화성 궤양 추적내시경에서 PPI를 중단해야 하는가?
 2025-8. Amebic colitis. 아마베 장염
2025-8. Amebic colitis. 아마베 장염
 2025-7. Bleeding peptic ulcer case discussion. 소화성 궤양 출혈 증례 토의.
2025-7. Bleeding peptic ulcer case discussion. 소화성 궤양 출혈 증례 토의.
[2025-1-26. 애독자 질문] Alcoholics case
에서 PPI를 유지한 상태로 내시경 재검을 시행하신 듯 한데, CLO 등 헬리코박터 검사의 위음성 가능성은 없을지요?
[2025-1-26. EndoTODAY 답변] 좋은 질문 감사합니다. 증례에서는 일단 지혈술 후 즉시 헬리코박터 검사를 하였습니다. 당시는 Giemsa 음성이었습니다. 물론 출혈 상황에서 헬리코박터 조직검사의 양성률이 조금 낮을 수 있다는 점은 이해하고 있습니다. Helicobacter 양성일 것으로 예상되는 상황에서 음성이 나왔으므로 추적검사에서도 헬리코박터 검사를 하는 것이 좋은 상황이었습니다. PPI를 4주 처방하고 3주 후 내시경 검사를 하였으므로 질문주신 바와 같이 PPI를 유지한 상태로 내시경 재검을 한 것은 맞습니다. 저도 소화성궤양 환자의 추적검사에서 PPI를 2주 중단하고 내시경을 하면서 헬리코박터 검사를 합니다. 그러나 고위험 출혈 환자에서, 특히 만성 질환이 있거나 NSAIDs나 술을 끊지 않은 환자에서 PPI 중단 후 내시경 검사를 하기 전 1-2주 사이에 재출혈을 하는 경우를 경험한 바 있습니다. 이런 위험이 있는 경우에는 헬리코박터 검사의 정확도가 다소 낮아지는 것을 감수하더라도 on PPI 상태에서 내시경 검사를 하고 있습니다. 헬리코박터는 추후 언제든지 검사할 수 있기 때문입니다. "이러저러한 이유로 헬리코박터 검사를 충분히 할 수 없었으니 이제 헬리코박터 검사를 해 봅시다"라고 말할 기회는 많습니다. UBT를 하면 됩니다. 헬리코박터 제균치료 후라면 일반 보험 급여, 헬리코박터 제균치료를 하지 않았던 환자에서는 비급여입니다.
[2025-1-26. 애독자 질문] 말씀주신 상황에서 serology 를 고려해 보는것은 대안이 될 수 있을까요?
[2025-1-27. EndoTODAY 답변] 예. UBT가 어려울 상황에서는 serology도 가능할 것으로 판단됩니다.
 2025-6. Exophytic SET at antrum에 대한 질문에 답합니다.
2025-6. Exophytic SET at antrum에 대한 질문에 답합니다.
 2025-5. Depth of invasion of a small depressed lesion with focal wall thickening. 조기위암인가 진행성 위암인가?
2025-5. Depth of invasion of a small depressed lesion with focal wall thickening. 조기위암인가 진행성 위암인가?

2025-1-15. ECR
 2025-4. AGC B-IV. 보만 4형 진행성 위암
2025-4. AGC B-IV. 보만 4형 진행성 위암
2025-1-10. ECR
[애독자 편지]
교수님 새해 복 많이 받으시고 더욱 건강하십시오. 증례2의 HP(-) fundic gland adenocarcinoma가 반갑네요. 일본 NTT 견학할때 HP(-) raspberry-like gastric fovelor type adenocarcimoma를 EMR-C로 시술하는 것을 자주 보았는데요. 다발성 위저선 용종환자에서 라즈베리모양의 용종은 없는지 꼼꼼히 확인하여 자주 발견하는 것을 보고 놀랐던 기억이 있습니다.
1) ColonTODAY - 대장 질환 증례 토의
2) SmallTODAY - 소장 질환 증례 토의
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.