 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Colorectal neuroendocrine tumor. Rectal carcinoid. 대장직장 신경내분비종양. 직장 유암종] - 終
[Colorectal neuroendocrine tumor. Rectal carcinoid. 대장직장 신경내분비종양. 직장 유암종] - 終
[알림]
2023년 3월 26일 내시경학회 KSGE 세미나에서 직장 NET의 코드에 대한 질의 응답이 여러번 있었는데 모두 C code를 주고 있다고 하셨습니다. 코드는 계속 바뀝니다. EndoTODAY에 의존하시지 마시고 심평원에 직접 문의하여 확인하실 것을 권합니다.
1. 내시경 치료
2. 내시경 치료 후 어떤 환자에서 수술을 권해야 하는가?
3. Rectal neuroendocrine carcinoma
4. Cases
5. FAQs
6. References
 1. 내시경 치료 Endoscopic treatment
1. 내시경 치료 Endoscopic treatment
Simple EMR 부터 ESD 까지 다양한 방법이 적용되고 있습니다.
2019-12-10 내시경학회 집담회에서 아산병원에서 anchor를 이용한 EMR법으로 EMR-C 법보다 빠르고 안전하게 치료하였다고 보고하였습니다.
2022년 대한소화기내시경학회 제1회 Webinar topic이 직장신경내분비종양이었습니다. 변정식 교수님의 멋진 강의를 소개합니다.
 2. [IDEN 2015] 내시경 치료 후 어떤 환자에서 수술을 권해야 하는가? (계명대학교 김은수 선생님 강의)
2. [IDEN 2015] 내시경 치료 후 어떤 환자에서 수술을 권해야 하는가? (계명대학교 김은수 선생님 강의)
계명대학교의 김은수 선생님은 screening을 하면 10 mm 이하의 rectal NE tumor의 비율이 현저히 높아진다는 이야기로 강의를 시작하셨습니다.
내시경적 치료방법은 다양한데 ESD와 modified EMR의 성적이 비슷하다는 점을 재치있는 슬라이드로 쉽게 보여주셨습니다. 동경암센터의 일본인 의사는 rectal carcinoid를 ESD할 필요가 없다고 comment 하였습니다.
NCCN guideline (2015)에서는 "<1cm, No follow-up reguired"로 되어 있고, 연세대 연구(Kim DH. Digest Dis Sci 2014)에도 위험인자가 없는 환자에서 intensive surveillance가 필요하지 않다고 언급되어 있습니다.
김은수 선생님은 5 mm grade 1 rectal NE tumor의 EMR 조직에서 lymphatic invasion이 있어 수술을 권하였고 local lymph node metastasis가 있었던 증례를 소개하셨습니다. 서울아산병원에서는 직장 유암종 내시경치료 후 직장옆 림프절이 천천히 (7년) 커진 것을 발견하고 수술하기도 했습니다 (Kim SH. Intest Res 2015). 즉 전이가 있어도 매우 천천히 자란다는 것입니다.
직장 신경내분비종양의 크기가 작더라도 lymphovascular invasion이 있으면 림프절 전이의 가능성은 아주 높습니다. 2022년 Gut and Liver 지에 실린 국내 연구에 의하면 약 48.8%라고 합니다.
고민이 아닐 수 없습니다. 내시경으로 잘 절제된 1 cm 이하의 작은 유암종의 병리검사에서 위험인자가 없으면 추적관찰을 하지 말자는 가이드라인과 연구가 계속 발표되고 있습니다. 그런데 추적관찰 대상이 아닌 환자에서 간혹 전이(metastasis)가 발견됩니다. 5년 이후에 발견되는 경우도 있습니다. 도대체 누구를 언제까지 추적관찰 하여야 할까요? 1명도 놓치지 않으려면 너무 많은 사람이 너무 많은 검사를 받아야 합니다. Risk benefit 연구가 필요하다고 생각됩니다. 아직 명확히 정리되지 못한 이슈입니다.
 3. Rectal neuroendocrine carcinoma
3. Rectal neuroendocrine carcinoma
건강검진에서 하부직장, anus에 연한 neuroendocrine tumor가 발견되어 수술한 환자입니다. 대단한 실력을 가진 의사를 만나 생명을 건진 운 좋은 환자이십니다.
Rectum and anus, abdominoperineal resection: Neuroendocrine carcinoma (G3)
1. Name of Procedure: Abdominoperianal resection
2. Site of Tumor: Rectum
3. Diagnosis: Neuroendocrine tumor
4. WHO classification(2010): Neuroendocrine carcinoma (G3)
5. Multiplicity: Single
6. Size: 1.5x1 cm
7. Extent: Proper Muscle
8. Grading: Mitotic Count: >20/10HPF, Ki-67 labeling index : G3>20%
9. Immunohistochemical Stains: 1. Synaptophysin : Positive, 2. Chromogranin A: Negative, CD56 (+)
10. Lymphovascular invasion: Present
11. Perineural invasion: Present
12. Lymph node metastasis: Number of positive nodes/Total number of nodes(0/16)
13. Resection Margins: Negative
14. Other pathologic components: Hyperplastic polyp
제가 우연히 추적검사를 하였던 환자입니다. 수년 전 rectal carcinoid로 의뢰된 분으로 ESD가 시행되었습니다. 당시 lifting이 되지 않아 시술이 어려웠을 것 같습니다. 여하튼 완전 절제가 되었습니다.
ESD 병리결과는 아래와 같았습니다. Carcinoma였고 깊었고 lymphatic invasion이 있었습니다.
1. Name of Procedure: EMR/ESD
2. Site of Tumor: Rectum
3. Diagnosis: Neuroendocrine tumor (Well-differentiated neuroendocrine carcinoma)
4. WHO classification(2004): Well-differentiated neuroendocrine carcinoma
5. Multiplicity: Single
6. Size: 1x0.9 cm
7. Extent: Proper Muscle
8. pT Stage(AJCC): T2
9. Grading: Mitotic Count(/HPF): 0-1, Ki-67 labeling index: G2 3-20 %
10. Lymphovascular invasion: Present
11. Perineural invasion: Not identified
12. Resection Margins: Positive deep resection margin
. D2-40: Endolymphatic emboli are present
. Ki-67: Positive (3 %)
. Chromogranin: Positive
. Synaptophysin: Positive
수술을 시행하였고 두 개의 perirectal lymph node 전이가 있었습니다.
몇 년 후 제가 추적 내시경을 하였습니다. Sigmoidoscopy였습니다.
화면 좌측이 정상 lumen이데 화면 우측 1시 방향에 또다른 lumen이 있었고 blind end였습니다. 무슨 pouch라는 느낌이 들었습니다. 외과 선생님께 문의하였습니다.
제가 오늘 직장경 검사를 한 명 하였습니다. Rectal neuroendocrine carcinoma로 수술한 환자입니다. 직장경을 항문 상방으로 진입하였을 때 화면의 좌측에 정상 lumen이 있고 화면의 우측에 pouch가 있었습니다. Pouch의 끝은 blind end 였습니다. 그런데 수술기록을 보니... 수술명이 "Low Ant.Resection, Ileostomy"라고만 씌여있고 어디에서도 pouch를 만들었다는 이야기가 없었습니다. 위암 전문 내과 의사로서는 수술 내용을 이해하기 어려웠고 경험이 부족한 의사가 pouch쪽으로 내시경을 밀어넣다보면 천공도 생길 수 있겠다 싶었습니다. 이 환자에 대한 의견을 부탁드립니다. 수술 내용을 좀 더 잘 써줄 수는 없는지...
외과 선생님께서 친절하게 답변을 보내주셨습니다. 그림과 함께...
질문/의견 주셔서 감사합니다. 환자의 내시경 사진 및 수술기록을 확인하였습니다. 수술 기록의 "수술방법 → anastomosis → method" 부분을 보면 side-to-end 라고 되어있습니다. 내과 선생님께서 이 부분까지 확인하기는 어려우셨으리라 생각됩니다.
Anastomosis:
Circular stapler(name : EEA) (size : 28mm)
Method :Side-to-end
Level of anastomosis : 1㎝ from anal verge
Leakage test : No
차세대 EMR이 되면 좀더 보기 좋게 변할 것입니다. 그 때까지는 수술기록지에서 수술방법 → Anstomosis 부분을 참고해주시면 사고 예방에 도움이 될 것 같습니다. 참고하시도록 그림을 그려보았습니다.
외과 선생님께서 그림까지 그려서 친절히 설명해주시니 쉽게 이해할 수 있었습니다. 환자가 어떤 수술을 받았는지 정확히 알고 내시경 검사를 해야겠습니다. 바른 내시경이 안전한 내시경입니다.
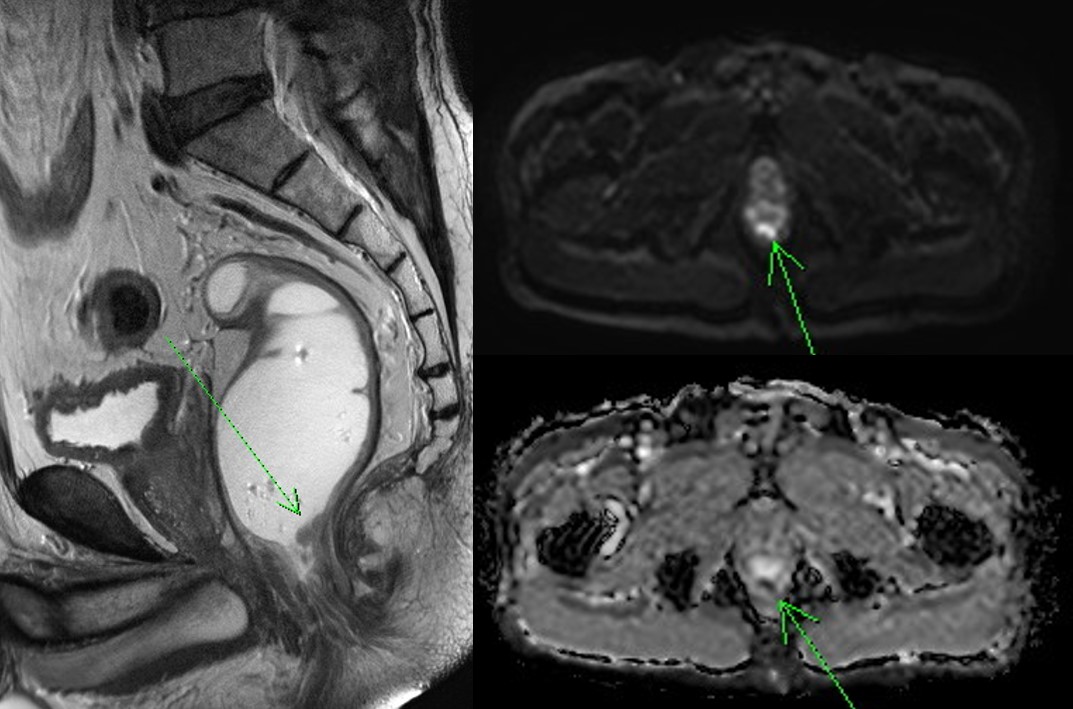
[증례 1] Rectal neuroendocrine carcinoma with liver metastasis
건진 복부 초음파에서 간 종양이 발견되어 의뢰된 분입니다. MRI에서는 epithelial hemangioendothelioma 아닌가 추정하였지만 간 조직검사는 neuroendocrine carcinoma로, 직장 종양 조직검사는 neuroendocrine carcinoma with lymphatic tumor emboli, Chromogranin (+, focal), Synaptophysine (+, diffuse)로 나왔습니다. 환자는 flushing과 pruritus 증상이 있었습니다. Octreotide IM으로 치료하였고 증상은 다소 호전되었습니다.
[증례 2] Rectal carcinoid with lymph node metastasis
Rectal carcinoid로 의뢰된 환자입니다.
ESD가 시행되었고 병리소견에서 lymphatic invasion이 의심되었습니다.

Well differentiated neuroendocrine tumor (CARCINOID) (G1)
1) size: 1.2x1.0 cm
2) confined to mucosa and submucosa
3) mitosis: 1/10 HPF
4) lymphovascular invasion: suspicious (in one focus)
5) perineural invasion: absent
6) focal involvement of deep cauterized resection margin
수술을 시행하였고 아래의 결과였습니다.
Rectum, low anterior resection : Status post endoscopic submucosal dissection for well-differentiated neuroendocrine tumor
. No residual tumor
. Histologic type and grade: not identified (no residual tumor):
1. Location: rectum
2. Gross type: scar
3. Size: cannot be determined (no residual tumor)
4. Depth of invasion: cannot be determined (no residual tumor)
5. Resection margin: free from carcinoma (no residual tumor) safety margin: proximal, 9.2 cm; distal, 0.5 cm; circumferential (radial), >10 mm
6. Lymphovascular invasion: cannot be determined (no residual tumor)
7. Perineural invasion: cannot be determined (no residual tumor)
8. Regional lymph node metastasis: metastasis to 1 out of 12 regional lymph nodes (1/12: perirectal, 1/12)
직장 유암종 내시경 치료에서는 병리과 선생님이 매우 매우 매우 매우 중요합니다.
[증례 3]
대한장연구학회 교육자료로 rectal carcinoid with liver metastasis 증례가 소개되었습니다.
[2016-7-1. 애독자 질문]
질문 1. 대장 내시경중 Rectal carcinoid 로 1cm 이하인 경우 abd' CT 등 study 를 다 진행해야 되나요??
질문 2. rectal carcinoid <1cm (거의 5mm 정도 size) 를 EMR 로 제거시 resection margin 이 positive 인 경우 어찌해야 하나요?
[2016-7-3. 김은란 교수님 답변]
질문 1에 대한 답변: Rectal carcinoid tumor의 크기가 1 cm 미만이면서 근육층 침범이 없고, 조직학적으로 악성도가 높지 않은 경우 주변 림프절 전이나 간전이등의 가능성은 매우 낮습니다. 그러나 드물게 증례보고가 있으므로 CT 검사를 해 보는 것은 좋겠습니다.
질문 2에 대한 답변: 대장의 경우 조직이 얇아서 hot snaring polypectomy등을 시행할때 burning effect로 인해 resection margin (+)로 나오는 경우가 있습니다. 가장 중요한 것은 시술자의 판단입니다. 시술자가 완전 절제했다고 판단하였다면 조직검사에서 RM (+)로 나와도 크게 염려하지 않아도 될 것 같습니다. 다만, 시술자가 판단하기에 완전절제된 것 같지 않다면, 가장 좋은 것은 그 부위를 한번 더 ESD로 절제해 주는 것이고, 거의 절제된 것 같은데 확신이 없는 경우는 short-term follow up하셔도 될 것 같습니다.
[2017-9-1. 애독자 질문]
안녕하세요. 이번에 대장내시경을 하다가 직장 유암종 환자가 있어서 질문 메일 드립니다. 크기는 0.7cm정도였고, EMR로 제거하였고, 조직검사 결과 유암종, 혈관이나 림프절 침범은 없었고, CT에서 타장기 전이는 없었습니다. 그리고 mitotic count와 Ki67에서 G1이였습니다. 이 환자를 암으로 하고 산정특례를 해야하는지요? 그리고, 보험공단에 전화해서 물어보니 유암종 코드가 없다고해서 당황했습니다. 선생님은 코드를 뭘로 넣으시는지 궁금합니다. 그리고, 유암종 G2~3으로 grade가 올라가면 산정특례로 해야하는지도 궁금합니다.
위 유암종은 f/u에 대해서 자세한 도표가 있었는데 EndoTODAY에서 직장 유암종에 대해서는 f/u 에 대한 도표가 없어서요. 위랑 같이 처리하면 되는지요? 선생님 기재하신 내용보면 간혹 f/u에서 전이가 있다고 하셨는데, 대부분이 괜찮다고 하시긴 하셨습니다.
이제 선선해지는데 환절기에 감기 조심하시고요, 머나먼 시골에서 선생님 덕분에 환자들한테 선생님 경험을 조금이라도 빌려 좀 더 잘 진료할 수 있다는 사실에 항상 감사드립니다.
[2017-9-1. 이준행 답변]
일전에 제가 아래와 같은 position statement를 낸 적이 있는데 아직도 같은 입장입니다.
[Position statement. 2016-9-4. 이준행]
직장 유암종 코드는 아직 학문적으로 정립되지 않은 부분입니다. 현재로서는 대장내시경 전문가들의 의견(아래 도표)을 따르는 것이 가장 적절할 것으로 판단됩니다.코드는 정부가 책임을 방기(放棄; 놓을 방, 버릴 기)하고 있는 부분인지라, 즉 정확한 기준을 밝히지 않고 있는지라 어느 누구도 답할 수 없는 영역입니다. 아래를 참조하세요.
* 참고: EndoTODAY 코드
[2017-9-2. 애독자 편지]
1cm 미만의 Rectal NET에대해 D코드인지 C코드인지는 전문가 의견에 따라야겠지만 아직 혼란스럽습니다. 특히 'D코드를 주는 의사결정'과 '(매우 낮지만) 전이 가능성을 확인하기위해 복부CT를 촬영하는 의사결정'은 이율배반적인 의사결정이라고 생각됩니다.
[2017-9-2. 이준행 답변]
좋은 의견 감사합니다. '전문가 의견을 따르는 것'은 일견 쉬운 일 같지만 (1) 전문가들마다 의견이 다른 경우가 많고, (2) 전문가들 모임에서 가이드라인이나 consensus 보고서를 내고 있으나, 여러 다른 그룹에서 약간씩 다른 보고서를 내고 있어서 어느 것을 표준으로 할 것인지 알 수 없으며, (3) 같은 그룹에서도 비슷한 보고서의 update version을 내곤 하는데 그때마다 코드와 비용이 달라야 하는지 등 쉽지 않은 이슈가 많습니다. 따라서 이것은 칼자루 혹은 돈자루를 쥐고 있는 정부에서 (1) 직접 정확한 코드 지침을 내리거나 (2) 어느 학회에서 언제 발표한 consensus 보고서를 따른다고 정해 주지 않는 한 혼선은 계속될 수 밖에 없는 구조입니다. 국민의 의료비용 부담을 줄이는 것은 좋은 정책방향이지만, 코드나 진단명에 따라서 세세한 비용 하나 하나를 깎아주는 정책은 혼선이 많고 과잉 진료를 유발할 수 있다는 점에서 바람직하지 않다고 생각합니다. CT는 전이 가능성이 매우매우 낮아도 찍어볼 수 있을 것 같습니다.
[2019-12-6. 애독자 질문]
교수님. Rectal carcinoid 같은경우 5~10mm 정도로 작게 발견되는 경우가 있는데 상급병원 의뢰시 bx를 하는것이 좋을시 아니면 NET 가 육안으로 의심되면 그대로 놔두고 의뢰드리는것이 좋을지 궁금합니다. mailgnant potential 이 있어보이는 병변을 1차의료기관에서 EMR 을 하기에는 부담도 되서요..
[2019-12-6. 이준행 답변]
Rectal carcinoid 처럼 보이는 병변을 조직검사 없이 바로 EMR/ESD 하는 경우는 드물 것 같습니다. 1차 의료기관에서 조직검사 후 의뢰주시면 중증종합병원에서는 다양한 내시경적 방법으로 제거할 수 있을 것입니다. 참고로 carcinoid는 점막하종양이라는 넓은 범주에 속해있지만 주로 lamina propria 기원입니다. 실제로 forceps biopsy를 통하여 조직학적 진단이 잘 되는 편입니다.
1) EndoTODAY Gastric carcinoid 위유암종
2) EndoTODAY Duodenal carcinoid 십이지장 유암종
3) EndoTODAY Colorectal neuroendocrine tumor. carcinoid 결장직장 신경내분비종양. 직장 유암종.
4) Carcinoid Tumor 대한 Helicobacter 및 상부위장관 연구학회 춘계심포지엄 (이준행. 2009)
5) EndoTODAY Case: rectal carcinoid with metastasis 직장 유암종 림프절 전이 증례
6) 직장 신경내분비종양 rectal neuroendocrine tumor 의 진단과 치료 2022-2-22 제1회 KSGE Webinar 변정식 교수님 (log-in required) - Q and A
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.