 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Thursday Endoscopy Conference 20160825]
[Thursday Endoscopy Conference 20160825]
F/32. chronic intermittent diarrhea with some episodes of hematochezia
Amebic colitis usually afffects the cecum and rectum. In the acute phase, a rectal lesion mimics the acute phase of ulcerative colitis. In the chronic phase, the cecum is usually affected with deep separative ulceration, ulceration surrounded by erythema, and ameboma.
The ulcer is typically 'flask- shaped' and the broad base is composed of fibrin and cellular debris. Visual inspection of the colon - Sigmoidoscopy and/or colonoscopy can be performed either to make the diagnosis of amebiasis or to exclude other causes of the patients' symptoms. However, colonoscopy is not recommended as a routine diagnostic approach since intestinal amebic ulcerations increase the likelihood of perforation during instillation of air to expand the colon.
Scrapings or biopsy specimens, best taken from the edge of ulcers, may be positive for cysts or trophozoites on microscopy, and antigen testing for E. histolytica may be positive. Colonic lesions in amebic dysentery range from nonspecific mucosal thickening and inflammation to classic flask-shaped amebic ulcers
오래 전 아메바 장염의 내시경과 병리소견에 대한 질문을 받은 바 있습니다. 그때 답변의 일부를 옮깁니다.
[2014-8-20. 이준행 답변]
아시다시피 flask는 삼각형 모양의 실험도구입니다. 따라서 flask-shaped ulcer는 궤양은 궤양인데 lumen 쪽의 점막조직 결손보다 점막하층 조직결손의 범위가 큰 경우를 말합니다. 즉 궤양의 입구는 좁은데 아래 쪽이 넓은 경우입니다. 점막하층을 파고 들었기 때문에 undermining ulcer라 부르기도 합니다.

Flask-shaped ulcer는 병리 소견입니다. 아메바 장염의 병리소견 사진 두 개를 소개합니다. 아! 이래서 flask-shaped ulcer라고 하는구나.... 금방 느낄 수 있습니다.
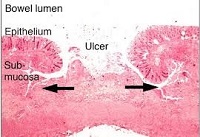

Histopathology of a typical flask-shaped ulcer of intestinal amebiasis CDC/Dr. Mae Melvin (출처)이들 궤양을 내시경으로 본다고 생각해 봅시다. Flask-shaped ulcer (= undermining ulcer)로 보일 것 같습니까? 아닙니다. 그냥 보통 ulcer로 보입니다. 제 경험과 생각으로는 amebic colitis에서 flask-shaped ulcer('플라스크모양 궤양'으로 번역해야 하지 않을까요?)를 내시경으로 관찰하기는 어려울 것 같습니다. Ginsberg 내시경책을 옮깁니다 (page 322). 더러운 점액이 부착된 다발성의 크고 작은 궤양인 경우가 많습니다. 경계는 뚜렷할 수 있고 뚜렷하지 않을 수도 있습니다.
"Amebic colitis is a protozoan infection that primarily affects the large bowel. It is most often seen in patients who recently immigrated from developing countries and who recently traveled to developing countries. Symptoms can vary from none to explosive diarrhea, tenesmus, fever and abdominal cramps.
Colonoscopic appearance during the acute phase resembles ulcerative colitis, but in the chronic phase it appears more like Crohn’s disease. The most common segments involved are the cecum and right colon, with the rectum and sigmoid less often involved. Toxic megacolon may develop in severe cases of amebiasis.
Colonoscopy reveals granular, friable, and erythematous mucosa with discrete large ulcers covered by yellowish, mucopurulent exudates. Biopsies of the margins of the ulcers provide a 60% to 90% yield of trophozoites to make the diagnosis."
Amebic liver abscess (ALA) 환자의 colonoscopy 소견을 기술한 논문이 있어서 소개합니다 (Ann Gastroenterol 2014;27: 156-161).
Colonic involvement in the form of erythema and ulceration was seen in 62 (77.5%) patients of amebic liver abscess (ALA) whereas no abnormality was seen in 18 (22.5%) patients. Cecum (70.9%) was the most common site of colonic involvement followed by lesions involving both right colon with transverse colon (35.4%) and isolated ascending colon (22.5%). There were no cases of isolated transverse colon involvement, but involvement of right colon was present in all patients with colonic involvement. Colonic lesions were more commonly seen with multiple than solitary ALA (Table 3). In patients with solitary ALA, cecum involvement (46.4%) was seen most commonly followed by isolated in the ascending colon (17.9%) and right plus transverse colon (7.1%). Most of the patients with multiple ALAs had involvement of the transverse and right colon (75%), while isolated right colon was involved in 16.6% patients. Among the 18 patients of multiple ALAs with lesions involving transverse colon, 16 had cecal lesions and two had lesions in the ascending colon. A significant involvement of the right and transverse colon was seen in cases of multiple ALAs compared to solitary ALA (P<0.0001). Histological analysis of the colonic biopsy was done in all subjects with colonic lesion; flask-shaped ulceration and acute inflammatory cells were seen commonly but trophozoite invading the lamina propria was seen in only 10 (16.1%) patients.
* 참고: EndoTODAY 아메바 장염
* 참고: 대한소화기내시경학회 교육자료 아메바 대장염 (2014-11)
 2. Pancreas cancer with duodenal invasion and gastric compression
2. Pancreas cancer with duodenal invasion and gastric compression
Anemia와 abdominal pain으로 CT를 찍고 이상소견이 있어 시행한 내시경입니다.
STOMACH: MB/PW 에 약 5cm 크기의 protruding mass 가 있으나 점막은 정상이었음 .
Duodenum: PCF scope 을 이용하여 duodenum 의 4th portion 까지 진입하였음. 4th portion 에서 약 3cm 크기의 ulcerating mass 가 관찰 이 되었음. moth-eaten edge 및 base 에는 yellowish exudate 와 hematin 이 관찰 되었음. active bleeding 소견은 관찰 되지 않았음. scope 이 더 이상 전진이 안되어 obstruction 여부는 관찰 할 수 없었음.
Impression : 1. r/o extrinsic compression, 2. pancreas cancer with duodenal invasion
EUS-FNA를 하였고 'poorly differentiated carcinoma (suspected pancreas primary)'로 확인되었습니다.
 3. Esophageal cancer recurrence
3. Esophageal cancer recurrence
식도암으로 Ivor-Lewis 수술 받은 환자입니다. 당시 병기는 pT1bN2M0였습니다. 추적내시경에서 gastric tube의 병소가 발견되었습니다. 조직검사는 squamous cell carcinoma, poorly differentiated with multiple endolymphatic emboli였습니다. 식도암 재발로 판단됩니다.
용종 조직검사에서 모두 W/D neuroendocrine tumor (carcinoid)가 나왔고 gastrin은 410으로 높았습니다. 경과관찰 중입니다.
1) SMC Endoscopy Unit 삼성서울병원 내시경실
2) SMC Monday GI conference 삼성서울병원 일원내시경교실 월요점심소화기집담회
3) SMC Thursday endoscopy conference 삼성서울병원 일원내시경교실 목요점심내시경집담회
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.