 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [일원내시경교실 목요점심집담회 2016-4-7]
[일원내시경교실 목요점심집담회 2016-4-7]
 1. Change of EGC morphology probably by PPI
1. Change of EGC morphology probably by PPI
위각의 함몰형 병소에서 조직검사하여 atypical cell이 있다고 의뢰되었습니다. 검사 직후부터 PPI를 드신 것 같습니다. 약 4주 후 내시경에서 궤양형 병소는 거의 아물어 있었습니다. 외부 조직검사 재판독과 본 병원의 내시경 조직검사 재검에서 모두 암으로 나와 수술을 하였습니다. 본 병원에서는 PPI를 드리지 않았고 약 2주 후 수술하였습니다. 수술 전날 clipping을 위하여 내시경 재검을 하였습니다. 3번의 내시경 사진을 잘 보시기 바랍니다. 조기위암은 natural history에 의하여 모양이 변하기도 하지만 PPI 등 약제에 의한 영향도 상당합니다.
Early gastric carcinoma
1. Location : lower third, Center at body and lesser curvature
2. Gross type : EGC type IIc and IIa
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size : 3.9x2.5 cm
6. Depth of invasion : invades mucosa (muscularis mucosae) (pT1a)
7. Resection margin: free from carcinoma, safety margin: proximal 3.5 cm, distal 6.3 cm
8. Lymph node metastasis : no metastasis in 65 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 7th edition: pT1a N0
위암의 자연사를 보여준 과거 증례를 소개합니다.
70대 남자입니다. Cardia를 involve하는 위암으로 수술을 권하였으나 수술하지 않고 경과관찰을 원하시어 follow-up loss가 되었다가 1달 전부터 dysphagia가 있어 의뢰된 환자입니다. 18 개월 전 사진을 보면 병소의 distal margin은 upper body와 mid-body의 경계 정도였으나 최근 내시경에서는 cardia involve가 있었고 (사진생략), angle까지 병소가 넓어졌습니다. 비교적 빠른 속도의 progression을 보인 진행성위암이었던 것으로 판단하였습니다.
과거에는 고령의 환자들에게 수술을 권하는 것은 매우 어렵고 위험한 일로 간주되었습니다. 그러나 최근에는 고령의 환자라고 하더라도 performance가 좋은 경우는 적극적인 치료를 권하는 것이 보통입니다. 수술에 따른 위험성은 실제 연령보다는 cardiopulmonary function에 의하여 결정되는 것으로 생각되기 때문입니다. 수술이 가능한 진행성위암 환자에서 초고령 환자라고 하더라도 중년 환자에 비하여 수술에 따른 morbidity와 mortality가 유의한 차이가 없다는 것은 여러 보고에서 반복적으로 확인되고 있습니다.
어떤 선생님은 이런 말씀을 하셨습니다. "나이는 단지 숫자일 뿐이다."
Advanced gastric carcinoma
1. Location : [1] lower third, [2] duodenum, Center at antrum and lesser curvature
2. Gross type : Borrmann type 2
3. Histologic type : tubular adenocarcinoma, poorly differentiated
4. Histologic type by Lauren : diffuse
5. Size : 4x3.1 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma
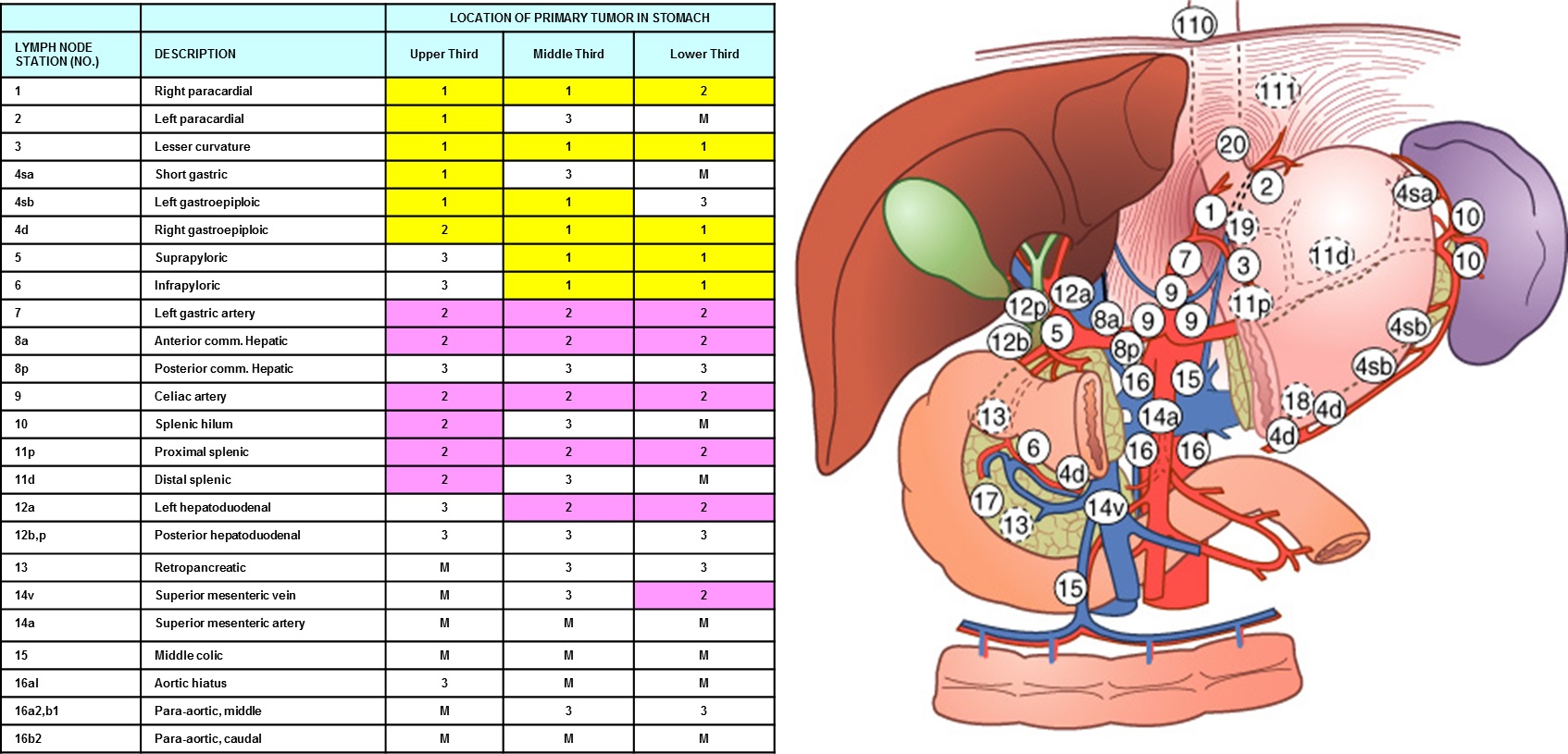
8. Lymph node metastasis : metastasis to 5 out of 30 regional lymph nodes (pN2) (5/30: "1", 0/4; "3", 1/10; "4", 1/2; "4sb", 0/1; "5", 1/1; "6", 1/4;
"8a", 0/3; "7", 0/2; "9", 0/0; "11p", 0/2; "12a", 1/1)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: pT2 N2
생각보다 림프절 전이가 현저했습니다. 3번, 4번, 5번, 6번, 12a번에 각각 전이되어 있었습니다. 아래 lymph node station을 참조하시기 바랍니다.
위 림프종은 간혹 Borrmann type II와 구분이 어렵습니다. 이 환자는 gastric biopsy에서도 diffuse large B cell lymphoma가 나왔습니다.
* 참고: EndoTODAY diffuse large B cell lymphoma
Stomach, endoscopic submucosal dissection:
2014년 증례입니다. LUQ pain, hematochezia, weight loss 3~4kg/10days 등으로 CT를 시행하고 "colon(splenic flexure) wall thickening with omentum invasion 있어 r/o colon ca, r/o metastatic cancer" 소견으로 의뢰되었습니다. 대장내시경과 CT 판독을 하였습니다. CT 판독이 매우 훌륭했습니다.
CT 판독: Left side의 gastrocolic ligament를 따라서 irregular enhancing mass가 있음. 경계가 좋지 않아 크기의 측정에 제한이 있으나 6 cm 이상의 extent를 보임. 이 병변은 상방으로 stomach의 body greater curvature side와 하방으로는 transverse colon의 upper wall까지 extension하고 있음. Involvement된 bowel wall thickening이 있으나 비교적 layering이 유지되고 있음. 그러나 transverse colon에서는 focal하게 layering이 유지되지 않는 부분이 의심됨. Left side mesorectum에 약 3.3 cm size의 enhancing mass가 있고 역시 경계가 좋지 않으며 주변으로 infiltration을 동반하고 있음. Rectum의 left side wall과 abutting하고 있으며 인접한 rectal wall에 wall thickening이 있고 역시 layering이 유지되고 있음. Pelvic cavity에 소량의 fluid collection이 있음. Uterus에 IUD insertion state임. 복강 내 의미있게 커진 lymph node 보이지 않음. 그 외 liver와 spleen, pancreas, both kidneys에 특이소견 없음. GB에 특이소견 없고 biliary tree dilatation 없음. Scan에 포함된 basal lung과 bone에 특이소견 없음.
Transvaginal biopsy를 시행하였고 다음의 결과였습니다. Inflamed granulation tissue with abscess and dense fibrosis. Bacterial colony present, consistent with actinomycosis
Treatment: IV penicillin G
2017년 3월 내시경학회 교육자료가 복부 방선균증 (actinomycosis) 이었습니다.
1) SMC Endoscopy Unit 삼성서울병원 내시경실
2) SMC Monday GI conference 삼성서울병원 일원내시경교실 월요점심소화기집담회
3) SMC Thursday endoscopy conference 삼성서울병원 일원내시경교실 목요점심내시경집담회
© EndoTODAY Endoscopy Learninng Center. Jun Haeng Lee.
 3. 8년전 hilar mass (diffuse large B cell lymphoma)로 항암치료 받던 환자의 gastric recurrence
3. 8년전 hilar mass (diffuse large B cell lymphoma)로 항암치료 받던 환자의 gastric recurrence
 4. 60 대 여. EGC. ESD 시도하였으나 깊어서 수술을 하였습니다.
4. 60 대 여. EGC. ESD 시도하였으나 깊어서 수술을 하였습니다.
Early gastric carcinoma
1. Location : antrum, lesser curvature
2. Gross type : EGC type IIa & IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 20 mm (2) vertical diameter, 17 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 3000 ㎛) (pT1b)
7. Resection margin : involved deep resection margin by carcinoma, safety margin : distal 8 mm, proximal 6 mm, anterior 6 mm, posterior 6 mm, deep 0 mm
8. Lymphatic invasion : present
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
 5. 40 대 여. Actinomycosis (복부 방선균증)
5. 40 대 여. Actinomycosis (복부 방선균증)
CONCLUSION: Inflammatory lesion such as actinomycosis R/O Malignancy such as transverse colon cancer with peritoneal seeding.
RECOMMENDATION: Transrectal biopsy for mesorectal mass.