 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
001 | 101 | 201 | 301 | 401 | 501 | 601 | 701 | 801 | 901 | 1000
2012년 치료 결과를 분석하여 'Diagnostic group classifications of gastric neoplasms by endoscopic resection criteria before and after treatment: real world experience'라는 제목으로 분석하였습니다. Absolute indication EGC, Expanded indication EGC, Beyond expanded indication EGC 등을 '진단명'이라고 붙일 수 없어서 'diagnostic group classification'이라는 말을 만들어 써 보았습니다.
Background and study aims: There are often discrepancies between the pretreatment evaluation of gastric neoplasms by endoscopy with biopsy and the final diagnosis of resected specimen in terms of pathology and depth of invasion. We evaluated the spectrum of discrepancies between pretreatment and posttreatment diagnosis which may deliver significant differences on clinical practice.
Patients and Methods: A total of 2,041 patients with gastric dysplasia or cancer who underwent curative endoscopic resections or surgeries in 2012 were enrolled. Patients were classified into five different diagnostic groups; low-grade dysplasia (LGD), high-grade dysplasia (HGD), absolute indication early gastric cancer (AI-EGC), beyond absolute indication early gastric cancer (BAI-EGC), and advanced gastric cancer (AGC). The choice of initial treatment and final pathologic diagnosis was analyzed.
Results: The study patients belonged to the following pretreatment diagnostic groups; LGDs in 162, HGDs in 164, AI-EGCs in 396, BAI-EGCs in 824, and AGCs in 495 cases. Posttreatment diagnostic groups were LGDs in 140, HGDs in 121, AI-EGCs in 322, BAI-EGCs in 947, AGCs in 505, and no residual tumor in 6 cases. In general, 6.9% (141/2,041) of cases were down-graded, and 15.9% (324/2,041) were up-graded. Thirty-four percent of pretreatment HGDs (56/164) were changed to cancers after endoscopic resection. Thirty-three percent of pretreatment AI-EGCs (131/396) were re-grouped as posttreatment BAI-EGCs. The additional surgery rate in each pretreatment group was 0.6% in LGD, 4.3% in HGD, 15.7% in AI-EGC, 23.6% in BAI-EGC among the patients with initial endoscopic resection (p < 0.01).
Conclusions: Twenty-three percent of gastric neoplasms changed in their final diagnostic group after endoscopic resection or surgery. This discrepancy should be considered when the initial treatment strategy is being selected.
우리나라에서 ESD 영역은 무척 혼란스럽습니다. 시술 전후 병리 결과가 바뀌는 예가 너무 많기 때문입니다. 일본은 조금만 이상하면 다 암으로 진단을 붙여버리므로 ESD 시행 환자의 대부분이 처음부터 위암입니다. 그런데 우리나라에서는 상당수가 시술 전 adenoma, 시술 후 adenocarcinoma입니다. 이 부분을 frank 하게 보고한 논문이 없어서 마음 먹고 한번 정리한 것입니다.
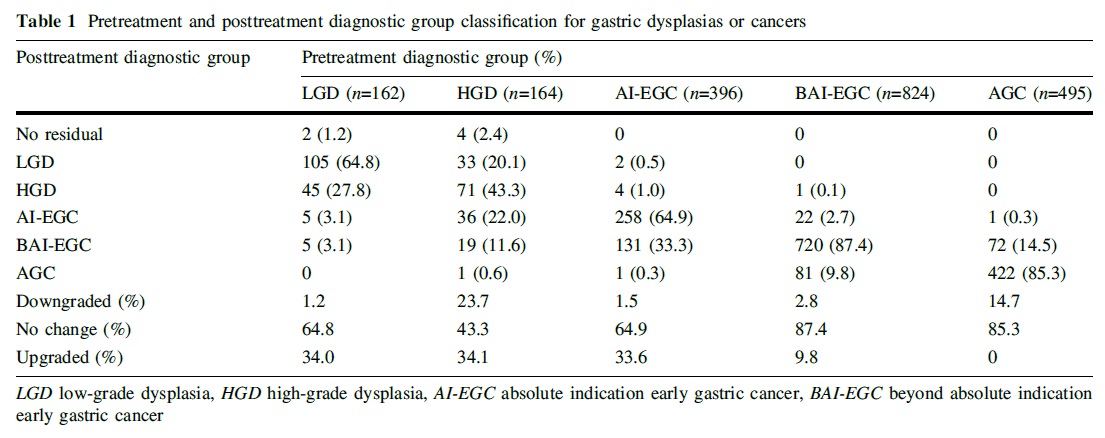 전체적으로 6.9% (141/2,041)가 down-grade 되고 15.9% (324/2,041)가 up-grade 되었습니다. Diagnostic group classification이 그렇게 바뀌었다는 의미입니다.
전체적으로 6.9% (141/2,041)가 down-grade 되고 15.9% (324/2,041)가 up-grade 되었습니다. Diagnostic group classification이 그렇게 바뀌었다는 의미입니다.
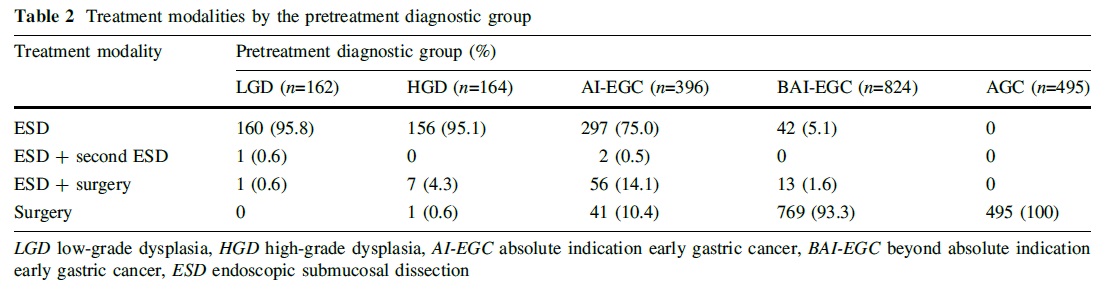 Absolute indication으로 판단된 환자의 89.6%가 첫 치료로 ESD가 선택되고 있습니다.
Absolute indication으로 판단된 환자의 89.6%가 첫 치료로 ESD가 선택되고 있습니다.
 이 결과를 바탕으로 ESD 후 수술이 필요할 확률이 15%라고 설명하고 있습니다.
이 결과를 바탕으로 ESD 후 수술이 필요할 확률이 15%라고 설명하고 있습니다.
 각 diagnostic group에 대하여 이와 비슷한 diagram을 만들어보면 재미있을 것 같습니다. Real world에서는 이렇게 복잡한 일이 벌어지고 있는 것입니다.
각 diagnostic group에 대하여 이와 비슷한 diagram을 만들어보면 재미있을 것 같습니다. Real world에서는 이렇게 복잡한 일이 벌어지고 있는 것입니다.
위 도표에서 ESD 前 absolute indication EGC로 판단되었으나 최종적으로 AGC로 나온 환자가 1명 있었습니다. 매우 드문 경우였기에 소개합니다. ESD가 시도되었는데 submucosal adhesion으로 ESD를 마칠 수 없었고 수술을 시행하여 AGC로 확인된 환자였습니다. ESD로 인한 인공궤양때문에 보만 3형으로 분류되었지만 내시경적으로는 EGC-like AGC 즉 Borrmann type unclassified가 가장 적합한 분류라고 생각합니다.
Stomach, total gastrectomy:
Status post endoscopic submucosal dissection (incomplete)
Advanced gastric carcinoma
1. Location : upper third, Center at body and lesser curvature
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size : 3x1.5 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma, safety margin: proximal 2 cm, distal 11.4 cm
8. Lymph node metastasis : no metastasis in 38 regional lymph nodes (pN0)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : present
12. Peritoneal cytology : negative
© 2015-12-3. 일원내시경교실 바른내시경연구소 이준행