 [Description exercise 6 해설] - 終
[Description exercise 6 해설] - 終
 [Description exercise 6 해설] - 終
[Description exercise 6 해설] - 終
이론과 실제의 균형이 필요합니다. 교과서와 논문을 통하여 이론을 배우고 증례를 통하여 실제를 배울 수 있습니다. 증례 토의 위주로 진행되는 집담회는 매우 중요합니다. 원내 집담회도 있고 원외 집담회도 있습니다.
* 참고: 삼성서울병원 목요 내시경 집담회 archive (2015-2018)
소견: 내시경을 반전하여 관찰하였을 때 hiatal opening이 넓게 확장되어 있고, 위 fundus의 일부분이 평행한 주름을 이루며 hiatal opening을 넘어 흉강까지 올라가 있음. SC junction이 hiatal opening에 비하여 약간 상방으로 올라가 있음. Cardia lesser curvature side (4시 방향)에 1cm 가량의 linear scar가 있고 erythema가 동반되어 있음. 6시 방향에도 0.5cm 가량의 유사한 소견이 있음.
진단: paraesophageal hernia (mixed type), BGU scar (Cameron ulcer scar)
[이준행 comment]
Hiatal hernia는 초심자가 개념 잡기 어려운 부분입니다. 아래 강의 동영상을 추천합니다. 그리고 이 환자에서는 4시 방향 linear scar가 있었는데 이를 보시지 못한 분들이 많았습니다. Cameron ulcer의 scar입니다.
[2017-8-17. 내시경을 배우고 있는 전공의 질문] Gastric fold가 한쪽에만 있는 것으로 paraesophageal type과 mixed type을 구분하는 것입니까?
[2017-8-18. 이준행 답변] Mixed type을 관례상 그냥 paraesophageal hernia로 부르고 있습니다. Pure paraesophageal hernia는 매우 드문 상황입니다.
(1) Hiatal hernia 중 paraesophageal hernia입니다. Squamocolumnar junction 부위는 hiatal opening에 비하여 상방으로 올라가 있으므로 엄밀히 말하면 mixed type으로 보는 것이 좋겠습니다.
(2) 순수한 형태의 type 2 (식도주위탈장, para-esophageal hernia)는 거의 없습니다. 순수한 type 2는 횡격막식도 인대의 손상은 없고, 열공 자체가 늘어나서 그 틈으로 위의 일부(특히 위분문부)가 흉강으로 빠져 들어가는 형식의 탈장을 말합니다. Gastroesophageal junction이 diaphragmatic orfice와 같은 level, 즉 정상 높이에 위치하고 있습니다. 책에서는 hiatal hernia의 2% 정도라고 합니다만 사실 저는 거의 본 적이 없습니다. 우리가 흔히 paraesophageal hernia라고 말하는 것은 대부분 type 3입니다. 아래 인터넷에서 나온 그림이 전형적인 type 2입니다. 환자 사진을 구할 수 없어서 인터넷 사진을 이용함을 용서해 주시기 바랍니다.
(3) Hiatal opening 직하부의 발적된 scar 모양 병소를 지적한 것은 매우 훌륭한 일입니다. 대부분 답변자가 이를 언급하지 않았습니다. 위암은 아니고 hiatal hernia가 심할 때 발생하는 hiatal hernia opening 부위 궤양의 반흔입니다. Cameron ulcer 반흔으로 판단하면 무난하겠습니다.
Cameron ulcer와 hiatal hernia. PDF 3.7M - Case Reviews in Gastroenterology
EndoTODAY '위내시경 삽입과 관찰' 180쪽을 참고하십시오.
* 참고: EndoTODAY 식도열공탈장
소견: GE junction 12시~4시 방향에서 mucosal break가 fusion 된 것처럼 보이는 geographic한 함몰부가 있고 주변 부위가 특히 stomach 쪽으로 융기되어 있음.
진단: GE junction cancer
[이준행 comment]
어려웠겠지만 매우 중요한 문제입니다. 이 문제에 대해서는 답변자의 절반 이상이 식도암을 의심하지 못하고 역류성 식도염으로 진단하였습니다. 하부식도의 squamous epithelium이 깨진 것 같으니 바렛식도로 오인한 분도 많았습니다. 그러나 GE junction cancer였습니다. EG junction 암은 adenocarcinoma인지 squamous cell carcinoma인지의 구분이 어렵고, 수술해보면 생각보다 깊은 경우가 많습니다. 이 환자도 진행성 식도암이었습니다.
Esophagus and upper stomach, Ivor Lewis operation:
Invasive squamous cell carcinoma, moderately differentiated, gastroesophageal junction:
1) tumor size: 2x1.5 cm
2) extension to perimuscular adventitia
3) extension to stomach
4) endolymphatic tumor emboli: present
5) perineural invasion: not identified
6) negative resection margins (proximal, 7.5 cm; distal, 5.5 cm)
7) metastasis to one out of 33 regional lymph nodes선생보다 description을 더 잘하는 제자들이 많습니다. 감사한 일입니다.
식도암과 sentinel polyp을 동반한 역류성 식도염의 감별진단은 매우 어렵습니다. 참고로 아래 증례는 sentinel polyp을 동반한 역류성 식도염이었습니다. 참 어렵습니다.
* 참고: EndoTODAY 위식도접합부암
[2017-10-15. 전공의 질문]
37번 증례의 esophageal mucosa가 정상에 비하여 더 짙고 지저분하다 생각되어 검색하던 중 squamous hyperplasia라는 표현이 있음을 알게 되었습니다. 이 경우에 적용해 볼 수 있는 것이라고 생각하시는지요? 또한, 이 정도라면 hiatal hernia라던가, GERD라고 보는 것은 부적절할까요? 고민하다 우선 뚜렷하다 생각되는 진단명만 붙였습니다.
[2017-10-16. 이준행 답변]
질문 주셔서 감사합니다. 그렇습니다. 하부 식도의 점막이 정상에 비하여 dirty white non-transparent 하지요? 그리고 Z-line이 hiatal opening 위치보다 아주 조금 올라온 부위가 있고, 하부 식도의 내강이 정상에 비하여 다소 넓어보이는 것 맞습니다. 흔히 이야기하는 2 cm 기준에 미치지 못하지만 약간의 hiatal hernia 있는 것 맞습니다. Short segment hiatal hernia라고 부르기도 합니다. GERD와 약간 관련도 있지만 너무 주관적이라 정식 진단명으로 사용하지 않고 있을 뿐입니다.
약간의 hiatal hernia가 있고 위내용물 역류가 오래되면 하부식도 점막이 dirty white non-transparent 하게 변합니다. Irregular Z-line 상방의 하부식도가 이렇게 변한 것을 과거에 minimal change의 하나로 언급하곤 했습니다만, 이 또한 너무 주관적이라 정식 진단명으로 사용하지 않고 있습니다. 전형적인 mucosal break를 가진 미란성 식도염 사진을 보면 longitudinal mucosal break 바로 옆 점막 혹은 하부식도 점막이 전반적으로 dirty white non-transparent 하게 변해있는 것을 알 수 있습니다. 다 비슷한 현상입니다. 위내용물의 반복적 역류로 인하여 식도 점막이 비후된 것이지요.


요컨데 이 환자는 위식도접합부 암은 틀림없는데, short segment hiatal hernia와 만성 역류로 인한 하부식도 점막의 경한 비후가 있는 것도 맞습니다. 내시경 결과지에 우선 뚜렷하다고 생각되는 것만 쓰는 것은 좋은 일입니다. 임상적으로 의미있는 것에 집중해야 하니까요. 그러나 사진을 잘 보면 글로 쓰지 않았더라도 많은 이야기가 담겨 있습니다. 그래서 결과지만 보지 말고 늘 사진도 함께 보자고 이야기 하는 것입니다.
[2017-11-9. 이준행 comment]
전공의 3년차 대상 description exercise를 하고 있습니다. 37번 문제과 38번 문제는 다들 어려워합니다. 그래서 조금 자세히 답변을 붙여 보았습니다.
 증례 38 (history of massive hematemesis)
증례 38 (history of massive hematemesis)
소견: 위체상부에 작은 미란(혹은 얕은 궤양)이 있고 그 중앙의 exposed vessel이 보임. 내시경을 처음 넣었을 때는 bleeding이 보이지 않다가 공기를 넣으면서 이리 저리 돌리는 과정에서 갑자기 우측과 같은 출혈이 발생함.
진단: Pumping bleeding from Dieulafoy lesion (or ulcer), Forrest classification Ia
[이준행 comment]
[2020-3-15. F1 질문]
Healing ulcer 에 혈관이 노출되는 경우가 있는지요? 뭔가 correlation이 안되는 듯한 느낌이 듭니다.
[2020-3-15. 이준행 답변]
좋은 질문입니다. 큰 ulcer가 있다가 healing 된 것이 아닙니다. (원인이나 결과인지 알 수 없으나) 처음부터 작은 점막 defect가 생겼는데 그 아래의 큰 혈관이 노출되어 피가 pumping하는 condition입니다. Dieulafoy라고 부르는 드문 상황입니다.
Proximal stomach의 작은 erosion이 있고 이로 인하여 굵은 혈관이 노출된 형태입니다. Dieulafoy lesion이라고 부르는 것입니다. 관례적으로 Dieulafoy ulcer라고 부르기도 합니다. 아래 민영일 교수님의 orange book을 참고하시기 바랍니다.
내시경 검사를 하던 도중 exposed vessel에서 갑자기 blood pumping이 관찰된 경우입니다. 내시경 검사를 위하여 공기를 주입하면 그 때문에 출혈이 조장될 수 있습니다. 아슬아슬한 상황이였기 때문에 약간의 자극만으로도 이런 일이 생기는 것입니다. 어짜피 아슬아슬한 상황 (Forrest IIa)이나 확식한 출혈 (Forrest Ia)이나 치료 원칙은 동일합니다. 이런 경우 Forrest 분류를 어떻게 써 줄 것인가 고민인데요... 저는 보통 심했던 상황으로 기술하도록 권하고 있습니다. 이 환자는 Ia가 되겠네요.
Dieulafoy ulcer bleeding은 band ligation, clipping, electrocauterization 모두 가능합니다.
Heart failure로 clopidogrel 등을 드시고 계신 분의 심한 Dieulafoy ulcer bleeding이었습니다. Injection 후 electrocauterization으로 지혈하였습니다.
 증례 39 - 원인이 명확하지 않은 recurrent upper GI bleeding의 과거력이 있는 분의 십이지장 소견입니다.
증례 39 - 원인이 명확하지 않은 recurrent upper GI bleeding의 과거력이 있는 분의 십이지장 소견입니다.
소견: 십이지장 구부와 제2부에 5 mm 이하의 multiple erosion들이 scattered 되어 있다. Shallow erosion은 margin은 irregular 하나 비교적 명확하고 whitish exudate 로 덮혀있고 일부는 hematin 이 동반되어 있다.
진단: Erosive duodenitis (Zollinger- Ellison syndrome, most likely)
[이준행 comment]
내시경 소견만 볼 것이 아니라, 주어진 임상 소견('원인이 명확하지 않은 recurrent upper GI bleeding의 과거력')을 함께 고려하면 Zolling-Ellison syndrome을 의심할 수 있었겠지요. Vasculitis such as H-S purpura 정도를 추가로 고려해 볼 수 있겠느나 가능성은 떨어집니다.
이 환자는 pancreas body에 mass와 간전이가 있었습니다. Gastrin이 1000 pg/ml 이상으로 높았습니다. 아래는 또 다른 Zollinger Ellison syndrome 1예입니다.

선생님께서는 r/o vasculitis라고 추가하셨는데요, 이 또한 excellent한 선택입니다. 사실 다발성 십이지장 미란에서 반드시 감별해야 할 것이 Henoch Scholein purpura입니다. 일전에 EndoTODAY에 이런 증례를 소개한 바 있습니다.
16세 남학생의 전형적인 HS purpura였는데 내시경 집담회에 증례로 올라왔습니다. 아무런 설명도 없이 아래 사진 한 장만 달랑 올라왔습니다. 발진이 있었다는 정보가 없었는데... 어떤 선배 의사께서 바로 HS purpura를 맞추셨습니다. HS purpura는 vasculitis이기 때문에 십이지장 점막에 지저분한 궤양이 산재되어 있더라도 그 사이 점막은 비교적 정상이라는 것입니다. 특징적인 소견이지요. 물론 깊은 궤양이 아닐 수도 있습니다. 자주 보고 많이 보면 딱 보면 알게 되는 그런 병입니다.
* 참고: EndoTODAY H-S purpura
소견: 위각 직하방 proximal antrum에 1.5 cm 가량의 궤양이 관찰된다. Edge는 sharp하고 margin 은 edematous, erythema 가 동반되어 있고 deep base는 dirty exudate 와 mucosal friability 소견이 보인다. 오른쪽은 ulcer 깊이가 좀더 얕아지고 margin의 edematous mucosa의 경사가 좀 더 완만해 진 상태로 조금 더 Healing 된 것으로 보인다.
진단: benign gastric ulcer, A2 (r/o recurrent ulcer)
[이준행 comment]
DEX workshop에 참여 후 지속적으로 DEX quiz 문제를 풀면서 공부하고 있는 한 가정의학과 전공의의 답변에 comment를 붙였습니다. DEX workshop을 열었는데 막상 내과, 외과 의사들은 바빠서인지, 관심이 없어서인지, 나중에 배울 기회가 많다고 생각해서인지 참여율이 저조합니다. 오히려 전국 각지의 가정의학과 의사들이 많이 오고 계십니다. 내과, 외과 전공의들에게 배움의 기회를 제공하였으나 알 수 없는 이유로 참여율이 저조한 점은 참으로 안타깝습니다. 근무시간을 줄여주고 공부할 시간을 드리면 더 좋겠으나 세상일이 그리 쉽지 않습니다. 그래서 주말과 야간에 공부하기를 권했는데, 역시 학생 생각은 선생 생각과 다른 모양입니다. 저도 노땅이 된 모양입니다. 기회가 늘 있는 것이 아닌데.... 여하튼 좀 더 기다려보려고 합니다. "아님 말고..." 이게 저의 전략입니다. (2018-11-28. 이준행)
추적관찰에서는 아래 사진과 같이 완전히 healing 되었습니다. Recurrent ulcer입니다. Active stage ulcer인데 비하여 주변이 단단해 보입니다. Fold도 이상하구요. BGU 같기는 한데 ulcer crater의 stage와 주변 점막의 stage가 일치하지 않으면 recurrent ulcer를 생각하시기 바랍니다. 과거에 궤양이 아물면서 deformity를 만들었는데 여기에 다시 active ulcer가 생긴 것이라고 보면 이해가 될 것입니다.
아래와 같은 흥미로운 질문이 있었습니다.
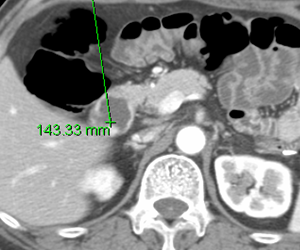
소견: 위체하부부터 fundus 일부까지 위점막 주름이 매우 두꺼워져있고 일부는 융합되기 시작하였음. 두꺼워진 주름 사이의 골짜기 부분은 좁고 얕아졌음. 두꺼워진 주름의 표면은 mozaic pattern의 점막을 보임. 위체상부 후벽은 3-4 cm 부위의 함몰부가 발생하고 있음. 위는 비교적 잘 펴짐.
진단: AGC, Borrmann type IV
[이준행 comment]
이 문제에 대하여 어떤 분께서 hypertrophic gastritis를 첫번째 impression으로 주셨기 때문에 다음과 같은 comment를 했습니다.
틀렸습니다. 보만 4형 진행성위암이었습니다. 절대로 틀리면 안 되는 증례입니다. 20대 여성이었습니다. 수술을 하였고 AGC, signet ring cell carcinoma, 17 x 12 cm, subserosa, LN 2/42로 나왔습니다.
Fold 간 편차가 있고 주름 사이의 위벽은 얇게 보존되어 있으면 비후성 위염을 의심하는 것은 맞습니다. 그러나 이 정도면 fold간 편차가 적은 편이고 주름 사이의 골짜기가 두꺼워진 주름에 의하여 거의 obliteration된 양상입니다.
2020-8-10. 8PM. EndoTODAY on Air
보만 4형 진행성 위암은 매우 어렵습니다. 비후성 위염보다 10배는 흔하다고 생각됩니다. 보만 4형 진행성 위암인지 비후성 위염인지 구분이 어려운 상황에서는 젊은 여자, 체중이 빠진 환자, 반년 이내에 증상이 발생한 환자라면 거의 보만 4형 진행성 위암으로 보면 틀림없습니다.
많은 분들이 r/o Borrmann type IV와 같은 impression을 주셨습니다. 그러나 이 정도면 너무나 확실함 보만 4형 진행성 위암입니다. "r/o"은 빼도 좋겠습니다. 아니 빼는 것이 좋겠습니다.
보만 4형 진행성 위암에 대해서는 EndoTODAY 20130210 부터 ENdoTODAY 20130405에서 상세히 논의하였으니 참고하시기 바랍니다.
보만 4형 진행성위암의 경계 판정은 매우 어렵습니다. 정상으로 보인 점막도 사실 암인 경우가 많기 때문입니다.
소견: 십이지장 제 2부 내측의 ampulla of Vater 상방으로 직경 1.5 cm 가량의 outpouching한 opening이 보임. 방이 형성되어 있다.
진단: Duodenal diverticulum
* 참고: EndoTODAY 십이지장 게실
 [EndoTODAY Weekly Seminar 다시보기 (2024년)]
[EndoTODAY Weekly Seminar 다시보기 (2024년)]
 2024-28. 날문 위암. Pyloric ring cancer
2024-28. 날문 위암. Pyloric ring cancer
ECR 022. 2024-12-26.
 2024-27. Description exercise 예제 4문제 해설
2024-27. Description exercise 예제 4문제 해설
우리나라에서 내시경을 배우는 것은 무척 어려운 일입니다. 질 좋은 curriculum이 많지 않기 때문입니다. 가장 표준적인 curriculum은 인턴 1년, 내과 전공의 3년 후 소화기내과 fellow 2년을 하는 것이지만 모든 분들에게 이 과정이 열려있는 것도 아닙니다. 게다가 2024년 2월 불거진 의정사태로 인하여 어렵게 운영되던 많은 과정들이 중단된 것도 안타까운 일입니다. 오호통재라...
제가 일본에서 ESD를 배울 때 제법 많은 일본 내시경실을 방문한 적이 있습니다. 당시 놀랐던 점은 내시경실에 의사들이 매우 많다는 점이었습니다. 우리나라에서는 간호사가 assist를 하는 경우가 많지만 일본에서는 젊은 의사들이 assist를 합니다. 내시경 준비도 하고, 조직 겸자도 잡고, ESD를 할 때 옆에서 이런 저런 것을 돕습니다. 이 과정을 통하여 비록 자신이 직접 내시경을 해 본 적은 없으나 선생님의 시술을 수십번 수백번 보면서 모든 상황에 익숙해집니다. 그리고 1년 쯤 후 처음 내시경을 잡게 되는데 이미 눈으로, 머리로 모두 익힌 상황이므로 술기를 금방 배우는 것을 보았습니다. 참 부러운 광경이 아닐 수 없습니다.
저는 우리나라에서 그래도 내시경 검사를 많이 했던 소위 내시경 전문가입니다. 그런데 늘 혼자입니다. 도무지 보러 오는 사람이 없습니다. 어쩌다 fellow들이 잠시 기웃거리는 경우가 있지만 보통은 혼자입니다. 가르치고 싶어도 배우러 오는 사람이 없습니다. 일본에서는 저와 비슷한 경력을 가진 내시경 선생이 시술을 하면 이 병원 저 병원에서 많은 분들이 찾아와 observation을 합니다. 소속 기관에서 보내는 경우는 거의 없는 것 같고 스스로 개인 휴가를 내서 선생을 찾아다니는 것이라고 합니다. 이러한 과정을 통하여 소위 내시경 고수들의 술기를 보고 고수들과 이야기를 하면서 스스로의 실력을 키우는 것입니다.
우리나라에서도 내시경을 하는 분들이 다른 병원의 내시경 시술을 많이 참관하는 문화가 되었으면 좋겠습니다. 개인 휴가를 쓰십시오. 휴가내서 경험이 많은 선생님들 찾아가 observation을 하십시오. 그래야 실력이 늘지 않겠습니다. 술기는 혼자 끙끙댄다고 향상되는 것이 아닙니다. 개인 휴가를 쓰십시오. 교육에 인색한 우리나라에서 조직이 나를 위해 교육 기회를 줄 것을 기대하지 마십시오. 개인 휴가를 내고 고수들을 찾아다니는 것이 유일한 해법입니다. 왜 맛집 tour는 하면서 내시경실 tour는 하지 않는 것입니까? 두드리십시오.
 2024-26. 자가면역위염. Autoimmune gastritis.
2024-26. 자가면역위염. Autoimmune gastritis.
 2024-26. EGC IIa 5.5cm near cardia
2024-26. EGC IIa 5.5cm near cardia
 2024-23. Submucosal invasion in forceps biopsy + Lecture dropout
2024-23. Submucosal invasion in forceps biopsy + Lecture dropout
 2024-22. ESD for EGC (2024 KAMA scientific convention)
2024-22. ESD for EGC (2024 KAMA scientific convention)
2024-21. 하부식도선암과 림프절명명법. Lower esophageal adenocarcinoma
2024-20. Post-colonoscopy surveillance. 임상강사 오영은
2024-19. ESD complication (pneumonia) and atypia
2024-18. 십이지장궤양출혈 증례토의. Duodenal ulcer bleeding
2024-17. Presidential Lecture at KINGCA WEEK 2024. Endoscopy and gastric cancer
2024-16. Endoscopy open education with EndoTODAY and ESD hands-on training
2024-15. Gastric MALToma treated by RT
저는 아낌없이 주는 선생입니다. 사랑하는 학회로부터 아낌없이 주지는 말라는 경고를 받은지 3주째입니다. 그렇다고 아껴가며 줄 수는 없는 일 아니겠습니까. 선생이라는 직업의 業의 특성이 원래 '배워서 남주는 것'일진데 어찌 아끼라는 말입니까. 그래서 그냥 원래 하던대로 하기로 했습니다. 계속 아낌없이 주겠습니다.
이제 마음 속의 태풍도 조금씩 가라앉고 있습니다. 이런 경우 공자는 도움이 되지 않았습니다. 역시 노자입니다.
위 MALT 림프종에 대한 상세한 증례토의입니다. 도움이 되기 바랍니다.
2024-14. 2024년 대한소화기내시경학회 징계 사태도 2주가 되었습니다. 정신을 차리고 다시 원래의 모습으로 돌아가려고 합니다. 그래서 교육 자료를 하나 만들었습니다.
2024-13. 쑥스럽지만... 환자안전제도 공헌 유공자 표창을 받았습니다.
[동문소식] 횡문근융해증
2024-12. Case Reviews in Gastroenterology 창간호
2024-11. 알쏭달쏭 Q & A 퀴즈 (6회)
2024-10. BOXIM simulator 훈련 2024년 신규 녹화
2024-9. The 6th SMC-MNCC joint symposium 1. Rare complications of ESD (TS Kim), 2. Pitfalls in pathologic evaluation of ESD specimen (SM Ahn), 3. Follow up strategy after endoscopic treatment for early gastric cancer (BH Min), 4. Interesting Mongolian cases (Amarbat, Mongolian National Cancer Center), 5. Interesting Korean cases (JH Lee)
2024-8. 위식도역류질환과 식도열공탈장
2024-7. 하이닥 인터뷰. 위암과 위내시경
2024-6. 알쏭달쏭 Q & A 퀴즈 (5회)
2024-5. 역류성 식도염
2024-4. 소화기와 호흡기의 만남 (닥터빌)
log-in 필요. 현장 스케치
2024-3. 자가면역위염 (김태세)
- 토론
2024-2. 1차 진료 시 절대 놓치면 안 되는 위내시경 소견 및 증례
2024-1. 비온뒤 강연. 저용량 아스피린과 비스테로이드소염제를 복용하는 환자의 위궤양 치료 
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.