 [위선암과 위암의 내시경 치료]
[위선암과 위암의 내시경 치료]EndoTODAY | EndoATLAS | Outpatient Clinic
Parasite | Esophagus | Stomach | Cancer | ESD
Home | Guide | Author | Search | Blog | Links
1. Introduction
4. 내시경 치료의 적응증
8. 퇴원 처방시 주의점
9. 시술 후 환자 주의사항
10. 영양 가이드라인
위암 치료의 표준은 수술이다. 그러나 모든 수술에는 어느 정도의 morbidity와 mortality가 따른다. 특히 위를 2/3 이상 제거하는 위암수술은 체중감소, dumping syndrome, 식생활 변화의 필요성 등으로 삶의 질을 크게 저하시킨다. 따라서 최근에는 저침습치료(less invasive treatment)에 대한 관심이 높다. 조기위암의 일부, 특히 점막에 국한된 암 (M cancer) 중 크기가 작은 분화암(일본에서는 differentiated cancer로 표현하는 것으로, 국내에서는 well differentiated 및 moderately differentiated type을 포함하는 개념이다)은 림프절 전이의 가능성이 매우 낮으므로 내시경을 이용한 국소치료만으로 완치가 가능하다.
수술한 환자의 lymph node status를 분석하여 림프절 전이가 거의 없는 병소의 특성을 요약한 것이 ESD 적응증이다. 심평원에서는 ESD 인정기준 (시행일자 2012.4.1)에서 "점막에 국한된 궤양이 없는 2㎝이하의 분화형 조기암"을 보험급여기준으로 발표한 바 있다. 이를 conventional indication이라 부른다.
전통적인 적응증을 초과하는 병소, 즉 좀 더 크거나 혹은 궤양이 약간 보여도 내시경치료를 시도하는 경우가 있는데 이를 확대적응증 (expanded indication)이라 부른다. 그러나 아직까지 임상연구결과는 부족하여 확대적응증을 폭 넓게 받아들이기는 힘들다. 너무 고령이거나 타 질환으로 인하여 전신상태에 문제가 있는 경우 등 수술 위험성을 고려하여 조심스럽게 ESD를 시도해 볼 수 있다고 생각한다.
적응증(indication)과 판정기준(criteria)을 구분해야 한다. 2013년 현재 가장 많은 의료기관에서 택하고 있는 전략은 conventional indication("점막에 국한된 궤양이 없는 2㎝이하의 분화형 조기암")을 기준으로 ESD candidate를 선택하여 시술한 후, 최종병리결과를 판정할 때에는 expanded criteria를 고려하는 것이다. 즉 시술전에 비하여 시술 후 minute한 submucosal invasion이 있거나, 병리학적 궤양이 있거나, 2cm보다 약간 크거나, 미분화요소가 조금 섞여있더라도 추가수술을 하지 않고 조심스럽게 경과관찰하는 전략이다.
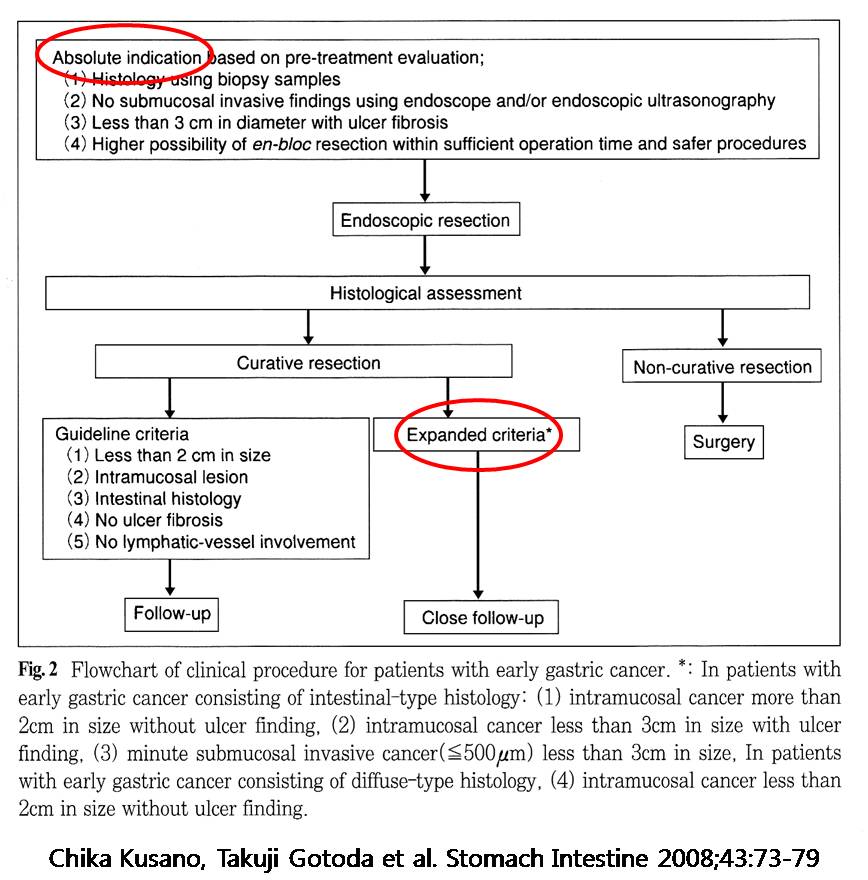
일본에서 제안된 표. 적응증의 표준을 3cm로 잡고 있다는 점을 제외하면 우리와 동일함.
ESD 시술에 있어서 환자 및 보호자의 이해와 동의는 필수적이다. 환자와 보호자에게자세히 설명을 하고 동의를 구한 후 ESD을 시행하는 것이 원칙이다 ("informed consent"). 간혹 심한 간기능부전, 폐기능부전, CVA 등으로 인하여 개복 수술을 시행하는 것이 거의 불가능한 환자가 ESD을 위해 의뢰되는 경우도 있다. 그러나 ESD은 수술을 통해서만 해결할 수 있는 합병증이 가능한 시술이므로, 수술의 definite한 contraindication인 환자는 ESD의 definite한 contraindication으로 생각하는 것이 좋다. 수술에 따른 위험성이 높으나 definite한 contraindication은 아닌 환자에서는 ESD를 조심스럽게 시행할 수 있다.
위암에 대한 개복수술은 일부의 예외적인 경우를 제외하면 대부분 1회의 수술로 모든 치료가 종료된다. 그러나 ESD를 시행한 후 병리결과에 따라서 추가적인 시술이 필요한 경우가 많다. 통상 절제된 병리조직에서 SM1(500 micrometer)을 초과하는 submucosal invasion이 있는 경우, poorly differentiated type의 조직형, lymphovascular invasion 양성의 경우는 수술을 권하고 있다. Resection margin 양성만 문제이고 다른 이상이 없는 경우는 내시경 절제술이나 내시경 소작술을 추가하는 것으로 수술을 대신하기도 한다.
조기위암으로 ESD를 시행한 환자의 10-15%에서 ESD 후 수술이 필요하다. 따라서 ESD를 시행하기 전 환자 및 보호자에게 시술이 잘 되었더라도 병리결과에 따라 수술이 필요한 경우가 있음을 명확히 이해시켜야 한다. 환자가 이해하기 쉬운 방법은 "뿌리가 깊은 경우 수술을 하셔야 합니다. 그런 경우가 7명 중 1명입니다"라고 설명하는 것이다.
위암에 대하여 치료를 받은 후에는 경과관찰이 필요하다. 수술을 시행한 경우도 마찬가지이지만 내시경을 시행한 경우에는 좀 더 짧은 간격으로 추적관찰 검사를 하는 것이 일반적이다. 이는 병소만 제거되었고 위가 그대로 남아있으며, lymph node에 대한 치료가 이루어지지 않았기 때문이다. 추적관찰시에는 통상 내시경, CT, chest X-ray가 시행된다.
[참고문헌]
1) 국내 최초 조기위암 내시경치료 다기관연구 (김재준. Gastrointest Endosc 2007)
2) Outcome after ESD for EGC in Korea (이준행. World J Gastroenterol 2011)
3) 삼성서울병원 ESD 근간 성적 (Dig Liver Dis 2009)
4) 삼성서울병원 ESD 근간 성적 (Surg Endosc 2011)
5) 국내 타병원 ESD 근간 성적 (GIE 2011)
이형성(dysplasia)는 원래 "developmental abnormality"라는 사전적 의미가 있으나, 병리학적으로는 "unequivocal neoplastic transformation"을 뜻하며, 대부분 전암성 병소로 간주된다. 위 이형성(gastric dysplasia)도 위암의 중요한 전구병소이다. 이형성은 병리학적으로 저도이형성(low grade dysplasia)과 고도이형성(high grade dysplasia)으로 나누어진다.
이형성과 혼동되는 개념으로 선종(腺腫, adenoma)이 있다. 선종은 서구와 일본에서 약간 다른 개념으로 사용되고 있어 더욱 혼란스럽다. 서구에서는 이형성 중에서 융기형만을 선종이라고 부르는 반면, 일본에서는 융기형, 평탄형, 함몰형의 이형성을 모두 선종이라고 부른다. 우리나라에서도 융기형, 평탄형, 함몰형의 이형성을 모두 선종으로 부르는 것이 일반적이다. 즉 "dysplasia=adenoma"로 생각해도 크게 무리가 없다. 본 병원의 조직병리 결과는 아래와 같은 방식으로 보고되고 있다. 즉 high grade dysplasia는 언급하고, low grade dysplasia는 생략하고 있다.
이형성은 중요한 전암성 병소(precancerous lesion)로 간주되지만, 내시경으로 절제하면 암으로 진단이 바뀌는 경우가 많다. 즉 forcep biopsy로 얻은 조직에서는 이형성으로 진단이 되지만, EMR/ESD로 전체 병소를 얻어 관찰하면 암으로 진단되는 예가 있다. Low grade dysplasia에서 EMR/ESD 후 암으로 진단이 바뀌는 경우는 5% 미만이지만, high grade dysplasia에서는 20-30%에서 암으로 진단이 바뀐다. 따라서 dysplasia에 대한 내시경 치료 후에는 최종 병리결과를 확인하는 것이 매우 중요하다. 아울러 환자에게도 사전에 진단이 바뀌는 경우가 적지 않음을 설명해 주어야 한다.
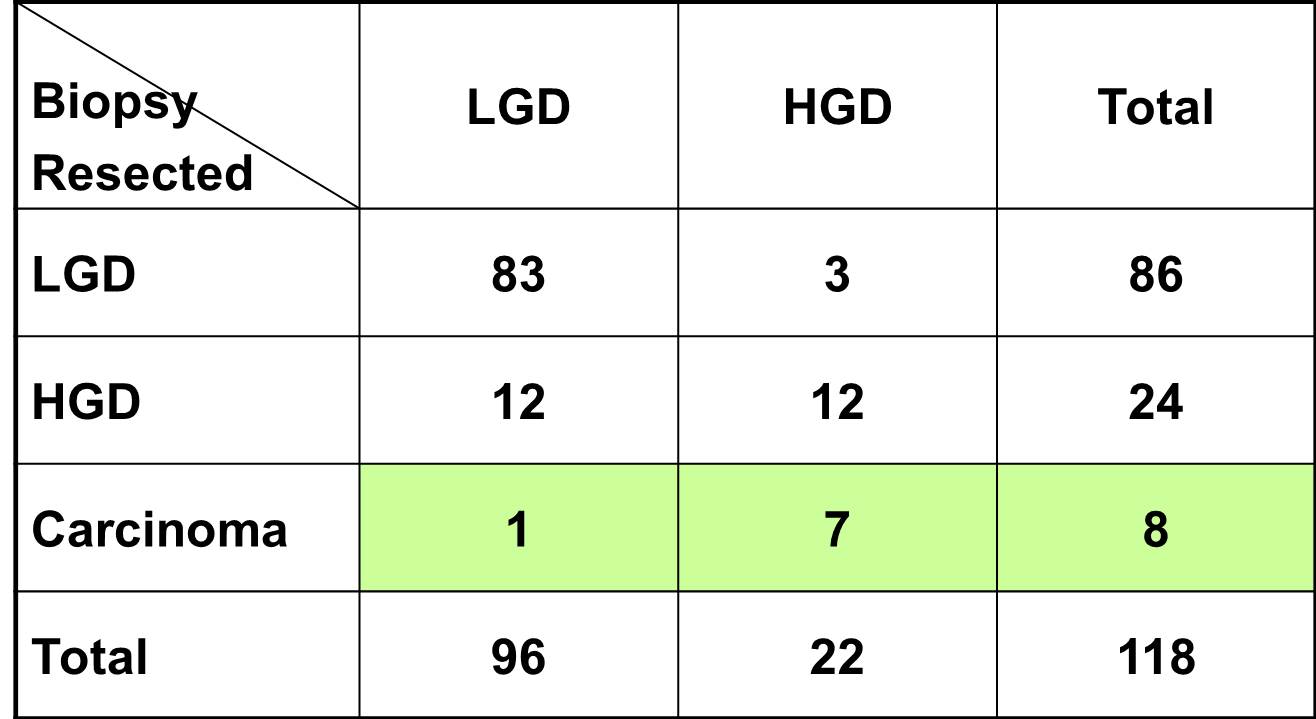
위 선종의 일부는 EMR 후 위암으로 진단이 바뀐다 (출처: Endoscopy 2001).
[참고문헌]
1) 위이형성의 진단과 치료 (text, 이준행 씀)
2) Gastric dysplasa (Powerpoint PDF)
둘 다 내시경으로 점막병소를 자르는 치료(endoscopic resection, ER)의 일종이다. 병소의 하단을 절제한다는 기본 원리는 동일하다. Endoscopic resection의 기법은 매우 다양한데, EMR-P (EMR with precutting)와 ESD (endoscopic submucosal dissection)가 주로 사용된다.
EMR-P는 needle knife나 IT knife 등을 이용하여 병소 주변을 360도 cutting 한 후, snare를 이용하여 병소 하단의 점막하조직을 절제하는 방법이다.

EMR-P (endoscopic mucosal resection with precutting)
ESD는 EMR-P와 마찬가지로 병소 주변을 360도 cutting한 후, snare를 이용하지 않고 needle knife나 IT knife를 이용하여 점막하 조직을 직접 dissection 하는 방법이다. ESD방법은 EMR-P에 비하여 큰 병소를 en bloc resection 할 수 있다는 장점이 있으나, 시간이 오래 걸리고 합병증 발생률이 높다는 단점도 있다. 병소에 따라서는 일부 submucosal dissection 한 후 snare로 resection 하기도 한다.
최근 국내에서는 EMR과 ESD를 서로 다른 시술법으로 간주하는 경향이다. 이는 ESD가 기존의 conventional EMR에 비하여 난이도가 높고 (숙련에 긴 시간이 소요됨), 시술시간이 길고, 보조 인력이 많이 필요하며, 기구와 장비가 상당부분 다르기 때문이다. 이를 통칭하여 endoscopic resection (ER)으로 부르기도 한다 ("ER = EMR + ESD").
[참고문헌]
2) EMR-P와 ESD 비교 (민병훈. Dig Liver Dis 2009)
4-1. Indications of EMR/ESD for EGC
1) Confined to the mucosal layer: 이 항목은 다소 주관적인 기준이다. 내시경 육안소견을 통하여 M cancer인지 SM (submucosal) cancer인지를 정확히 구분하기 어렵기 때문이다. 많은 내시경 경험을 통하여 암의 depth of invasion을 예측하는 능력을 키울 수 밖에 없다. EMR/ESD 시술 전에 EUS를 통하여 depth of invasion을 평가하기도 하지만, minute한 submucosal invasion은 EUS를 통해서 진단하기 어렵기 때문에 EMR/ESD 전에 EUS를 시행하는 것은 필수적이지 않다. 필자는 EMR/ESD전 EUS를 시행하지 않고 있다.
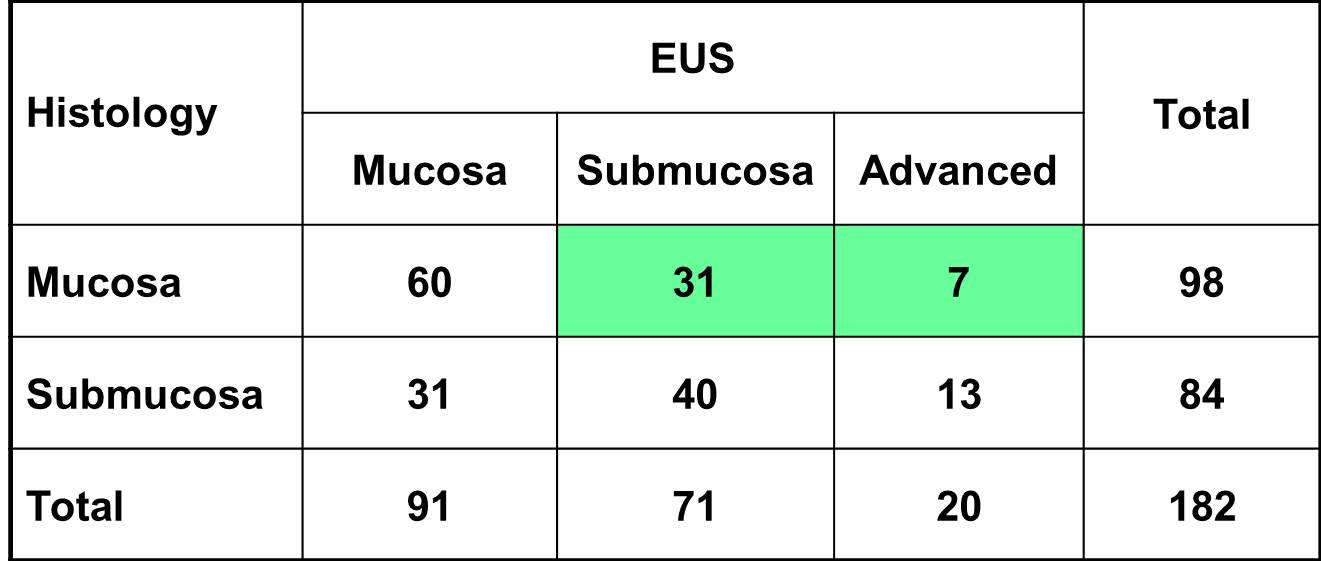
EUS를 이용하여 점막암과 점막하암을 구분하는 것은 용이하지 않다 (출처: Nakamura. Cancer 1999;85:1500-1505).
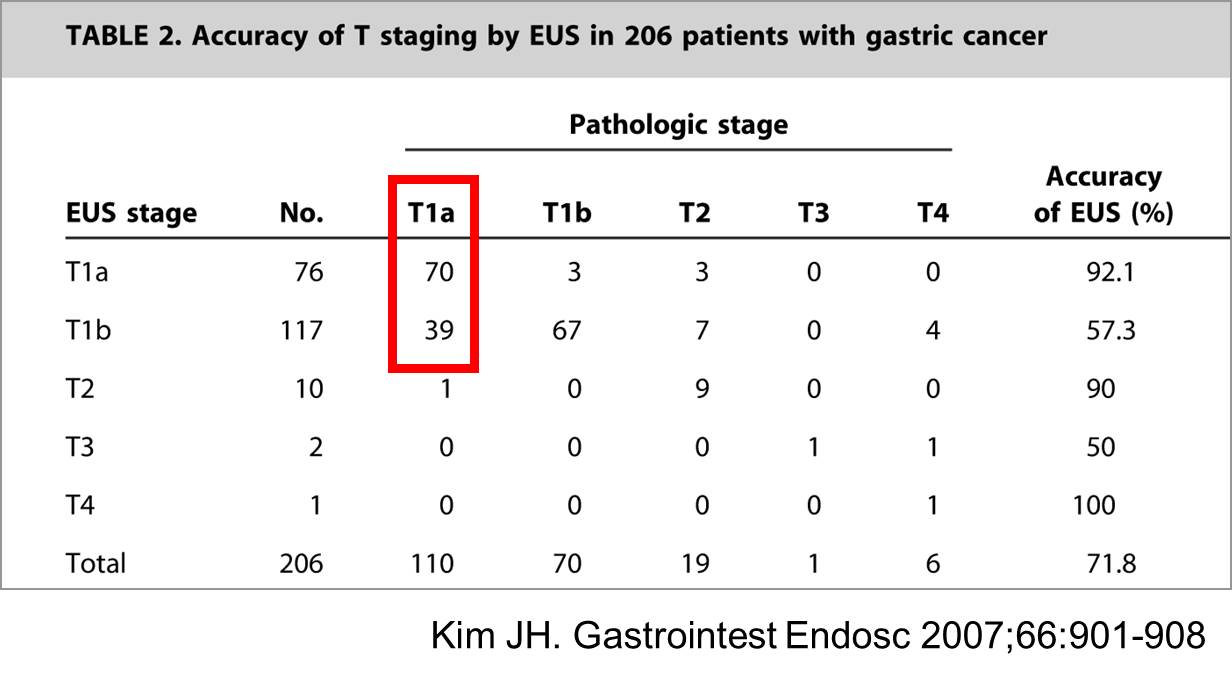
Over-staging of the mucosal cancer is still a big problem.
2) Well differentiated or moderate differentiated adenocarcinoma
3) Less than 2-3 cm for the elevated lesion: 크기 기준은 다소 유동적이다. 함몰형에서는 크기 기준을 좁히는 전문가도 있다. 점막암이 강력하게 의심되는 경우에는 크기 기준을 다소 초과한다고 하더라도 EMR/ESD를 시행하기도 한다.
4) Without ulcer: ulcer가 있는 경우는 submucosal invasion이 흔하므로 ulcer는 EMR/ESD의 contraindication으로 간주된다. 그러나 내시경으로 ulcer인지 erosion인지를 정확히 평가하기 어렵다는 한계가 있다.
5) Stomach CT or chest X-ray: no evidence of distant metastasis or LN involvement
4-2. Indications of EMR/ESD for gastric adenoma with or without high grade dysplasia
일반적으로 위암의 전구병변으로 간주되는 선종(腺腫, adenoma)은 모두 (크기 및 모양에 제한이 없음) EMR/ESD의 적응증으로 간주한다. 그러나 일부 큰 선종은 EMR/ESD시술 후 위암으로 진단이 바뀌는 경우가 많기 때문에 시술 전에 환자 및 보호자에게 이 점을 명확히 설명해 둘 필요가 있다.
[초창기에는 4박 5일 CP를 사용했습니다]
1) Grossly complete resection (by the endoscopist): 시술의사가 종양이 모두 제거되었다고 판단하는 것은 complete resection으로 판정하는 기본이다.
2) En-bloc resection (or complete reconstruction in piecemeal resection cases)
3) Well or moderately differentiated histology: 다른 조건은 모두 complete resection이지만 cell type만 문제인 경우는 경과관찰을 하는 예도 있으므로, 반드시 staff와 상의한다.
4) Limited to the mucosal layer: muscularis mucosa (점막은 epithelial layer, lamina propria, muscularis mucosa의 3 층으로 구성되어 있다) 까지 침윤된 경우는 점막암이다. 500 micrometer (=0.5 mm)이하의 점막하층 침윤(SM1이라고 부른다)에서는 보통 수술을 권하지 않고 경과관찰을 한다. 500 micrometer를 초과하는 경우는 원칙상 수술을 한다. 500 micrometer 이하의 침윤이라도 종양이 2 cm 이상이거나 궤양이 있거나 기타 상황에 따라 수술을 권하기도 한다.
5) Resection margin (-): 점막암이고 lateral margin이 한 두 방향에서만 양성이면 추가적인 ESD 혹은 ablation을 하기도 한다.
6) No vascular invasion
7) No lymphatic invasion
[참고문헌]
1) Surgical outcome after incomplete ESD (삼성서울병원의 경험, Br J Surg 2011) - The incidence of residual tumour in the surgical specimen was 24·6 per cent after incomplete ESD.
[Treatment outcome based on pretreatment diagnostic groups]
7-1. 출혈
1) 출혈의 빈도와 출혈 시기: EMR/ESD 후 출혈은 hematemesis나 melena로 나타난다. 출혈은 시술 3일째까지 흔하다. 그 이후 발생하는 출혈은 많지 않다. 출혈의 빈도는 3-10% 정도이다. 짜장면(옛날 짜장보다는 간짜장에 가깝다)과 같은 black tarry stool, 갑작스러운 식은땀, 현기증, palpitation 등이 출혈의 증상이라는 점을 환자에게 미리 교육해두면 좋다. EMR/ESD 시술 후 melena 여부를 확인하기 위하여 환자에게 변 색깔을 묻게 되는데, 이 때문에 환자들이 불필요한 불안감을 가지는 경우가 있다. 따라서 변을 보지 않아도 아무 문제가 없다는 점을 사전에 알려주면 좋다.
2) 출혈시 초기 대응: 출혈이 발생하면, vital sign을 확인하고, 생리식염수를 주사하면서 혈액검사를 한다. 소화성궤양 출혈에 준하여 고용량 PPI를 사용한다 (80mg loading 후 시간당 8 mg 3일간 continuous infusion). 필요시 혈액을 준비하고 꼭 필요하다고 판단되면 수혈한다. 불필요한 수혈은 피한다. 불필요한 수혈을 하는 것보다 준비한 피를 버리는 편이 낫다.
3) 응급내시경: 아무리 늦은 시간이더라도 병동에서 혼자 환자를 manage하지 말고 즉시 담당 임상강사나 staff에게 보고한다. 출혈양이 많으면 빨리 내시경 검사를 한다. 소량의 melena만 보인 환자는 (1) 증상이 없고, (2) 활력증후가 안정적이고, (3) hemoglobin 감소폭이 2 이하면 내시경 없이 고용량 PPI만 투여하면서 경과관찰할 수 있다.
4) 퇴원 후 출혈: 드물게 퇴원 후 출혈하는 경우가 있다. 정확한 빈도는 알 수 없지만 300명에 한명으로 설명하고 있다. Hematemesis 환자는 대부분 병원을 방문하지만, melena 환자는 병원을 찾지 않기도 한다. 환자에게 melena도 출혈의 증상임을 사전에 설명하는 것이 좋다.
5) 항혈소판제와 항응고제: 내시경 조직검사 전에는 아스피린이나 clopidogrel을 끊지 않는다 (SMC guideline: 고위험환자의 조직검사). 그러나 EMR/ESD 시술 전에는 3-4일 정도 약제를 중단하는 예가 많다. 최근에는 aspirin이나 기타 항혈소판제를 끊지 않고 시술하기도 한다. (관련 EndoTODAY, 관련 국립암센터 논문). EMR/ESD 시술 후 출혈이 없으면 가급적 빨리 항혈소판제를 시작하는 것이 좋다. 시술 전후 아스피린 혹은 클로피도그랠 중단 기간이 총 7일을 넘지 않는 것이 좋다. 항혈소판제를 끊는 기간 동안 CVA나 AMI와 같은 심혈관계 질환이 발생할 가능성이 높다는 점과, 항혈소판제를 다시 시작하는 시점에 출혈하는 경우가 있다는 점을 사전에 설명하는 것이 좋다. 그러나 출혈위험을 지나치게 회피하면 반대급부로 중풍이나 심근경색이 많아진다. 출혈로 사망하는 환자는 드물다. 그러나 중풍이나 심근경색으로 환자가 사망할 위험은 높다.
6) Warfarin 사용 환자들은 항혈소판제 사용 환자보다 심혈관계 위험이 더 높은 경우가 많다. 따라서 individualize할 수 밖에 없다. Warfarin을 처방한 의료진과 상의가 필수적이다 (관련 EndoTODAY).
7-2. 천공
1) Sign of gastric perforation
2) 천공의 종류: EMR/ESD에 의한 천공은 knife에 의한 고유근층(proper muscle layer)의 직접적인 손상 혹은 snare에 의해 고유근층이 포획되어 병변부와 함께 절개됨으써 발생되는데, 그 빈도는 0-5%로 알려져 있다. EMR/ESD에 의한 천공은 크게 두 가지로 나누어진다.
(1) Frank perforation: EMR/ESD 시술 도중 뚜렷한 perforating hole이 발견되는 경우. 과거에는 수술을 시행하는 것이 원칙이었으나 최근에는 대부분의 환자에서 endoscopic clip을 이용하여 즉시 내시경적 치료를 시행할 수 있다.
(2) Micro-perforation: EMR/ESD 시술 도중 뚜렷한 perforating hole이 발견되지 않았으나, 시술 직후에 시행한 chest X-ray에서 복강내 free air가 관찰되는 경우를 말한다. 대부분의 환자에서 내시경적 치료가 필요 없으며, 금식 및 IV 항생제로 치료가 된다 (관련 SMC 논문). 과거에 많이 사용하던 nasogastric tube는 이제는 사용하지 않는다. 복강내 공기가 너무 많으면 바늘로 제거하기도 한다 (EndoTODAY- 복강공기 제거방법).
3) 천공시 대처방법: EMR/ESD의 경험이 축적되면서 frank perforation이나 microperforation의 빈도가 모두 감소되었다. 최근에는 frank perforation보다 microperforation의 빈도가 더 높다. 내시경으로 치료한 frank perforation이나 microperforation의 치료원칙은 동일하다. EMR/ESD 시술 동안 frank perfoation이 있어 clip으로 치료한 경우나, chest X-ray에서 우연히 pneumoperitoneum이 발견된 경우에는 아래와 같이 관리한다.
- 임상강사나 staff에게 즉시 보고한다.
[참고문헌]
1) Management of complications during ESD (전성우. Diagn Ther Endosc 2012)
2) Non-surgical management of microperforation (정규. Digest Liver Dis 2006)
1) 퇴원은 CP에 따라 진행한다. 통상 PPI를 투여하고 2개월 후 추적내시경을 시행한다.
2) 위암에 대한 내시경 치료 후 경과관찰 중 국소재발이나 새로운 위암의 발견으로 인해 수술을 받는 환자가 있다는 점을 환자와 보호자에게 미리 알려드려야 한다. 최근까지의 통계에 의하면 그 확률을 10% 미만이다.
3) 위암 환자에서 대장암의 발견율이 높다는 연구결과가 있다. 퇴원시 환자에게 향후 대장에 대한 검사도 시행할 것을 권하는 것이 좋다. 그러나 대장에 대한 검사는 EMR/ESD 4주 이후로 미루는 것이 바람직하다 (퇴원시 order를 입력할 필요는 없음).
4) EMR/ESD 시술 후 병소가 완전히 호전되기까지는 언제든지 출혈의 위험이 있다는 점을 미리 알려드려야 한다. 통상 1달 이후의 지연출혈은 드물지만, 항혈전제나 aspirin을 복용하는 환자에서는 그 이후에도 출혈하는 예가 있다. 출혈의 증세(혈변, 흑색변, 갑작스런 오한과 기운없음 등)를 미리 알려드리고, 출혈이 의심되면 즉시 가까운 병원을 방문하도록 지도하는 것이 좋다.
1. 내시경 치료 후 일정 기간 출혈 위험이 있습니다. 치료로 인한 궤양이 완전히 치유되기까지 4-8주가 소요되기 때문입니다. 출혈은 피를 토하거나 혈변(붉은 색의 혈변이나 짜장면처럼 검은색의 흑색변), 어지러움증, 갑작스런 땀 등의 증세로 나타납니다. 별다른 증상이 없다가 갑자기 혈압이 떨어지는 쇼크로 나타나기도 합니다. 시술 후 1-2 일 사이에 출혈 위험이 가장 높습니다. 시술 후 1 달 까지는 지연출혈(delayed bleeding)이 가능합니다. 만성신부전이나 간경변 환자인 경우와 항응고제나 항혈소판제를 복용하셨던 환자에서 특히 위험합니다. 병원에 입원해 계시는 동안 나타나는 출혈은 약물요법과 내시경 지혈술로 치료합니다. 간혹 수술이 필요한 경우도 있습니다만 매우 드문 일입니다. 드물게 퇴원 후 집에서 출혈할 수 있습니다. 이때는 가장 가까운 의료기관에서 응급조치를 받으셔야 합니다.
2. 출혈을 예방하기 위하여 시술 당일과 다음날은 금식을 권하고 있습니다. 시술 2일째에는 '미음(아침) - 죽(점심과 저녁)'의 순서로 식이진행을 합니다. 퇴원 후 2일 정도 죽을 드시고 그 이후 밥을 잘 씹어서 드십시요. 시술 후 몇 가지 음식(예를 들어 매우 단단한 반찬 등) 섭취에 주의하십시오. 그러나 일반적으로 음식의 종류와 출혈은 무관합니다.
3. 내시경 치료 후에는 조금 싱거운 균형된 식사를 권합니다.
4. 술은 4주간 금하는 것이 좋습니다.
5. 시술 후 4주 동안은 가급적 장거리 여행을 피하는 것이 좋습니다. (최소한 2주 동안)
6. 퇴원 후 가벼운 일상생활은 가능합니다. 산책, 골프연습장 등 가벼운 운동은 2주 동안 피하고, 테니스, 수영과 같은 힘든 운동은 4주간 피하십시오.
7. 항응고제나 항혈소판제(아스피린 등)의 사용시점은 의료진과 상의하십시오. 약물 중단 기간이 가급적 7일을 넘지 않는 것이 좋습니다.

Lymphatic involvement가 있어 수술을 보낸 예

Warfarin 사용환자의 ESD 시행 예. EGC (W/D) 12 mm, S/P MAP(ring 31mm), TAP (ring 33mm), Maze op
- severe abdominal pain during the EMR/ESD procedure
- prominent abdominal distension immediately after the procedure
- persistent pain after procedure
- free air on the chest X-ray after gastric EMR/ESD
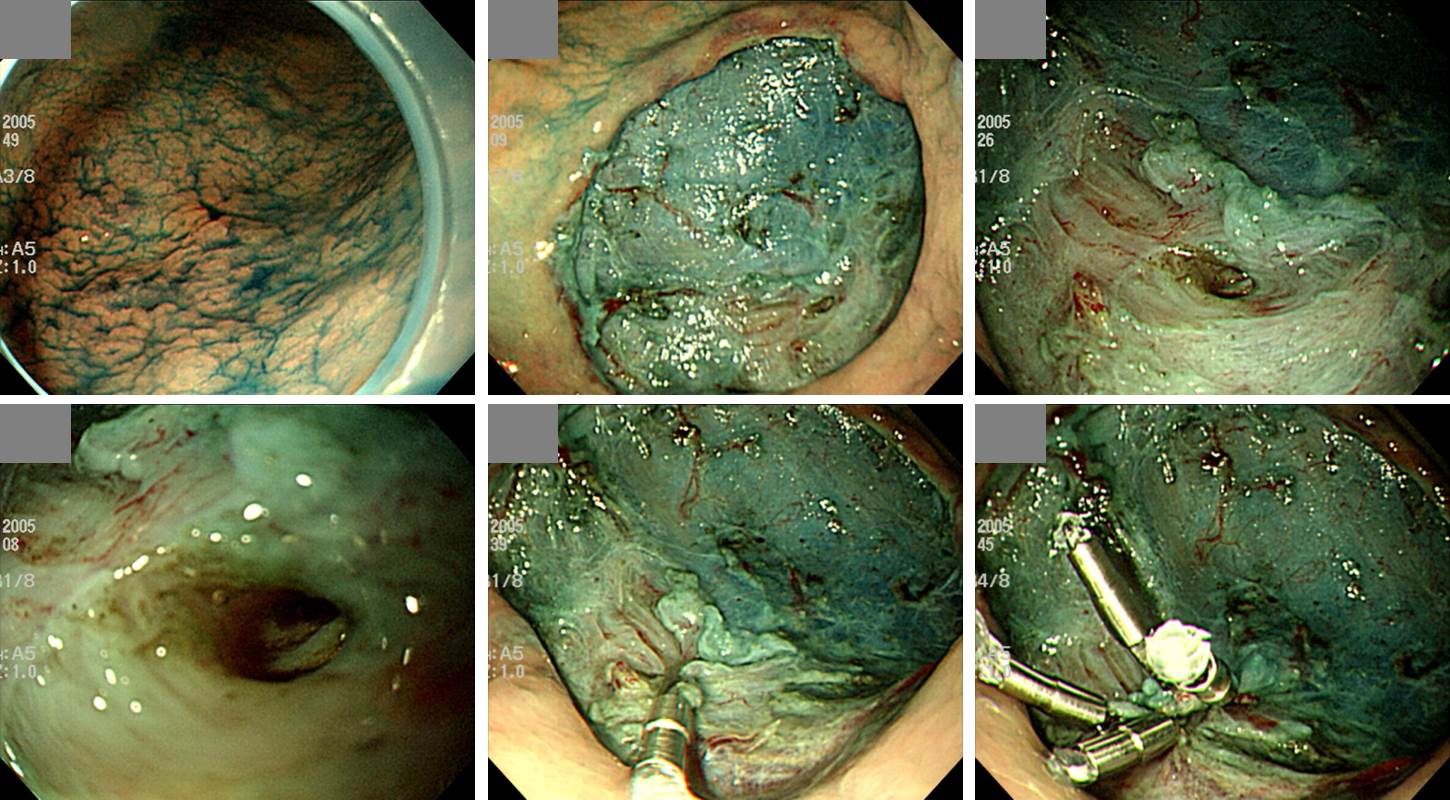
Frank perforation을 즉시 clip으로 치료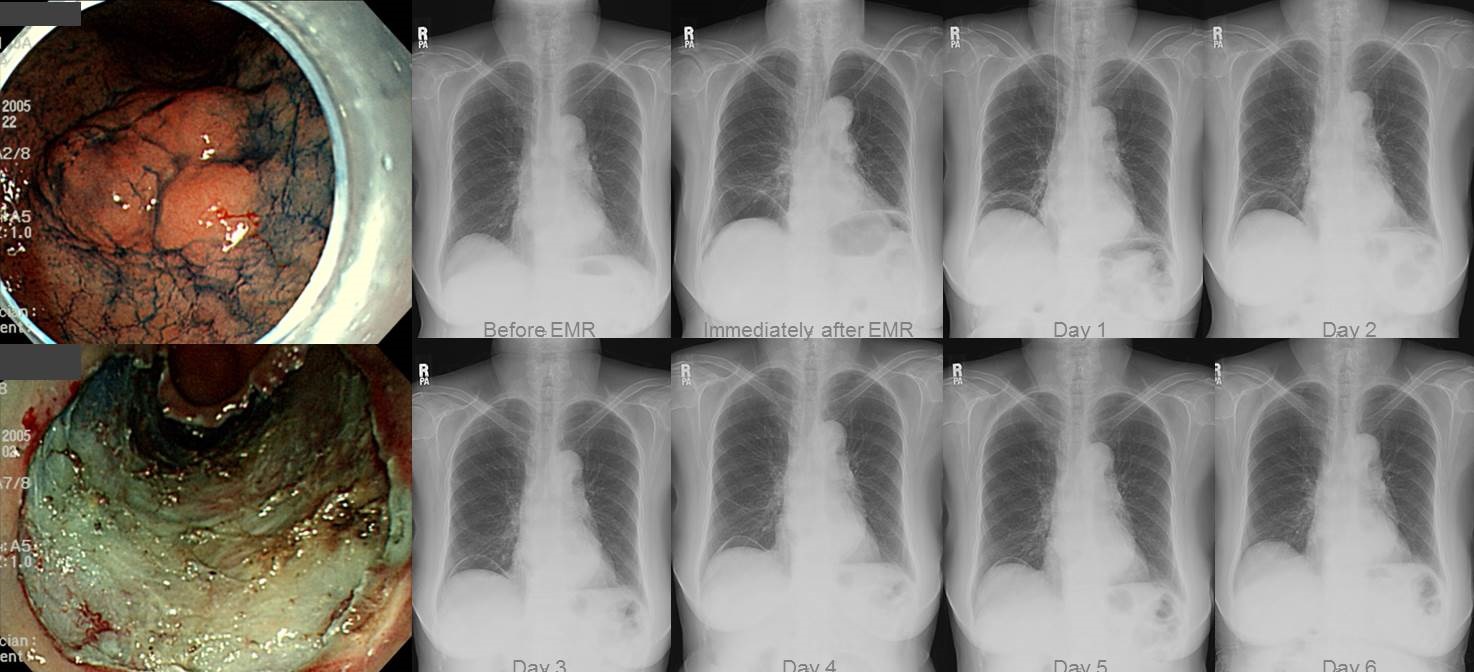
Microperforation. 며칠간의 금식과 항생제 주사만으로 peritoneal free air가 저절로 소실되었다.
- Intravenous antibiotics, usually ceftriaxone + metronidazole. 퇴원시에는 ciprofloxacin을 투여한다. 항생제 투여기간 총 10일이 되도록 조절한다. 감염내과에서는 Unasyn을 권하고 있다 (관련 EndoTODAY).
- Nasogastric tube는 삽입하지 않는다.
- NPO: 통상 EMR/ESD 시술 48-72시간까지 금식하고, 증상의 호전이 있으면 SOW부터 시작한다. 천공이 없었던 통상적인 EMR/ESD에 비하여 1일 늦게 diet가 시작되는 셈이다.
- 통증의 조절: 시술 당일이나 다음 날 통증이 지속되면 IV Demerol 1/2 ampule을 투여한다. 복강내에 free air가 너무 많아서 복부 불편감이 지속되는 환자에서는 복수천자와 비슷한 방법으로 복강내 free air를 제거하기도 한다 (EndoTODAY- 복강공기 제거방법).
- 혈액검사: 시술 다음 날 CBC에서는 약간의 leukocytosis를 보이기도 하지만 1-2일 후 대부분 정상화된다.
- 발열의 조절: 시술 당일 혹은 다음 날까지 경한 발열을 보이기도 하지만 대부분 호전된다.
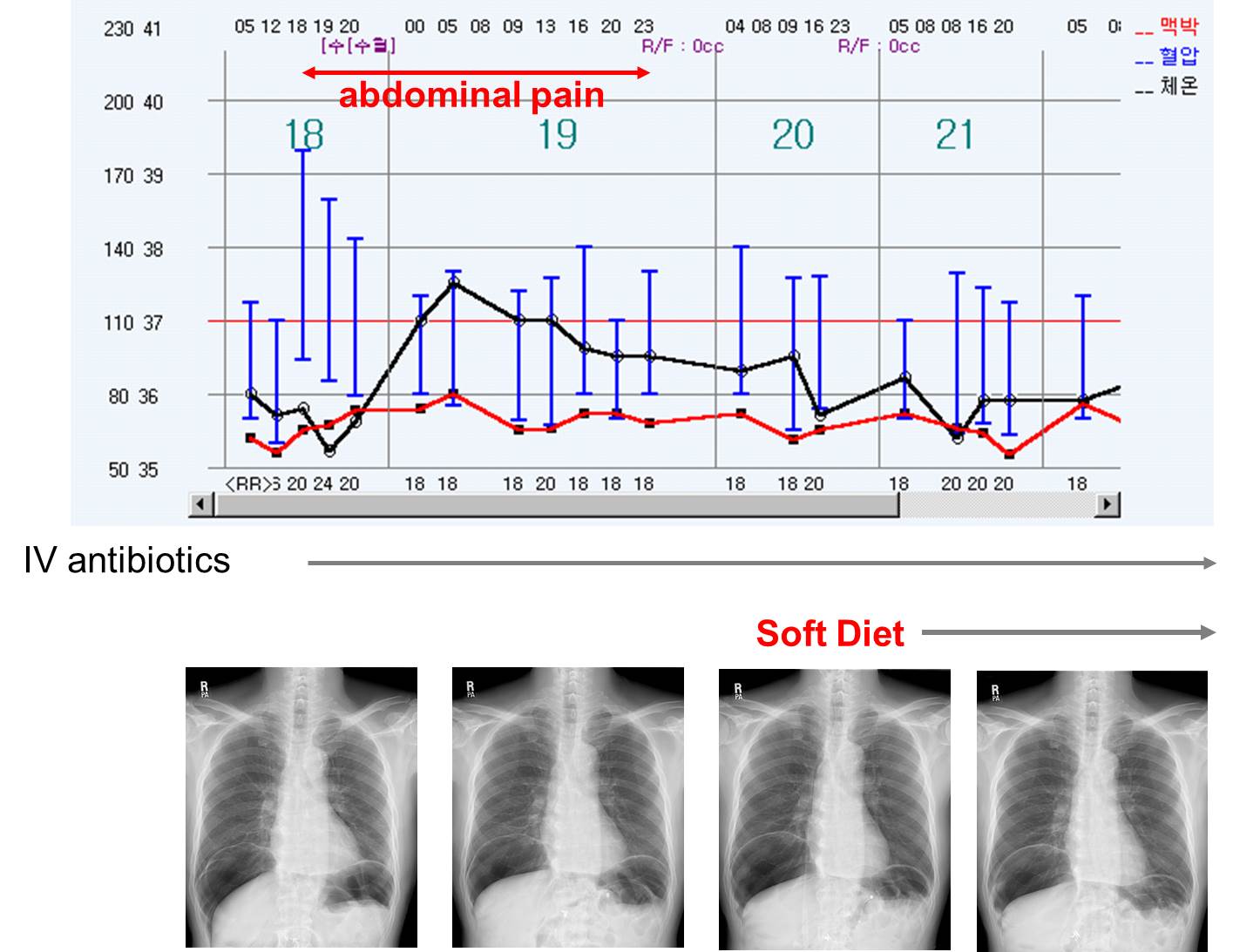
Microperforation 후 전형적인 경과. 약간의 leukocytosis와 발열이 가능하지만 이내 좋아진다. 하루 이상 통증과 발열이 지속되면 수술을 고려해야 한다.
1. 퇴원 직후에는 가급적 부드러운 형태의 음식을 많이 섭취하십시오. (각 종 죽류, 스프류, 부드러운 빵류, 치즈, 연두부, 계란찜류...)
2. 퇴원 2-3일 이후부터 정상적인 식사가 가능하지만 되도록 10번 이상 천천히 꼭꼭 씹어서 섭취하십시오. 몇 주간 장기적으로 죽을 드실 이유는 없습니다.
3. 반드시 피해야 하는 음식은 없으며, 본인의 체중이나 연령에 맞도록 골고루 균형된 식사를 하십시오. 당뇨, 고혈압, 심장, 신장질환 및 간질환과 같은 동반 질환이 있는 분은 관련질환 식이요법을 참고하여야 합니다.
4. 거친 채소나 딱딱한 형태의 음식섭취는 주의하십시오. (더덕, 도라지, 풋고추, 고사리, 멸치, 곳감...)
5. 과도하게 맵거나 짠 음식을 주의하십시오. (젓갈, 짱아찌류, 매운 김치류...)
2) 조기위암 내시경치료에 대한 온라인 환자설명서 (beta version)
3) 입원환자에게 보여드리는 설명 그림
4) Government regulation on ESD - Indications of ESD in Korea (심평원 기준),
5) 보건복지부 고시 2011-129, 130, 132 관련: 내시경적점막하박리절제술(ESD) 고시 개정 관련 질의 응답
6) Complications: perforation, microperforation, bleeding, rare complications
7) Interesting cases: Cancer after ESD for adenoma with LGD, Cancer after ESD for adenoma with HGD, ESD in LT patient
8) Others: Biopsy and aspirin in ESD candidate
9) [Review] Endoscopic resection for EGC beyond absolute indication with emphasis on controversial issues
[Home]