 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Thursday Endoscopy Conference 20170216]
[Thursday Endoscopy Conference 20170216]
 1. EGJ cancer (Barrett's adenocarcinoma)
1. EGJ cancer (Barrett's adenocarcinoma)
Tongue-like projection을 보이는 short segment Barrett esophagus로 추정하고 조직검사를 하였는데 의외의 결과(adenoma with HGD, suspicious carcinomatous transformation)가 나와 의뢰된 분입니다.
ESD가 시행되었고 다행스럽게 병리학적 complete resection 결과였습니다. 민병훈 교수님. 수고 많으셨습니다.
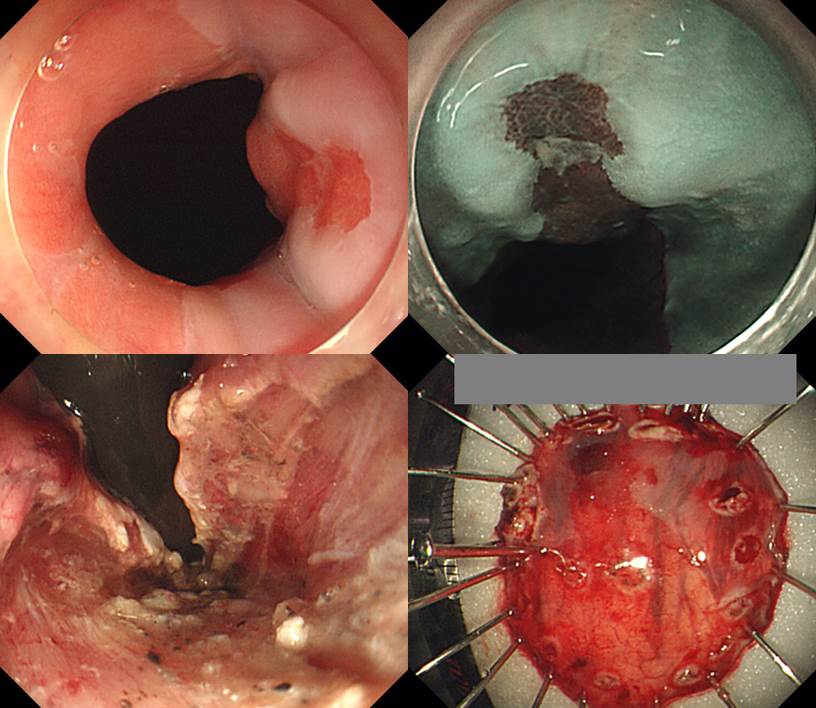
Adenocarcinoma, well differentiated, arising from Barrett esophagus with high grade dysplasia ;
1. Location : gastroesophageal junction
2. Size of carcinoma : (1) longest diameter,9 mm (2) vertical diameter, 6 mm
3. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
4. Resection margin : free from carcinoma(N), safety margin : distal 16 mm, proximal 3 mm, anterior 6 mm, posterior 14 mm
5. Lymphatic invasion : not identified(N)
6. Venous invasion : not identified(N)
7. Perineural invasion : not identified(N)
Stomach, subtotal gastrectomy:
Advanced gastric carcinoma
1. Location : lower third, Center at body and greater curvature
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 3.7x1.4 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma, safety margin: proximal 2.3 cm, distal 9.4 cm
8. Lymph node metastasis : metastasis to 1 out of 37 regional lymph nodes (pN1), (perinodal extension: present) (1/37: "3", 1/11; "4", 0/11; "5", 0/0; "6", 0/0; "7", 0/4; "9", 0/0; "8a", 0/3; "11p", 0/2; "12a", 0/5; "4sb", 0/0; "1", 0/1)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : present
12. AJCC stage by 7th edition: pT2 N1
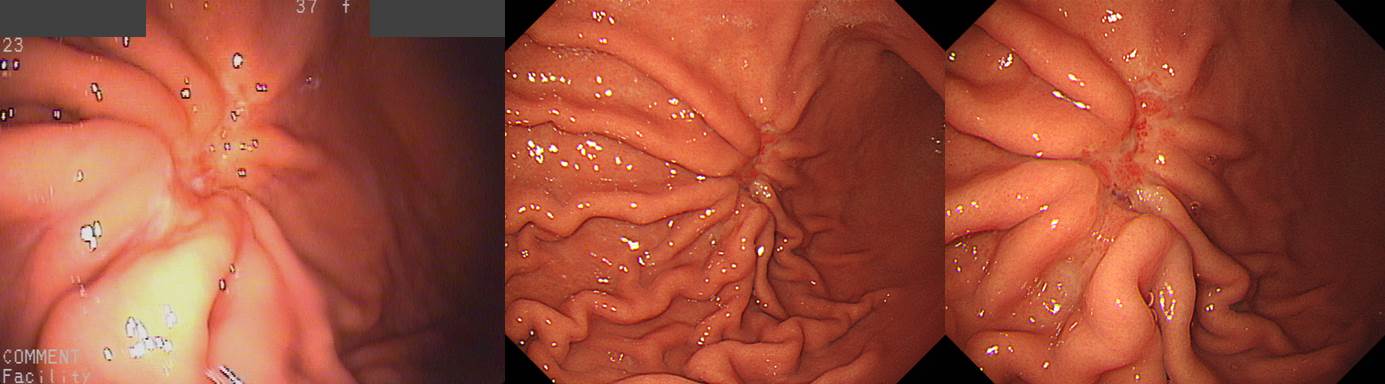
조기위암의 침윤 깊이 (심달도, depth of invasion) 평가의 중요한 요소 중 하나는 fold 변화입니다. Fold는 위내에 공기를 어느 정도 뺐을 때 잘 관찰됩니다. 공기를 약간씩 넣고 빼면서 병소 주변 점막의 변화를 조심스럽게 관찰하는 것이 좋습니다.
조기위암 fold에 대한 (간단하지만 그리 정확하지 않은) 대원칙은 다음과 같습니다. 점막암에서는 abrupt cutting, rapid tapering (= rat-tailing, 쥐 꼬리처럼 생겼다는 의미), 점막하암에서는 fusion, clubbing이, 고유근암(PM cancer)에서는 dam-formation이 관찰됩니다. Fold 변화는 위암 침윤 깊이 예측의 중심이지만 fold에 따른 침윤 깊이 진단이 꼭 옳은 것은 아닙니다. 침윤 깊이 예측은 예술입니다. EGC로 추정했는데 AGC로 나오는 경우는 약 5-10%입니다. AGC로 추정했는데 EGC로 나오는 경우도 약 5-10%입니다. (대한소화기내시경학회지 2007;35:297-303)
이번 증례는 (1) 함몰부가 비교적 깊고, (2) fold fusion 소견이 여럿 관찰되고, (3) 조직형이 signet ring cell carcinoma이었으므로 눈으로 보기보다 다소 깊을 수 있을 여지가 많았던 경우입니다. 비록 내시경에서 EGC III (r/o submucosal cancer)라는 impression을 붙일 수 밖에 없지만... 약간 깊다고 나왔지만 놀랄 필요는 없을 것 같습니다.
* 참고 1: [2013-4-17 대한소화기내시경학회 교육자료] 위암의 내시경 진단 분류 체계
* 참고 2: Survey on endoscopic classification of EGC (EndoTODAY 2013-5-23)
* 참고 3: EndoTODAY 위암 침윤 깊이 진단
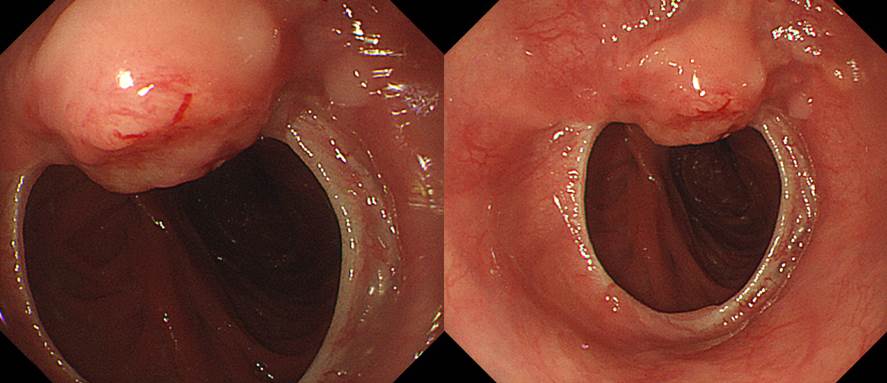
 3. Local recurrence after total gastrectomy for gastric cancer
3. Local recurrence after total gastrectomy for gastric cancer
위암으로 수술하였는데 국소 재발을 보였습니다. 수술 당시부터 병기가 매우 높았고 T colon 결절에서도 metastatic adenocarcinoma까지 나왔던 상황이었습니다.
Stomach, total gastrectomy:
Advanced gastric carcinoma
1. Location : [2] upper third, [1] middle third, Center at body and anterior wall
2. Gross type : Borrmann type 3
3. Histologic type : signet-ring cell carcinoma
4. Histologic type by Lauren : diffuse
5. Size : 8x8 cm
6. Depth of invasion : invades serosa (pT4a)
7. Resection margin: free from carcinoma, safety margin: proximal 1.5 cm, distal 4.5 cm
8. Lymph node metastasis : metastasis to 40 out of 82 regional lymph nodes (pN3b) (perinodal extension: present) (40/82: "1", 0/2; "2", 8/10; "3", 19/25; "4", 7/17; "4sb", 0/0; "5", 1/1; "6", 0/8; "7", 0/2; "8a", 0/1; "9", 1/3; "11p", 1/5; "12a", 0/2; perigastric, 3/6)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : present
12. Associated findings : ulceration
13. Peritoneal cytology : negative
14. AJCC stage by 7th edition: T4a N3b
위암 수술 후 문합부 협착이 발생할 수 있습니다. 특히 total gastrectomy 후 식도와 소장의 연결부가 membraneous하게 좁아지는 경우가 많습니다. 최근에는 많이 줄었지만 2005년에 발표된 삼성서울병원의 자료(Lee SY. EJSO 2005)를 보면 total gastrectomy후 8-9% 전후에서 stricture가 발생하였습니다.
수술한 환자에게 미리 obstruction 증상을 설명해 주는 것은 매우 중요합니다. 간혹 obstruction 증상을 수술 후 당연히 발생할 수 있는 변화로 생각하여 몇 달이나 참고 지내는 환자들을 만날 수 있습니다.
Anastomosis site의 benign postoperative stricture가 흔하지만 드물게 local recurrence도 가능합니다. Benign stricture는 수술 직후부터 수개월 이내에 호발하고 1년 이후에 발생되는 경우는 드뭅니다. 반면 위암의 local recurrence에 의한 stricture는 위암 수술 반년 경부터 2-3년 사이에 발견되는 경향이 있습니다. 일찍 발견되면 benign, 늦게 발견되면 malignancy라는 경향입니다.
문합부 주위의 재발은 문합부 소만측에 많으며, 문합부 주위 점막의 결절상 융기나 점막 비후로 나타날 수 있습니다. 수술 후에는 문합 부위의 부종과 발적, 잔존하는 봉합사 주변으로 염증 및 부분적인 궤양 등은 잔위암 또는 암의 재발과 혼돈될 수 있습니다. 자세히 관찰되고 조금이라도 이상하면 조직검사를 하는 수 밖에 없습니다. 아래는 수년 전 삼성서울병원의 논문(Lee SY. EJSO 2005)에 실렸던 재발예들입니다.
Benign post-op stricture는 수술 후 4-8개월에 발생합니다. 1년 이후에 발견된 협착은 대부분 국소재발입니다. 따라서 total gastrectomy후 anastomosis site stenosis로 내원한 환자에서 가장 먼저 확인할 것은 수술 시점입니다. 수술한지 1년 이상 경과하였으면 대부분 local recur입니다. 게다가 수술 당시 병기가 높았다면 거의 틀림없습니다. 그러나 역은 성립하지 않습니다. 1년 미만이라고 모두 benign post-op stenosis인 것은 아닙니다. 조금이라고 의심스러우면 바로 dilatation을 할 것이 아니고 조직검사를 해야 합니다.
내시경 조직검사에서 adenoma with HGD and suspicious carcinomatous transformation으로 나와 papillectomy를 시도하였으나 non-lifting sign을 보여 PPPD 수술을 하였습니다.
Ampullary Carcinoma arising from IAPN
(1) Histologic type: Adenocarcinoma
(2) Histologic Grade: G2 (moderately differentiated)
(3) Precursor lesion: Adenoma
(4) Invasive tumor size: greatest dimension (0.5cm) (S/N)
(5) T1b Tumor invades into perisphincteric and duodenal submucosa
(6) N0: No regional lymph node metastasis (0/13: LN8, 0/5; LN12, 0/3; periductal, 0/5)
(7) cM0: Clinically No distant metastasis
(8) Involvement of portal vein: absent
(9) Margin status; Bile duct margin : negative; Retroperitoneal margin: negative; Duodenal margin: negative (safety margin: 4cm)
(10) Perineural and neural invasion: absent
(11) Lymphovascular invasion: not identified
* 참고: EndoTODAY 유두부 종양
 6. ESD for esophageal cancer after EVL in LC patient
6. ESD for esophageal cancer after EVL in LC patient
간경변, 식도정맥류 환자에서 정맥류에 연해 식도암이 발견되었고 EVL로 정맥류 치료 후 식도암에 대한 ESD가 성공적으로 시행되었습니다. 민양원 교수님. 수고 많으셨습니다.
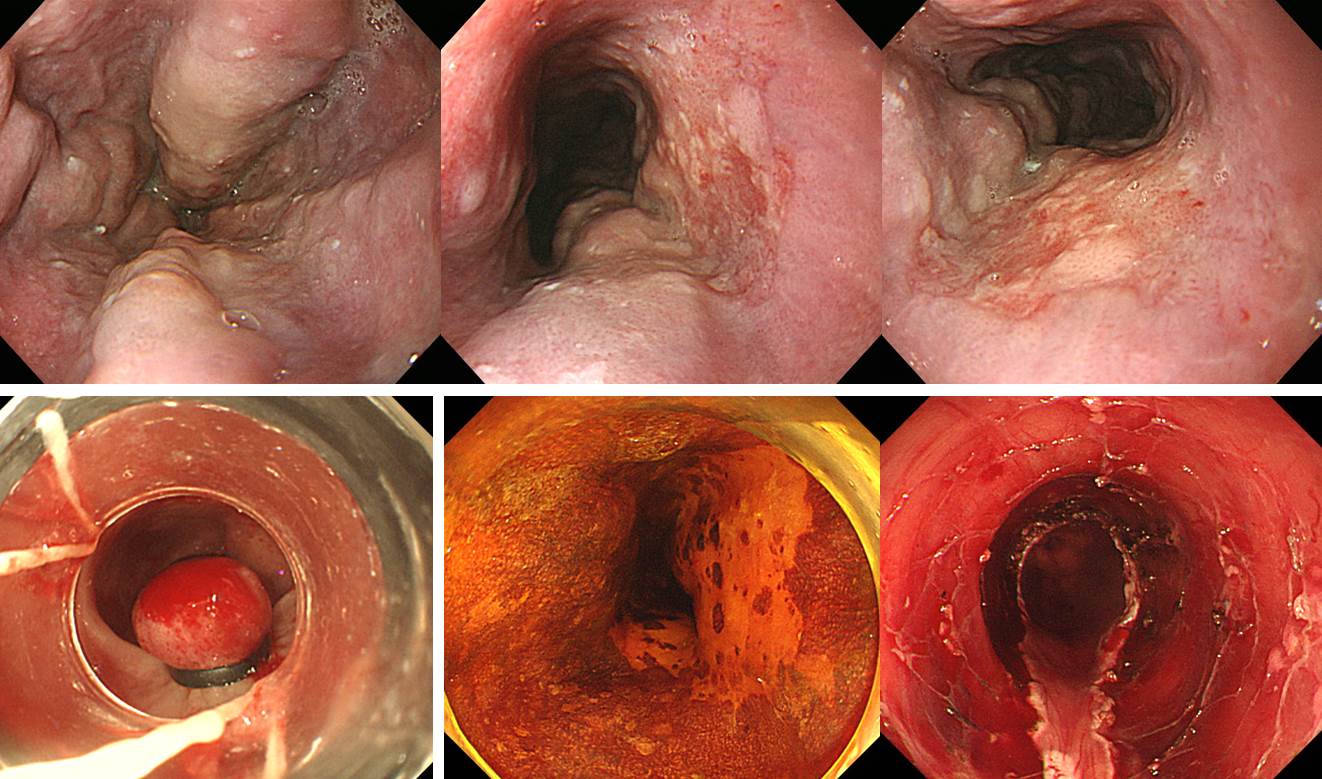
Esophagus, endoscopic submucosal dissection:
Squamous cell carcinoma, moderately differentiated
1. Location : 25cm from incisor
2. Size of carcinoma : (1) longest diameter, 32 mm (2) vertical diameter, 31 mm
3. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
4. Resection margin : free from carcinoma(N), safety margin : distal 3 mm, proximal 2 mm, anterior 6 mm, posterior 4 mm
5. Lymphatic invasion : not identified(N)
6. Venous invasion : not identified(N)
7. Perineural invasion : not identified(N)
8. Peritumoral lymphoid follicle: not identified(N)
1) SMC Endoscopy Unit 삼성서울병원 내시경실
2) SMC Monday GI conference 삼성서울병원 일원내시경교실 월요점심소화기집담회
3) SMC Thursday endoscopy conference 삼성서울병원 일원내시경교실 목요점심내시경집담회
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.