 [Description exercise 2 해설] - 終
[Description exercise 2 해설] - 終
 [Description exercise 2 해설] - 終
[Description exercise 2 해설] - 終
출혈성 위염이라는 말은 가급적 쓰지 맙시다. (완전히 이준행 개인 생각입니다만) RT-induced hemorrhagic gastritis나 immune checkpoint inhibitor-induced hemorrhagic gastritis와 같이 특수한 경우를 빼고 출혈성 위염이라는 말을 쓰지 않도록 권합니다.
적절한 내시경 검사 시간은 몇 분일까요? 저는 위내시경은 전체 검사시간 5분, 대장내시경은 withdrawal time 6분이라고 생각합니다. 내시경을 처음 시작하는 1년차 fellow의 경우 오전 위내시경 12명이 적당합니다. 검사 시간은 5분이지만 sedation, 환자파악, 처방, 결과입력 등의 시간도 필요하기 때문입니다. 1년차 중반 혹은 2년차 이상이 되면 좀 더 많은 검사를 할 수 있습니다. 검사를 잘 해 드려야겠다는 생각으로 한 명의 환자에서 너무 긴 시간을 쓰는 것은 환자에게도 해가 될 수 있습니다. 특히 비진정 내시경의 경우는 더욱 그러합니다. 뭐든지 적절한 것이 좋습니다. 너무 빠르지도 않고 너무 느리지도 않게. 中庸.
DEX 2에 대한 여러 질문이 있어서 답변 동영상을 만들어 보았습니다.
소견: Squamocolumnar junction이 diaphragmatic orfice보다 2cm 이상 올라와 있음. 하부 식도에 4개 정도의 linear하고 아래쪽으로 갈수록 넓어지는 exudate로 덮힌 mucosal break가 있으며 맨 하단에서 circumference의 75% 이상 fusion되어 있음.
진단: (1) Sliding hiatal hernia, (2) Reflux esophagitis, LA-D
[이준행 comment]
진단명을 GERD로 주신 분이 많았습니다. GERD는 임상 진단명입니다. GERD는 내시경에서 mucosal break(대강 erosion이나 ulcer를 말하는 것임)가 뚜렷한 reflux esophagitis (관례적으로 reflux esophagitis = erosive esophagitis)와 mucosal break가 없는 non-erosive reflux disease (NERD)를 포함하는 개념입니다 (GERD = reflux esophagitis + NERD). 따라서 전형적인 산역류 증상이 있는 환자에서 내시경 진단은 mucosal break가 있으면 reflux esophagitis LA-A/B/C/D로, mucosal break가 없으면 정상으로 내면 되겠습니다. Hiatal hernia가 있으면 병기해 주십시오. 내시경 진단명으로 GERD를 쓰지 마시기 바랍니다.
진단명으로 "LES incompetence"이라 쓰신 분도 계셨습니다. 내시경 진단은 anatomical diagnosis입니다. 무리하여 functional diagnosis를 붙이면 적지 않은 혼선이 발생합니다. LES incompetence 대신 hiatal hernia가 적절한 진단명입니다.
위식도역류질환의 진단 및 치료에 대한 아래 동영상을 꼭 보시기 바랍니다.
역류성 식도염에 의한 mucosal break가 보통의 경우처럼 가늘지 않고 넓은 모양이었으므로 간혹 바렛식도로 답한 분이 계셨습니다. 그러나 바렛식도는 염증 소견보다는 metaplasia입니다. 그냥 예쁜 columnar colored mucosa로 보이므로 영 다릅니다. 아래를 참고하세요.
이 정도 심한 역류성식도염에는 늘 hiatal hernia가 동반되기 마련입니다. Hiatal hernia는 내시경 초심자들이 올바른 개념을 잡기가 어려운 부분이기도 합니다. 아래 동영상을 꼭 보시기 바랍니다.
Hiatal hernia의 분류를 mixed paraesophageal 형으로 답한 분이 계셨습니다. 위에서 retroflexion한 사진이 없어서 정확히 알 수 없지만 저는 sliding hernia로 보았는데요... 사실 mixed paraesophageal hernia일 가능성도 없지 않습니다.
주변 점막을 언급하신 분이 계셔서 답변을 드렸습니다. 다소 모호하게 답했습니다.
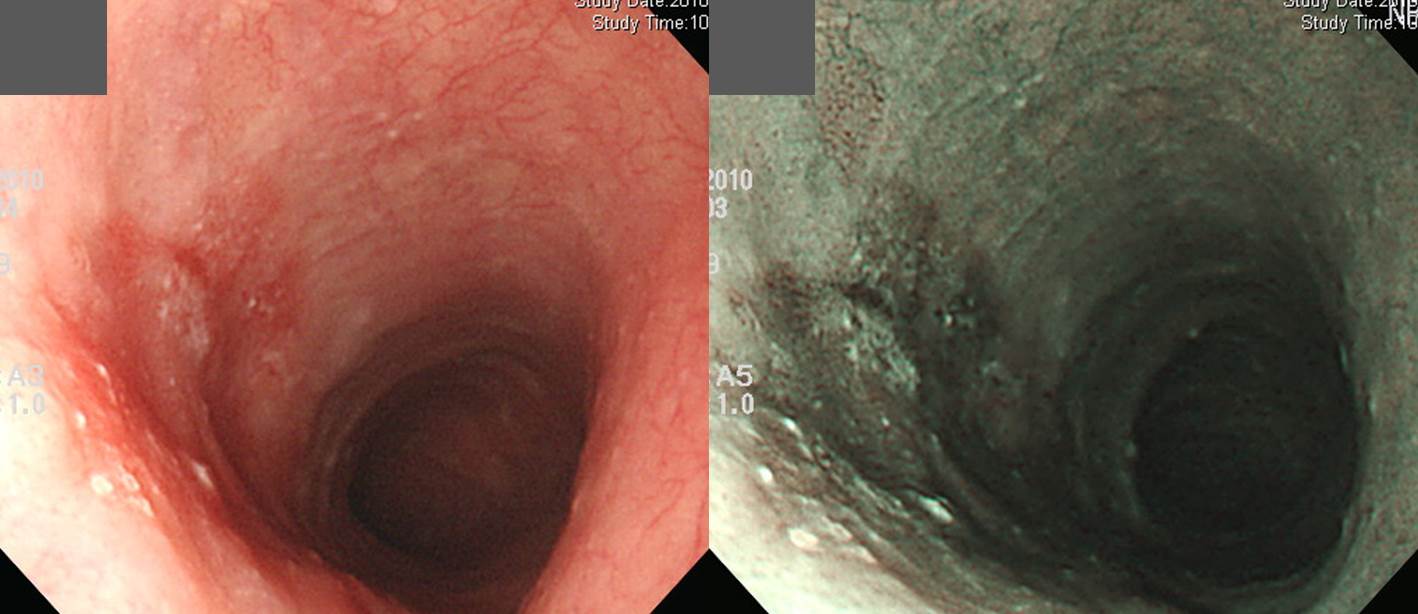 left: white light endoscopy picture, right: NBI (narrow band imaging) picture
left: white light endoscopy picture, right: NBI (narrow band imaging) picture
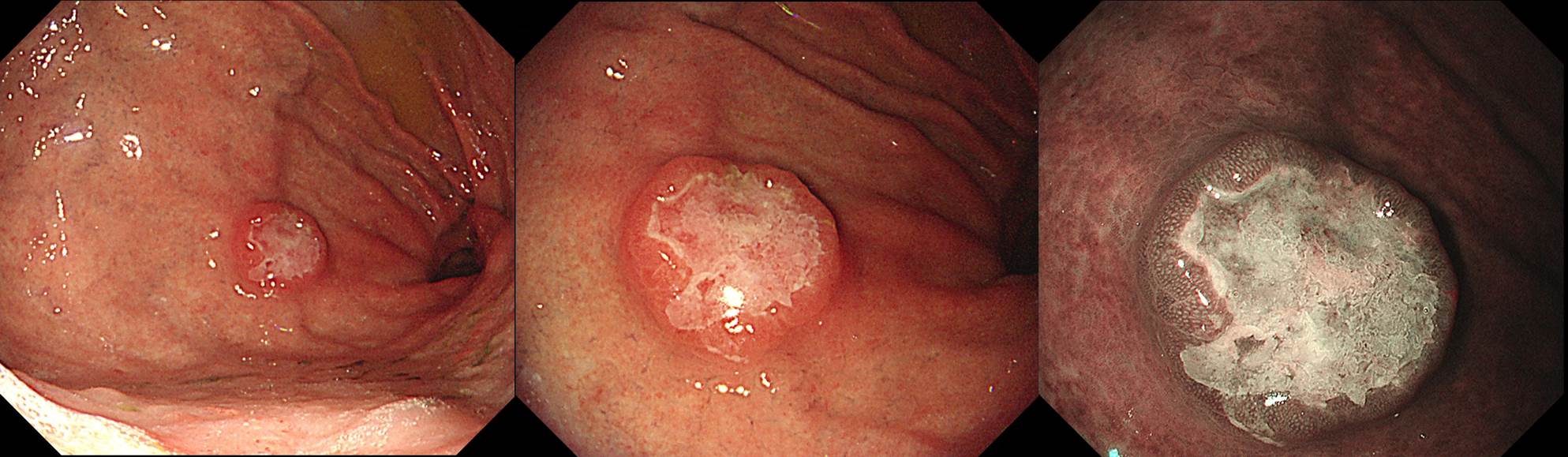
소견: 중부식도 6시~9시 방향에 2 cm 가량의 slightly depressed hyperemic area가 있음. 9시 방향으로 0.5cm 정도의 경미한 융기부도 보임. 경계는 약간 불규칙하지만 전체적으로 둥근 병소이고, 표면은 일부 irregular한 양상이며 일부 white papule 양상의 exudate가 붙어 있음.
진단: Superficial esophageal cancer, IIb - 참고: IIc라고 해도 무난할 것 같습니다.
[이준행 comment]
식도의 지름은 대강 2.5 cm 입니다. 이를 고려하여 크기를 짐작해 주십시오. 저는 flat 혹은 depressed로 생각하였는데 의외로 여러분이 slightly elevated로 보셨군요.^^ 관례에 따라 식도에서는 내시경 진단에 early esophageal cancer라고 쓰지 말고 superficial esophageal cancer라고 쓰시기 바랍니다. '경계가 모호하다'고 표현할 정도로 모호하지 않은데요... 이 정도는 비교적 경계가 잘 보이는 편입니다. 크기 언급이 없는 분이 많았습니다. 종양성 질환에서는 항상 크기를 언급해 주는 것이 좋습니다. 식도에서는 크기 대신 circumference의 얼마를 차지한다고 쓰는 것도 가능합니다. 이 경우는 '지름 2 cm 크기의 혹은 circumference의 40%를 차지하는' 정도의 표현을 소견에 써 주었으면 좋았을 것 같습니다.
Early esophageal cancer라 답한 분이 많으셨는데요, 식도에서는 superficial이라는 표현이 좋습니다. 수술 후 림프절 전이가 없다는 것이 확인된 후 early esophageal cancer라고 붙입시다. 식도와 위의 early cancer 개념이 다른 것이 문제입니다. 통일하면 좋을 것이지만, 식도 전문가들이 고집을 부려서 서로 다른 정의를 사용하고 있으니 골치가 아픕니다. 그러나 따르는 수 밖에...
표재성 식도암 내시경 소견은 아래과 같습니다. 조기위암처럼 fold가 끌려온다거나 edge가 어떻다거나 margin이 어떻다는 등의 소견이 없습니다. 모호한 색조변화, 정상 식도의 submucosal vessel들이 잘 보이지 않는다 등이 오히려 중요한 소견입니다.
표재성 식도암 내시경 소견 1) Faint hyperemia
2) Change of microvasculature
3) Eroded/ulcerated
4) Mucosal thickening
5) Coarsening of the mucosa
6) Multiple white mucosal plaques수술을 하였고 아래와 같은 소견이었습니다. 내시경 치료를 할까 잠시 고민하다가 수술보낸 환자인데 림프절 전이까지 있었습니다. 휴~~~
Invasive squamous cell carcinoma, moderately differentiated:
1) tumor size: 2.5x1.5 cm
2) extension to submucosa
3) endolymphatic tumor emboli: not identified
4) perineural invasion: not identified
5) negative resection margins (proximal, 3 cm ; distal, 15 cm)
6) metastasis to one out of 22 regional lymph nodes
* 참고: EndoTODAY 표재성 식도암
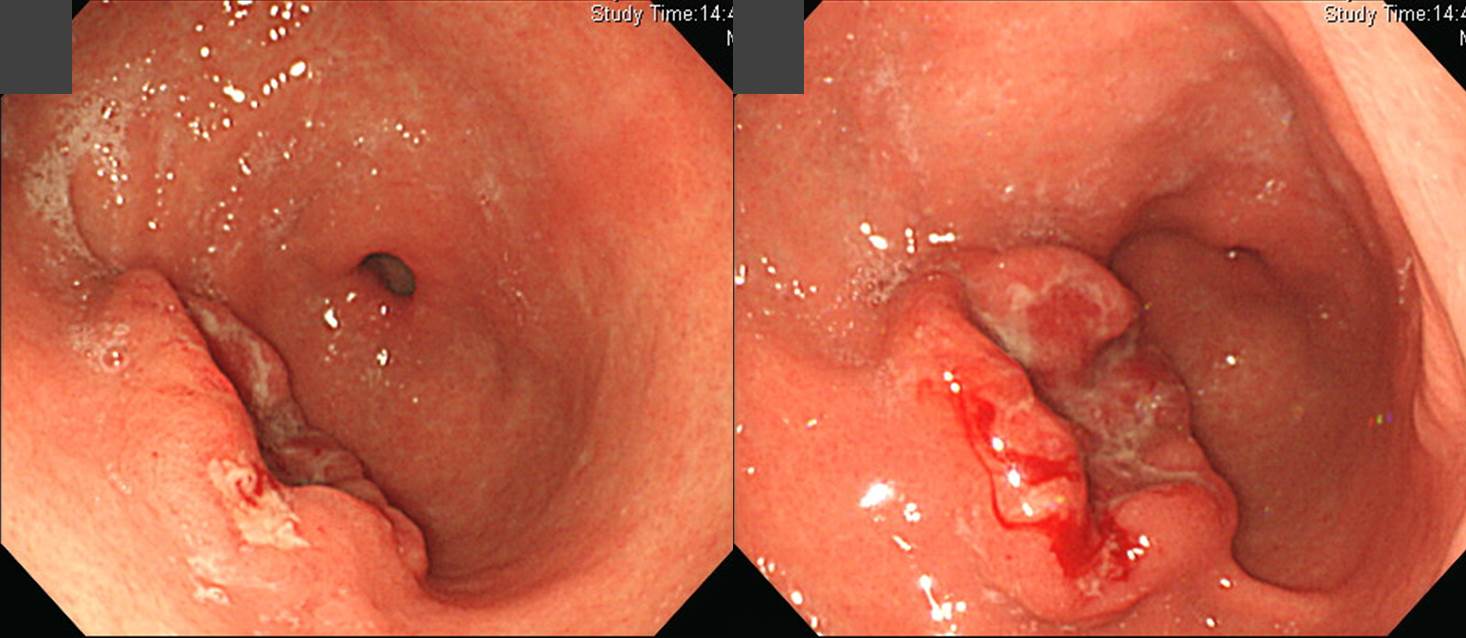
소견: 전정부 전반에 걸쳐 지저분해보이는 다양한 크기의 ulcer, erosion들이 산재되어 있고 hematin이 부착되어 있음.
진단: AGML (acute gastric mucosal lesion)
[이준행 comment]
위장관에 어떤 병이 생길 수 있는지 알아야 맞출 수 있는 문제입니다. 암, 궤양 말고도 병은 많습니다. 특징적인 소견이고 AGML이라고 합니다. 내시경 초심자는 아틀라스 한권을 처음부터 끝까지 빠르게 다 읽어볼 필요가 있습니다. '소화기내시경아틀라스-상부위장관: 전공의와 개원의를 위한' 을 추천합니다. 오래 전 제가 주저자로 참여하여 쓴 책입니다. 그 책의 위암은 모두 제 증례입니다.
이런 문제가 더 어려울 수 있습니다. 내시경만 보면 그렇습니다. 증상과 맞춰보아야 합니다. 문제를 다시 보면 acute abdominal pain이라고 되어 있을 것입니다. 급성이라는 말입니다. 급성 복통으로 내원한 경우이므로 malignancy의 가능성은 매우 낮아집니다. 여기까지 생각한 후 내시경을 보면 AMGL을 떠올릴 수 있을 것입니다.
AGML 맞습니다. 다만 'hemorrhage가 있었던 것으로 보임'은 사족입니다. 내시경에서는 보이는 것만 쓰면 됩니다. hemorrhage 여부는 임상가가 판단하면 될 문제입니다. 내시경 의사는 깔끔하게 보이는 것만 씁시다. 'Hemorrhage가 있었던 것으로 보임'을 꼭 쓰고 싶다면 소견이나 impression에 쓰지 말고 그 아래에 comment (혹은 note)라는 항목을 만들어 해당 내용을 언급해 줍시다.
* 참고: EndoTODAY AGML
소견: 근위전정부와 위체하부에 2-3cm 크기의 다양한 크기의 ulcer가 있고 일부 hematin이 부착되어 있음. Ulcer margin이 edematous 하고 erythema가 동반되어 있음.
진단: Multiple benign gastric ulcers, A2 (r/o CMV gastritis, r/o NSAID induced gastritis)
[이준행 comment]
Multiple ulcers 이므로 NSAIDs-associated를 고려하는 것이 가장 타당합니다. R/O Zollinger-Ellison syndrome을 언급하신 분도 계셨는데요... 글쎄요... 가능성은 떨어지는 것 같습니다.
AGML로 답한 분이 계셨습니다. 그러나 AGML은 보다 acute하고 보다 광범위한 경우에 붙이면 좋겠고 이 경우는 다발성 궤양이 적당할 것 같습니다.
이 증례는 NSAID 복용자의 다발성 궤양이었습니다.
* 참고: EndoTODAY NSAID 위장관 합병증
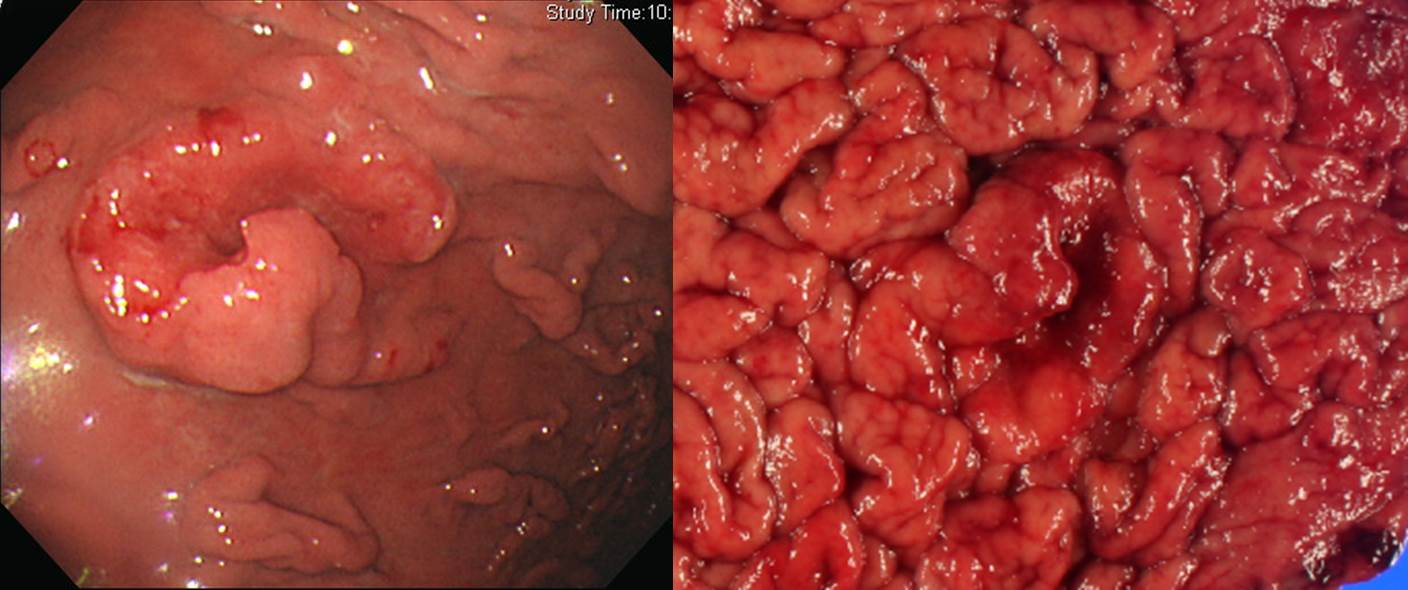
소견: Proximal antrum, lesser curvature 에 2 cm 정도의 전체적으로 flat한 elevated lesion이 있습니다. 표면은 nodular하고 정상 점막과의 경계는 white light endoscopy에서는 다소 불명확하지만 indigo carmine 살포 후에는 비교적 명확하게 관찰됩니다.
진단: Early gastric cancer, IIa
[이준행 comment]
전정부 위치를 세분하는 방법을 문의하신 분이 계셨습니다. 좋은 질문이라고 생각되었고 답변 내용을 소개합니다.
조기위암이나 진행위암의 subtype 분류는 대강 하는 것이 좋습니다 (EndoTODAY 조기위암 내시경 분류). 대강 납작하되 약간 올라왔으면 type IIa, 상당히 튀어 올라왔으면 type I으로 주시기 바랍니다. 자로 측정하여 몇 mm 이상이면 어떻고... 등은 쓰잘데기 없는 일입니다. 조기위암을 별로 본 적이 없는 서양사람들을 가르치려고 억지로 만든 Paris 분류는 약간 무시해도 좋습니다.
Mass로 표시한 분이 계시는데... 이보다는 nodular elevated lesion으로 표현해주시기 바랍니다. 즉 superficial lesion이라는 뜻이지요. 납작한 병소. Mass는 보통 AGC에서 쓰는 용어입니다.
초심자 중에는 함몰형 위암으로 보신 분도 계셨습니다만, 이 병소는 주로 flat nodular elevated lesion입니다. Elevated nodule 사이 사이가 약간 함몰된 것 뿐이지 함몰형 위암은 아닙니다.
크기 측정에 대한 질문이 있었습니다. Antrum을 가득 채우는 지름 6cm 공이 있다고 생각해 보세요.
전체를 하나로 보는 방향으로 describe 해 봅시다.
ESD를 했습니다. 최종 병리 결과는 아래와 같았습니다.
Stomach, endoscopic submucosal dissection:
. Early gastric carcinoma
1. Location : antrum, lesser curvature
2. Gross type : EGC type IIa+IIb
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size : 2.8x2.3 cm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin: free from carcinoma (safety margin: distal 0.8 cm, proximal 0.8 cm, anterior 0.4 cm, posterior 0.8 cm)
8. Lymphatic invasion : not identified
9. Venous invasion : not identified
10. Perineural invasion : not identified
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
2017년 소화기학회 연수강좌에서 위암의 진단과 치료에 대하여 강의한 아래 동영상을 참고해 주시기 바랍니다.
소견: 위전정부 소만에 4 cm 크기의 mass가 있음. Mass의 상단부는 함몰되어 있는데 distal 부위는 주변에 비하여 일부 함몰되어 있음.
진단: AGC, type I
[이준행 comment]
EGC인지 AGC인지 애매합니다. 다소 깊은 EGC일 수도 있고, PM cancer 정도의 AGC일 수도 있는 그런 상황인데요.... 수술 후 병리결과에서는 deep SM invasion (SM3)을 보인 EGC였지만, 내시경 진단으로 AGC를 붙였다고 크게 탓할 정도는 아닙니다. EGC type I과 AGC type I은 늘 구분하기가 어렵기 때문입니다 (EndoTODAY 보만 1형 진행성 위암과 1형 조기위암의 구분).
AGC로 보았을 때 보만 타입이 다소 애매합니다. 저는 보만 1형을 추천합니다. 일부가 다소 함몰되어 있지만 보만 2형에서 보이는 뚜렷하고 깊은 궤양은 아니니까요.
7-8시 방향의 abnormal fold에 대한 질문이 있어 답합니다. 일반적으로 fold는 궤양형 병소에서 발생하지만 융기형 병소에서도 점막이 들리면서 주름이 잡히는 경우가 있습니다. SMT에서는 이런 것이 자주 보이는데 bridging fold라고 합니다. 이와 비슷하다고 이해하시기 바랍니다. 다른 특별한 comment는 없습니다. 이준행
AGC로 생각하고 수술했는데 deep SM invasion을 보이는 EGC였습니다.
Stomach, subtotal gastrectomy:
Early gastric carcinoma
1. Location : lower third, Center at antrum and lesser curvature
2. Gross type : EGC type I
3. Histologic type : gastric carcinoma with lymphoid stroma (medullary carcinoma)
4. Histologic type by Lauren : intestinal
5. Size : 3x2.3 cm
6. Depth of invasion : invades submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 17 cm, distal 4.5 cm
8. Lymph node metastasis : no metastasis in 41 regional lymph nodes (pN0), (perinodal extension: absent)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: T1b N0
2017년 새로 fellow 과정에 들어온 선생님께서 과거 본인이 경험한 유사 증례를 보내주셨습니다. 병리 type이 동일한 것이었습니다. 감사합니다.
Stomach, total gastrectomy ;
EARLY GASTRIC CARCINOMA
Location : upper third
Gross type : EGC type IIa
Histologic type: MODERATELY DIFFERENTIATED ADENOCARCINOMA WITH LYMPHOID STROMA (=lymphoepithelioma-like carcinoma)
Histologic type by Lauren: Intestinal type
Size: 1.7 x 1.2 cm
Depth of invasion: invades submucosa (sm3) (pT1b)
Resection margin: free from carcinoma
NO PERIGASTRIC LYMPH NODE available for histologic examination
Lymphatic invasion: not identified
Venous invasion: not identified
Perineural invasion: not identified
Pathologic stage: pT1b pNX
내친 김에 lymphoepithelioma-like carcinoma (림프양상피종양 암종)를 조금 더 설명해 보겠습니다. Lymphoepithelioma-like carcinoma (LELC)는 비인두암과 조직학적으로 유사하고, 림프구성 간질을 가진 미분화된 위종양입니다. Epstein-Barr 바이러스와의 연관성도 언급되고 있습니다. LELC은 식도, 위, 담관, 타액 선, 폐, 자궁, 피부 등에서 발생합니다. 위 LELC는 전체 위암의 l-4%를 차지하는데 조기위암의 경우 IIa + IIc형이 많으며 진행성 위암의 경우 Borrmann type IV 형이 많다고 합니다. 조기위암의 형태로 나타날 경우는 일반적인 조기위암과 예후가 비슷하나 진행성 위암의 형태를 취할 경우 일반적인 진행성 위암에 비하여 예후가 훨씬 좋은 것으로 알려져 있습니다. 드물게 점막하 종양의 형태로 나타나는 경우도 있어 주의가 필요합니다. (참고: 대한소화기내시경학회지 2004;28:123-126)
관련 저널 하나 소개합니다.
Wang HH, Wu MS, Shun CT, Wang HP, Lin CC, Lin JT. Lymphoepithelioma-like carcinoma of the stomach: a subset of gastric carcinoma with distinct clinicopathological features and high prevalence of Epstein-Barr virus infection. Hepatogastroenterology. 1999;46(26):1214-9.
METHODOLOGY: Of 379 patients with gastric adenocarcinoma, from 1993 to 1996, 6 of them with lymphoepithelioma-like carcinoma of stomach were retrospectively studied.
RESULTS: Five patients were females and one patient was male. Their age ranged from 51-75 years with a mean age of 61.5 years. Endoscopically, 2 patients were initially diagnosed as early gastric cancer and the other 4 were diagnosed as advanced gastric cancer. Three patients had tumors located in the lower third of the stomach, while the other three tumors were located in the middle and upper third. Two tumors invaded into the serosal layer and the other four lesions were confined at submucosal and muscular layers. Using the in situ hybridization method, all 6 patients (100%) had positive nuclear Epstein-Barr virus-encoded small RNA signals in the tumor cells but not in the surrounding lymphoid stroma and non-neoplastic gastric mucosa. Helicobacter pylori was found in 4 (66.7%) of the cases. The mean follow-up period of the 6 patients was 27 months. Five patients were free of the disease. Lymph node involvement and mesenteric implantation was noted in one patient in which cancer recurred 1 year after gastrectomy.
CONCLUSIONS: Lymphoepithelioma-like carcinoma of stomach in this study revealed a female predominance, preferential localization in the proximal part of the stomach, better prognosis, and a high association with Epstein-Barr virus infection.
관련 증례 몇 개 소개합니다.
Early gastric carcinoma
1. Location : lower third, center at antrum and greater curvature
2. Gross type : EGC type IIc+IIa
3. Histologic type : lymphoepithelioma-like carcinoma (EBV-positive)
4. Histologic type by Lauren : intestinal
5. Size : 2.5x2x0.5 cm
6. Depth of invasion : extension to submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal, 10.0 cm; distal, 1.8 cm
8. Lymph node metastasis : metastasis to 2 out of 36 regional lymph nodes (pN1)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
Advanced gastric carcinoma
1. Location : upper third, Center at high body and greater curvature
2. Gross type : Borrmann type 2
3. Histologic type : lymphoepithelioma-like carcinoma
4. Histologic type by Lauren : diffuse
5. Size : 4.4x3.2x1.4 cm
6. Depth of invasion : extension to proper muscle (pT2a)
7. Resection margin: free from carcinoma, safety margin: proximal, 5.5 cm; distal, 21 cm
8. Lymph node metastasis : no metastasis in 67 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10.Venous invasion : not identified
11.Perineural invasion : not identified

1. Location : upper third, center at cardia (Siewert III)
2. Gross type : Borrmann type 2
3. Histologic type : Medullary carcinoma (lymphoepithelioma-like carcinoma)
4. Histologic type by Lauren : indeterminate
5. Size : 2.2x2.2 cm
6. Depth of invasion : invades muscularis propria
7. Resection margin: free from carcinoma, safety margin: proximal 1.4 cm, distal 2 cm
8. Lymph node metastasis : no metastasis in 52 regional lymph nodes
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
Findings: 십이지장 구부의 전벽쪽으로 fold들이 converging하는 모양이고 ulcer crater는 없음. 이로 인하여 십이지장 구부가 약간 deformed 되어 있음. (Duodenal bulb was deformed due to multiple converging folds. There was no active ulcer crater.)
Impression: Duodenal ulcer scar, S2
[이준행 comment]
십이지장이 매우 어려웠던 모양입니다. 작은 erosion 혹은 ulcerative lesion이라도 답한 분도 계시는데요... 사실 그러한 종류는 아무 것도 없습니다. 단지 ulcer scar와 주변으로 끌려오는 여러 fold 들만 있을 뿐입니다.
보이지 않는 ulcer crater를 보인다고 하고, 보이는 fold를 보이지 않는다고 답한 분들이 많습니다. 선입견이 이리 무섭습니다. 아래와 같이 해석하기 바랍니다.
H2 stage로 답해주신 분이 계셔서 아래와 같이 그림을 그려 설명하였습니다.
아래는 melena 며칠 후 내원하셨던 분입니다. 출혈은 없었고 ulcer crater와 red pigmentation 정도만 보였습니다. 추적내시경에서 완전히 호전되었습니다. 만약 어떤 환자에서 좌측 사진과 같은 소견이 보이면 궤양의 과거력을 물어보여야 하겠지요?
 [EndoTODAY Weekly Seminar 다시보기 (2020년)]
[EndoTODAY Weekly Seminar 다시보기 (2020년)]
2020-25. 중환자실 내시경과 스트레스 궤양 예약
2020-24. 보만 4형 진행성위암. AGC Borrmann type 4
2020-23. Achalasia, lymphoma, EG junction cancer, Trichuris trichiura, EGC arising from hyperplastic polyp
2020-22. Esophageal diverticulum, anal melanoma, Henoch Scholein purpura, colonic invasive aspergillosis, esophageal neuroendocrine carcinoma
2020-21. Hiatal hernia Achalasia EGC Cowden NET (대한위대장내시경학회 on-line 강의) - 학회 1달 후인 7월 7일부터 YouTube에서 시청하실 수 있습니다.
2020-20. Cowden syndrome 카우덴 증후군
2020-19. Inlet patch, lymphangioma, cavernous hemanioma, rectal carcinoid
2020-18. FAP. Familial adenomatous polyposis. 가족성 선종성 용종증
2020-17. Hereditary non-polyposis colorectal cancer (HNPCC) = Lynch syndrome, 유전성 대장암
2020-16. 바렛 식도암, 위신경내분비종양, 허혈성 장염, 대장 전이
2020-15. 미란인가, 궤양인가, 혹시 암은 아닌가?
[Special] 헬리코박터에 대한 사견 (2020)
2020-14. 위암, 위용종증 (Cowden syndrome), 내시경 사진과 내시경 시스템의 button 익히기
2020-13. 식도암, amyloidosis, extrinsic compression
[Special] 순천만 내시경 세미나 특강: 위장관 게실증
2020-12. Introduction to IEE (image enhanced endoscopy)
2020-11. One point lesson - 응급내시경과 금식기간, actinomycosis, CMV 식도염
2020-10. 식도질환 내시경 사진 토론. Mucosal break, hiatal hernia, achalasia, esophageal ESD
2020-9. Quiz 해설 (성결) - 상부식도암, 위암과 위궤양, 항문 흑색종, 직장 MALToma
2020-8. 위축성 위염, 와파린, 난치성 궤양, 변비
2020-7. Quiz 해설 (오주현)
2020-6. Quiz 해설 (김민지)
2020-5. 식도 질환 FAQ. 무증상 식도 칸디다증, Sloughing esophagitis, 식도 black pigmentation, 식도 dysplasia, Achalasia, Diffuse idiopathic skeletal hyperostosis
2020-4. 내시경 검사 전 아스피린 중단, 헬리코박터 조직검사, MALToma 추적검사 등 fellow 선생님들의 질문에 답합니다.
2020-3.
2020-2.
2020-1.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.