 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Barrett's esophagus. 바렛식도] - 終
[Barrett's esophagus. 바렛식도] - 終
[바쁘신 분을 위한 한 줄 요약]
우리나라에서 바렛식도의 임상적 의의는 거의 없거나 minimal입니다. 바렛 식도의 내시경 진단에서 가장 중요한 point는 바렛이 아닌데 바렛으로 과잉진단하지 말자는 것입니다. 괜히 환자 걱정시키지 맙시다.
M/53 (2018) 바렛식도로 듣고 놀라서 찾아오셨으나 바렛식도가 아니었던 경우. Z-line은 다소 불규칙할 수 있습니다. 그게 정상입니다. 그래서 Z-line입니다.
[2025-9-16. SMC 화요아침내시경세미나]
바렛식도에 대한 토론을 하였습니다. 진단에 대한 혼선과 치료에 환상이 많은 condition입니다. 과잉 진단/치료를 피하고 과소 진단/치료도 피하고 적정 진단/치료를 해야 할 것인데 참 어렵습니다.
1. 바렛식도 요약
2. 내시경 소견과 조직검사 - CLE (columnar-lined esophagus)
3. 내시경 증례 - 이형성 dysplasia 증례
4. Reflux esophagitis with Barrett esophagus
5. 역학
6. 이형성이 없는 바렛식도 - 내시경 소견과 임상적 의의
7. 암발생 위험
10. 2016 ACG 가이드라인
11. Symposiums
12. EndoTODAY FAQ on Barrett esophagus
13. References
바렛식도의 전통적인 정의는 식도 하부의 편평상피가 원주상피로 치환된 것을 의미하지만, 최근에는 특수 장상피화생(specialized intestinal metaplasia)이 존재하는 식도를 바렛식도로 정의합니다. 이 상피는 goblet 세포를 포함한 장상피와 유사합니다. 최근 영국에서는 장상피화생이 없어도 원주상피화생만 증명되면 바렛식도라 하자는 의견이 있지만 대세는 아닙니다. 우리나라에서는 식도점막에서 장상피화생을 동반한 원주상피화생이 확인되어야만 바렛식도로 정의하고 있습니다. 내시경에서 의심된다고 바로 진단하면 안됩니다. 반드시 조직검사 결과가 있어야 합니다.
바렛식도의 중요성은 식도 선암의 전구병변이기 때문입니다. 미국과 영국에서 바렛식도는 연간 0.5%(200명당 1명)에서 식도 선암이 된다고 합니다. 우리나라에서는 명확하지 않습니다. 바렛식도의 특별한 증상은 없습니다. 간혹 위산역류로 인한 가슴쓰림이나 연하장애, 토혈 등이 동반될 수 있습니다.
바렛식도는 내시경으로 진단하지만 조직검사로 특수 장상피화생을 확인해야 합니다. 바렛식도의 중요한 내시경 소견은 EGJ보다 상방으로 이동한 SCJ입니다. SCJ과 EGJ 사이의 길이에 따라 장분절 바렛식도(long segment Barrett's LSBE, >3 cm), 단분절 바렛식도(short segment Barrett's esophagus, SSBE, 1-3 cm), 초단분절바렛식도 (ultrashort segment Barrett's esophagus, USSBE, <1 cm)로 구분합니다.
고전적인 장분절바렛은 분홍색의 원주 점막이 hiatal hernia로부터 3-10 cm 가량 상방으로 뻗쳐 있으며, 바렛식도의 근위부는 수평적일 수도 있고, 혹은 원주상피가 불규칙적이고 혀처럼 뻗쳐 있는(tongue-like projection) 경우도 있습니다. 원주 점막부위 안에 잔존한 편평상피의 부위가 섬처럼 보일 수 있습니다 ("squamous island"). 바렛식도의 상연은 대개 흰색의 편평상피와 잘 구분되나, 중증 식도염이 있으면 경계가 잘 그려지지 않습니다. 단분절 바렛은 식도하부에 원주 상피 길이가 3cm 이하로 짧으며, 조직생검상 특수 장상피화생을 동반합니다. 요오드 염색을 하면 바렛상피와 정상 식도점막의 경계가 보다 선명하게 보입니다.
우리나라에서 바렛식도의 임상적 의의는 불명확합니다. 현재 하부식도 선암이 증가하고 있다는 증거가 없기 때문입니다. 장분절 바렛식도와 단분절 바렛식도의 의미도 불명확한 상태입니다. 하물며 1 cm 미만의 초단분절 바렛식도의 의미는 더더욱 불명확합니다. 바렛식도라는 진단이 붙으면 온갖 이상한 일이 벌어집니다. 불필요한 걱정, 불필요한 투약, 불필요한 치료 등등. 초단분절 바렛식도라는 차라리 언급하지 않는 편이 환자에게 유리하다고 생각합니다. 피부과에 가면 가려운 원인에 대해서 이야기 해 줍니다. 점이 몇개인지는 말해주지 않습니다. 별 의미가 없기 때문입니다. 의미없는 것은 말하지 않는 편이 낫습니다. 저는 좋은 사진 한 장 찍고, 결과지에는 아무 언급을 하지 않습니다.
사실 우리나라에서 바렛식도는 과대평가 상태입니다. 식도선암 발생률이 낮음에도 불구하고 암발생 위험이 과장되고 있습니다. 일전에 이풍렬 교수님께서 적절히 설명하셨다고 생각되어 아래에 옮깁니다.
[2014-1-25. 부산대 김광하]
서구에서 바렛식도환자의 식도선암 발생률은 1년에 0.5% 정도이다. 가장 최근의 유럽 연구에서는 1년에 0.12-0.22%로 보고되었다. 바렛식도에서 고도이형성 및 식도 선암으로 진행 인자는 고령, 남성, 바렛분절의 길이, 흡연, 바렛분절의 결절성 변화 등이다. 우리나라에서는 아직까지 바렛식도 및 식도선암의 발생률이 의미있게 증가하였다는 역학연구가 없는 상황이지만, 생활방식의 서구화 및 위식도역류질환의 증가로 인해 바렛식도가 점차 증가할 것으로 예상된다.
 2. 바렛식도의 내시경 소견과 조직검사 - 2009년 내시경학회지에 실린 저의 리뷰에서 옮깁니다.
2. 바렛식도의 내시경 소견과 조직검사 - 2009년 내시경학회지에 실린 저의 리뷰에서 옮깁니다.
1) 바렛식도의 내시경 소견
바렛식도의 가장 중요한 내시경 소견은 위식도접합부보다 상방으로 이동한 편평상피-원주상피접합부다.
편평상피-원주상피접합부와 위식도접합부의 사이 점막은 위점막과 비슷한 연어빛 원주상피인데, 근접하여 관찰하면 바렛식도의 표면은 융모 같은 패턴을 보이기도 한다. 편평상피가 원주상피로 바뀌면서 군데군데 편평상피가 남아있는 경우가 흔하며, 이를 편평상피섬(squamous island)이라고 부른다. 바렛식도에서는 위점막에서는 보이지 않는 상피하 혈관이 관찰된다. 그러나 식도염이 있거나 협착이 있는 경우에는 편평상피-원주상피접합부를 명확히 구분하기 어렵고 하부식도 상피하 혈관이 잘 보이지 않을 수 있다.
바렛식도에서 편평상피-원주상피접합부는 매우 다양한 모양을 보인다. 위식도접합부의 상방에 위치하는 매끈한 직선 혹은 부드럽게 물결치는 곡선으로 관찰되는 경우가 많지만, 손가락 모양으로 상방으로 펼쳐진 원주상피가 동반된 예도 많다. 간혹 편평상피-원주상피접합부 상방에 정상식도도 둘러싸인 원주상피섬(columnar island)이 보일 수 있다.
많은 수의 바렛식도, 특히 길이가 긴 바렛식도는 대부분 열공허니아를 동반하고 있다. 그러나 반대로 열공허니아가 있는 환자에서 위점막의 근위부가 불분명해지면서 위식도접합부를 명확히 구분하지 못하여 위점막에서 조직검사를 하여 바렛식도를 과잉진단하는 우를 범하기도 한다. 따라서 열공허니아가 있는 환자에서 위점막의 근위부를 정확하게 구분하기 어려운 경우에는 보조적으로 울타리영역 원위부를 위식도접합부로 판단한다.
2) 바렛식도의 길이에 대하여
비교적 최근까지 하부식도의 1-2 cm정도는 정상적으로도 점액원주상피로 구성될 수 있으며 식도와 위 사이의 완충영역으로 작용한다고 믿어져 왔다. 따라서 1-2 cm 정도 짧은 길이의 원주상피는 자연스럽게 무시되었다. 1983년 Skinner는 하부식도에서 원주상피의 길이가 3 cm 이상인 경우에만 바렛식도로 부르자고 주장하였고, 이후로 3 cm은 바렛식도의 진단에서 중요한 기준으로 인정되어 왔다. 이러한 기준은 실제적으로 바렛식도의 과잉진단을 방지하는 역할을 하였고, 임상적으로 나름대로 의미있는 기준이었다고 생각한다.
1994년 Spechler는 3 cm보다 짧은 길이의 하부식도 원주상피를 보인 환자의 생검조직을 관찰하여 놀랍게도 18%에서 장상피화생이 관찰된다는 중요한 논문을 발표하였다. 당시까지 정상적인 현상으로 간주되었던 3 cm 이하의 하부식도 원주상피에서도 전암성 변화로 인정되는 장상피화생이 높은 빈도로 발견된다는 그의 보고는 바렛식도의 정의에서 3 cm라는 기준이 절대적인 의미를 가질 수 없다는 것으로 해석되었다. 그 이후로 3 cm을 초과하는 바렛식도를 장분절바렛식도(long segment Barrett esophagus; LSBE), 3 cm 이하의 바렛식도를 단분절바렛식도(short segment Barrett esophagus; SSBE)로 부르게 되었다. 최근에는 이를 더욱 세분화하여 1-3 cm의 바렛식도만을 단분절 바렛식도로 부르고, 1cm 이하는 초단분절바렛식도(ultra-short segment Barrett esophagus; USSBE)로 부르기도 한다.
3) 바렛식도의 길이 측정과 Prague 법 실제 내시경을 시행하면서 길이를 정확히 측정하는 것은 매우 어려운 일인데, 흔히 위식도접합부로부터 내시경을 조금씩 빼면서 최대 길이를 정하는 것이 일반적이다. 매우 짧은 바렛식도에서는 길이를 알고 있는 조직검사 겸자를 벌려서 비교하는 방식이 좋다.
식도점막이 360도 모두 바렛식도로 변한 부위와 손가락 모양으로 부분적으로만 변한 부위가 있는 경우에는 CM 방식으로 길이를 기술하는 것이 편하다. 예를 들어 혀모양의 부분적인 바렛식도 ("tongue-like projection")를 포함한 최대 길이(M 길이)가 5 cm 이고 360도 모두 원주형으로 관찰되는 바렛식도의 길이 (C 길이)가 3 cm라면 C3M5라고 표시하는 방식이다.
4) 바렛식도의 조직검사
호주 2015년 바렛식도 가이드라인의 조직검사 부분을 소개합니다. 미국과 영국의 의견을 종합한 전형적인 서구의 의견입니다. 2cm 간격의 4 quadrant biopsy, 즉 Seattle protocol을 고수하고 있습니다. 호주 가이드라인을 옮깁니다.
Recommendation: Random four-quadrant biopsies at 2cm intervals are the mainstay for tissue sampling. (Recommendation grade B)
Practice points: Focal abnormalities such as ulcerated or nodular lesions should be targeted with biopsies and labeled before random biopsies from the rest of the mucosa as minor biopsy-related bleeding is common and may impair endoscopic views. Technological advancements in chromoendoscopy, digital enhancements and enhanced magnification complement rather than replace random four-quadrant biopsies at 2 cm. (Recommendation grade B)
Seattel protocol에 따른 조직검사를 어떻게 하는 것인지 궁금해 하는 분들이 많습니다. 아래 그림이 잘 설명해 주고 있습니다. 위식도접합부부터 위로 올라오면서 3시, 6시, 9시, 12시 방향에서 각각 조직을 얻는 것입니다. 만약 바렛 식도 길이가 5 cm라면 8개 혹은 12개의 조직검사를 해야 합니다. 위식도접하부인 0 cm 부터 시작하여 2 cm 간격으로 올라오면서 조직검사를 하라는 문헌도 있고, 0 cm는 skip하고 2 cm, 4 cm 방식으로 조직을 얻으라는 문헌도 있습니다. 여하튼 엄청 조직검사를 많이 하는 것입니다. 이게 다가 아닙니다. 사이 사이에 의심스러운 곳이 있으면 Seattle protocol과는 별도로 target biopsy를 해야 합니다.
호주나 미국 사람들이 Seattle protocol을 지키고 있을까요? 아닙니다. 마침 제가 2007년에 Seattle에 연수를 받았습니다. 그곳 젊은 의사들에게 물어보았습니다. "너희들은 Seattel protocol을 지키느냐?" 놀랍게도 Seattle에서조차 Seattle protocol을 지키는 의사는 딱 한명뿐이라고 합니다. 처음 그 protocol을 제안한 그 분 한명만 지키고 있고 다른 분들은 모두 적당히 그냥 몇 개 target biopsy를 한다고 합니다. 본 고장에서도 이 모양이니 다른 곳은 안 봐도 뻔합니다.
왜 아무도 지키지 않는 protocol이 버젓히 가이드라인에 언급되어 있을까요? "조직검사의 sensitivity를 높이기 위하여 조직을 많이 얻을수록 좋다"는 당위를 부정하기 어렵기 때문에 책이나 가이드라인에서 Seattle protocol을 말하고 있을 뿐입니다. 아무도 지키지 않는데도 말입니다. 영국에서는 아예 단 한점의 조직검사도 하지 않는 의사들이 많아서 의료계의 골치거리라는 이야기를 들은 적도 있습니다.
우리나라에서는 어떻게들 하고 있을까요? 일전에 한 모임에서 voting을 한 적이 있습니다. 아래가 그 결과입니다. 놀랍게도 Seattle protocol을 따르겠다는 분들이 20-30% 정도 있었습니다. 그런데 voting 후 개인적으로 문의를 하였더니, Seattle protocol을 따르겠다고 답변한 분들은 모두 젊고 경험이 짧은 분들이었습니다. 실제로 장분절바렛식도를 한 번도 본 적이 없는 분들이 대다수였습니다. 만약 장분절바렛식도를 만나면 그렇게 해 보고 싶다는 희망이었지 실제로 그렇게 하고 있다는 것은 아니었습니다.
우리나라에서는 어떻게 하는 것이 좋을지 고민하다가 일전에 병리학회 선생님들과 상의하였습니다. 병리학회에서 보내준 내용은 2개 이상("at least 2")의 조직검사를 하는 것이었습니다. 진단을 위해서 그렇다는 말씀입니다.
실제로 제가 어떻게 하는지 물어오는 분들이 많습니다. 저는 1 cm 미만의 초단분절 바렛식도는 무시합니다. 조직검사도 하지 않고, 결과지에 기록하지도 않고, 좋은 사진 2장 정도 남겨둡니다. 1 cm 이상의 바렛식도를 처음 발견한 경우는 조직검사를 2개 정도 합니다. 아무 곳에서나 합니다. 특별히 dysplastic 한 부위를 본 경험은 없습니다. 추적관찰에서 과거와 거의 변화가 없으면 그냥 사진만 남기고 조직검사는 하지 않습니다. 물론 조금이라도 dysplastic해 보이는 focal lesion이 보이면 조직검사를 합니다. 몇 번 해 보았는데 다 별볼일 없게 나왔습니다.
5) 바렛식도 병리학적 진단
Histological definition of Barrett esophagus is relatively simple for esophagectomy specimen. Esophageal mucosa must be changed into columnar epithelium with Goblet cell metaplasia. However, endoscopic diagnosis of Barrett esophagus is not so simple.
6) Columnar-lined esophagus (CLE)
바렛식도를 의심하였으나 조직검사에서 (specialized) intestinal metaplasia가 확인되지 않으면 columnar-lined esophagus (CLE)라고 부릅니다. 조직검사의 false negative로 인하여 바렛 식도가 CLE로 과소평가된 것일 수 있으나 어짜피 짧은 바렛 식도는 임상적 의의가 거의 없는 것입니다.
* 참고: EndoTODAY CLE cases
This is a typical case of long segment Barrett esophagus. I made the diagnosis in 2003. There was no histological evidence of dysplasia. I have done endoscopy every year. Sometimes I took some biopsies. The patients are taking PPI for a long time. Half dose every day recently. Without PPI, he has some reflux symptoms.
* 참고 바렛식도 2013년 대한위장내시경학회 증례 quiz 풀이
[Barrett's esophagus with dysplasia]
우리나라에서는 바렛식도에 뚜렷한 이형성이 동반된 예가 거의 없는 것 같습니다. 저는 한 번도 본 적이 없습니다. YouTube를 뒤져 찾을 수 밖에 없습니다.
2019년 12월 Facebook의 GINTE (group of international therapeutic endoscopy) 라는 그룹에 한 분이 소개한 Barrett's esophagus with high grade dysplasia의 내시경 치료 사진입니다. 우리나라에서는 본 적이 없는 장면인데요... 혹시 우리나라에서 이와 비슷한 증례를 경험하신 분이 계시면 제게 연락을 주시면 감사하겠습니다.
"바렛식도와 동반된 조기 식도암 및 형성이상의 치료"라는 제목으로 제가 오래 전 기고한 글을 우연히 다시 만났습니다. 다시 읽어보았는데 12년 사이에 한 마디도 바꿀 것이 없네요. 의학은 생각보다 천천히 발전합니다. (2020-7-24. 이준행)
 4. Reflux esophagitis with Barrett esophagus
4. Reflux esophagitis with Barrett esophagus
어떤 분은 역류성 식도염이 오래되면 바렛식도가 된다고 주장하기도 합니다. 저는 역류성 식도염과 바렛식도가 별개라고 여기고 있습니다. 둘 다 hiatal hernia에 의해서 발생할 수 있습니다.
어떤 환자에서 hiatal hernia, 역류성 식도염, 바렛식도가 동시에 있다면 어떻게 해석해야 할까요? Hiatal hernia에 의해 역류성 식도염이 있다가 그 결과 바렛식도가 발생한 것일까요? 아니면 hiatal hernia에 의하여 서도 다른 두 가지 방향의 현상으로 역류성 식도염과 바렛식도가 따로따로 발생한 것일까요? 저는 후자라고 생각합니다.
저의 임상경험이 짧은 탓일 수 있으나 역류성 식도염 환자를 follow-up 하던 중 과거에 없던 바렛식도를 진단한 사람은 한 명도 없었습니다. 처음부터 바렛식도와 역류성 식도염을 동시에 가지고 있던 환자는 엄청 많았습니다.
Long non-confluent erosions
Biopsy-proven Barrett's esophagus
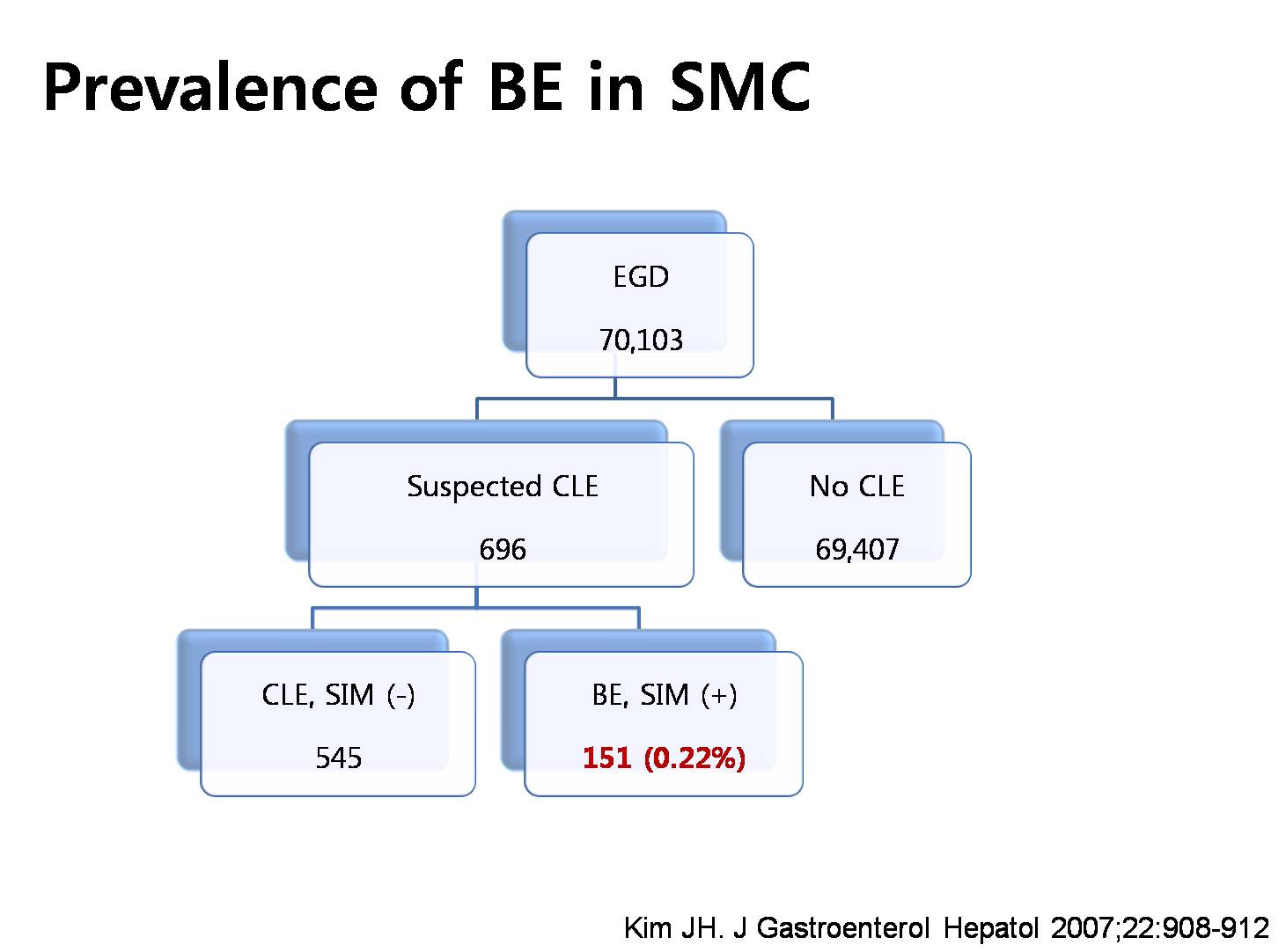 Prevalence of Barrett esophagus in Korea is not clear because of the definition problem. This is the experience of Samsung Medical Center. 0.22 percent.
Prevalence of Barrett esophagus in Korea is not clear because of the definition problem. This is the experience of Samsung Medical Center. 0.22 percent.
우리나라에서 바렛식도나 바렛식도암이 증가하고 있는지는 아직 미지수입니다.
일본에서는 바렛식도와 바렛식도암이 증가하고 있다고 합니다 (Lee HS. Clin Endosc 2014). 그러나 바렛식도와 바렛식도암에 대한 일본의 진단은 매우 특이합니다. 사소한 이상이 크게 강조되는 분위기입니다. 일본에서 바렛식도암이 실제로 증가하고 있는지 저는 확신하지 못하고 있습니다.
Do you think Barrett esophagus is increasing in Korea? It is not clear, but in a study from The Catholic University of Korea, the prevalence of Barrett esophagus is slightly increasing.
Where are we now? In the far future, it may increase, but I am not sure. It may or may not increase.
 6. 이형성이 없는 바렛식도 - 내시경 소견과 임상적 의의
6. 이형성이 없는 바렛식도 - 내시경 소견과 임상적 의의
Journal of Neurogastroenterology and Motility 2013년 10월호에 건국대학교 김정환 교수님이 기고한 Journal Club 기사를 흥미롭게 읽었습니다. 바렛식도 환자에서 내시경 조직검사에서 dysplasia가 없다고 여러번 나오면 암발생 위험이 낮다는 내용입니다. 최근 Gastroenterology에 실린 Gaddam 등의 연구를 요약한 것이었습니다. 일부를 옮깁니다.
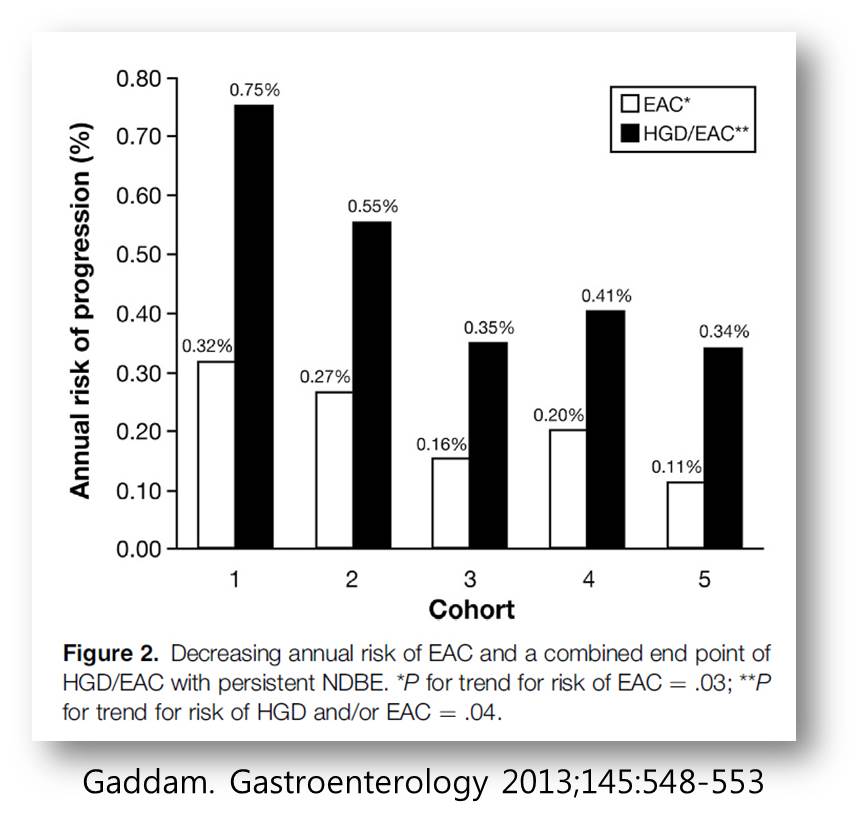
"As far as I know, this is the first study to show that patients with multiple endoscopic examinations presenting persistence of Barrett esophagus without dysplasia have a decreased risk of esophageal adenocarcinoma......
Unlike the Western countries, the Asian contries including Korea have the important distinct characteristics. First, although the prevalence of gastroesophageal reflux is increasing, the prevalence of Barrett esophagus or esophageal adenocarcinoma has remained low in most Asian countries. Second, upper endoscopic examination is easily accessible and available, especially in Korea, in contrast to the Western populations."
연구 quality가 좋으면 암발생 위험률이 낮아진다는 흥미로운 연구입니다.
The most important clinical significance of Barrett esophagus is that it is a precursor lesion of esophageal adenocarcinoma. However, there is no epidemiological evidence that the esophageal adenocarcinoma is increasing now. We have only one Barrett adenocarcinoma a year, usually, at Samsung Medical Center.
조기위암 내시경치료 후 경과관찰 중인 환자에서 발견된 심하지 않은 바렛식도이고 조직검사에서 이형성이 없었습니다. 바렛 식도에 대하여 설명을 할 것인지, 한다면 어떻게 할 것인지 고민입니다. 저는 그냥 아무 말도 하지 않았습니다. 어짜피 위암 때문에 정기적인 내시경 검사를 받을 것이므로.
[2015-8-20. 애독자 질문]
1. Dysplasia가 없는 바렛 식도의 경우 1년 뒤 내시경에서 육안적으로 dysplasia가 의심되지 않는 경우도 꼭 biopsy를 해야 하는지요? 매번 하지만 의미있는 결과를 본 적이 거의 없습니다.
2. 조직학적으로 바렛식도는 나타나지 않았지만 내시경적으로 바렛식도 의심되는 환자도 1년 뒤 내시경에서 육안적으로 특별한 변화가 없어도 조직검사는 해야 하는지요?
[2015-12-25. 이준행 답변]
2014년 Gut & Liver 지에 바렛 식도 리뷰가 있습니다. Dysplasia가 없는 바렛식도는 대강 3년 후에 추적검사를 하도록 권하고 있습니다.
서양과 우리나라는 매우 다릅니다. 서양은 우리보다 바렛 식도가 흔하고 바렛 식도가 보이면 조직검사를 여럿 시행합니다. 서양에서의 surveillance 간격은 길지만 surveillance 때에는 대부분 조직검사를 합니다. 그러나 아직까지 서양조차 바렛 식도 surveillance가 환자의 outcome을 좋게 했다는 연구 결과를 가지고 있지 않습니다.
우리나라는 서양보다 바렛 식도가 드물고 대부분 단분절입니다. Dysplasia를 동반한 경우는 거의 없습니다. 우리나라에서 바렛 식도 환자의 surveillance 내시경 간격은 바렛 식도의 중증도에 의하여 결정되지 않고 통상의 위암 검진 간격으로 진행되고 있습니다. 바렛 식도고 뭐고 할 것 없이 전 국민이 1-2년에 한번 내시경을 받게 되어있다는 이야기입니다. 우리나라는 위험도는 낮은데 내시경을 자주하게 되는 셈이므로 surveillance 내시경을 할 때마다 조직검사를 할 필요는 없을 것 같습니다.
저는 이렇게 권합니다. (Personal position statement 2015-12-25)
1) 1 cm 미만의 바렛식도가 의심되면 사진을 잘 찍어두고 결과지에 언급하지 않는다. 임상적 의의가 없는 소견으로 간주한다.
2) 1 cm - 3 cm의 바렛식도가 의심되면 사진을 잘 찍어두고 조직검사를 2개 정도 시행하고 결과지에 r/o short segment Barrett's esophagus로 쓴다.
3) 3 cm 이상의 바렛식도가 의심되면 사진을 잘 찍어두고 조직검사를 2(4)개 정도 시행하고 결과지에 r/o long segment Barrett's esophagus로 쓴다. [2019-12-20. 4개를 2(4)로 변경합니다. 4개도 많은 것 같아서]
4) Dysplasia가 있거나 의심되면 전문가에게 의뢰한다.
5) Dysplasia가 없으면 1년 후 추적내시경 검사를 시행한다. 추적내시경에서 자세히 관찰하여 특별히 의심되는 곳이 없으면 조직검사를 하지 않아도 좋다.
[2018-8-2. 이준행 추가 답변]
2015년 바렛식도 surveillance 질문에 대한 답변에서 저는 "Dysplasia가 없으면 1년 후 추적내시경 검사를 시행한다. 추적내시경에서 자세히 관찰하여 특별히 의심되는 곳이 없으면 조직검사를 하지 않아도 좋다."는 의견을 낸 바 있습니다. 그런데 2018년 8월 Clinical Endoscopy에 발표된 바렛식도의 질지표에 대한 종설을 보니 내시경을 3-5년 이내에 하지 말라는 부분이 있어서 이에 대한 의견을 냅니다.
"If systematic surveillance biopsies performed in a patient known to have BE show no evidence of dysplasia, follow-up surveillance endoscopy should be recommended no sooner than 3 to 5 years."
3-5년 이내에 검사하지 말라는 것은 여러 전제조건이 있습니다.
- 첫 내시경 검사에서 바렛 식도가 의심될 때 systemic surveillance biopsies (무지하게 많은 조직검사를 하는 시애틀 protocol을 의미합니다)를 한 경우에 간격을 늘리라는 것입니다. 그러나 우리나라에서 시애틀 protocol을 일상적으로 지키는 의사는 없습니다.
- 3-5년 후 추적 내시경 검사에서 그냥 관찰만 하는 것이 아니라 systemic surveillance biopsies (무지하게 많은 조직검사를 하는 시애틀 protocol을 의미합니다)를 또 해야 한다는 것입니다. 즉 검사 간격은 늘리되 한 번 할때에는 아주 많은 조직검사를 하라는 의미입니다.
- 내시경 검사가 고가인 서양의 자료에 근거한 지표입니다. 우리나라에서는 cost benefit가 다를 수 밖에 없습니다. 우리나라에서 내시경 검사는 싸도 싸도 너무 쌉니다.
- 우리나라에서는 바렛식도가 없더라도 위암 조기검진을 위하여 최소한 2년에 한번 내시경 검사가 권유되고 있습니다.
- 우리나라에서는 바렛식도 조직검사를 하더라도 dysplasia 여부를 정확히 판단할 수 있는 병리학자가 거의 없습니다. 환자가 없으니 병리의사의 경험도 일천합니다.
이러한 모든 점을 고려할 때 비록 외국인 의사가 쓴 종설의 취지는 이해할 수 있으나 우리나라에는 적용할 수 없는 질지표라고 생각합니다. 그래서 당분간 personal position statement를 바꾸지 않을까 합니다. 위암도 볼 겸하여 내시경은 조금 자주 하고, 육안 소견을 중시하고, 조직검사는 최소한 시행한다는 입장은 변화 없습니다.
저는 아직까지 바렛식도로 추적관찰하던 환자에서 심한 바렛식도암이 되어 이로 인해 사망한 환자를 본 적이 없습니다. 바렛식도로 추적관찰 하던 중 우연히 위암이 발견되어 치료받은 환자를 많이 보고 있을 뿐입니다. 우리나라는 아직까지 위암의 왕국입니다. 바렛식도는 명함을 내밀 수 있는 형편이 아닙니다. 바렛식도암은 희귀질환 중 희귀질환일 뿐입니다.
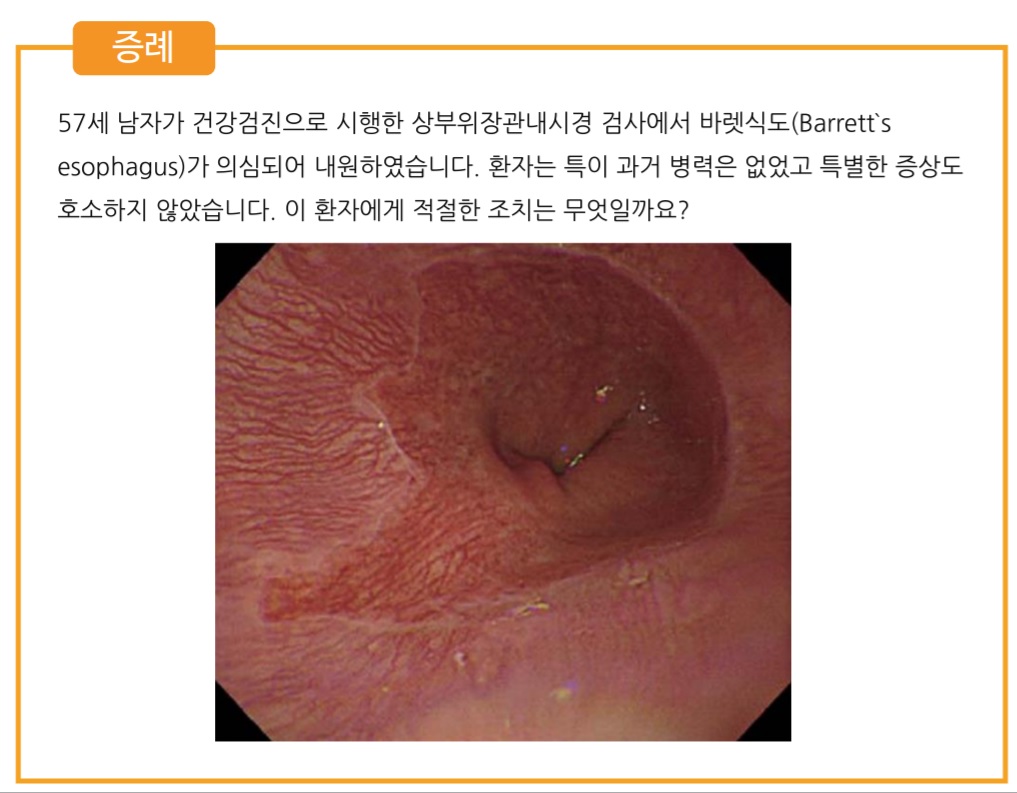 [2019년 10월] 대한소화기내시경학회 진료지침TF - 증례를 통한 임상진료지침 학습
[2019년 10월] 대한소화기내시경학회 진료지침TF - 증례를 통한 임상진료지침 학습
Journal of Gastroenterology and Hepatology 2005년 1월 Epub에 바렛식도에 대한 호주 가이드라인이 실렸습니다. 바렛식도에 대하여 가장 최근에 나온 가이드라인입니다. 흥미로운 내용이 많아 소개합니다. 일단 요약은 이런 문장으로 시작합니다. 바렛식도의 대부분은 암이 되지 않는다는 점을 명확히 밝히고 있습니다.
Barrett's esophagus (BE), a common condition, is the only known precursor to esophageal adenocarcinoma (EAC). There is uncertainty about the best way to manage BE, since most people with BE never develop EAC and most patients diagnosed with EAC have no preceding diagnosis of BE.
1) 바렛식도의 조직학적 진단: Goblet cell metaplasia가 있어야 하고, 만약 없으면 columnar mucosa without intestinal metaplasia와 같은 표현을 쓰도록 권하고 있습니다.
For the Australian guidelines however, the presence of intestinal metaplasia with morphologically typical goblet cells was considered necessary for the diagnosis of BE. Biopsies from the tubular esophagus containing columnar mucosa without intestinal metaplasia should be given a descriptive diagnosis (e.g. columnar mucosa without intestinal metaplasia), but it is currently recommended that these are not diagnosed as BE until the biological significance of this entity is clarified.
2) 조직검사는 다른 곳에서도 언급된 바 있는 2cm 간격의 4 quadrant biopsy를 고수하고 있습니다. 실제로 이대로 하고 있는지는 알 수 없습니다. 아마 아닐 것입니다.
Recommendation: Random four-quadrant biopsies at 2cm intervals are the mainstay for tissue sampling. (Recommendation grade B)
Practice points: Focal abnormalities such as ulcerated or nodular lesions should be targeted with biopsies and labeled before random biopsies from the rest of the mucosa as minor biopsy-related bleeding is common and may impair endoscopic views. Technological advancements in chromoendoscopy, digital enhancements and enhanced magnification complement rather than replace random four-quadrant biopsies at 2 cm. (Recommendation grade B)
3) 바렛식도 환자가 산역류 증상이 있을 때에만 PPI를 쓰도록 권하고 있습니다. 바렛의 regression을 위하여 사용하는 것은 권유되지 않습니다.
Symptomatic patients with BE should be treated with Proton Pump Inhibitor therapy (PPI), with the dose titrated to control symptoms. (Grade C)
There is insufficient evidence to recommend the use of acid suppressive therapy for the regression of BE (Grade B).
* [2016-6-6. 이준행 추가]
과거에는 바렛이 있어도 산역류가 있는 경우만 PPI를 투여했습니다. 최근에는 개념이 바뀌었습니다. 바렛과 산역류의 관련성이 관심을 끌고 있습니다. 아직 대규모 연구는 부족하지만 이제는 바렛이 있으면 증상이 없더라도 PPI를 투여하는 쪽으로 이야기가 모이고 있습니다.
4) Dysplasia가 없는 바렛식도에 대한 여러 종류의 ablation 치료는 모두 권유되지 않고 있습니다.
Long term outcome studies do not yet support ablation in patients without dysplasia. (Grade B) Ablation of BE should remain limited to individuals with HGD in BE who are at imminent risk of developing esophageal adenocarcinoma. (Grade B)
5) 3cm 이상의 장분절 바렛식도 환자에 대하여 2-3년에 한번 내시경과 조직검사를 하도록 권하고 있습니다. 그리고 이를 intensive surveillance라고 부르고 있군요.
Patients with Barrett's Esophagus length equal to or greater than 3cm may have intensive surveillance, possibly every two to three years following the Seattle protocol. (Grade D)
[2015-2-16. 이준행 해설]
호주에서도 "바렛이라고 부르려면 반드시 조직학적으로 Goblet cell metaplasia가 있어야 한다"고 주장하고 있습니다. 조직검사도 하지 않고 바렛이라고 부르는 것을 동의할 수 없다는 뜻입니다. 이점에서 영국보다는 미국에 가까운 가이드라인입니다. (영국에서는 의사들이 도무지 조직검사를 하지 않기 때문에 조직학적 증거가 있어야 바렛이라고 부르자는 주장을 하지 못하는 것으로 들었습니다.) 호주에서는 3 cm 이상에서 surveillance endoscopy를 권하고 있으며, 증상이 없는 사람에서 PPI를 권하지 않고 있습니다. 우리나라에서 발견되는 바렛의 대부분인 dysplasia가 없는 3 cm 미만의 단분절 바렛식도에 대해서는 투약도 추적내시경도 아무 것도 권하지 않고 있는 셈입니다. 이 정도의 바렛은 발견되도 무시하라는 말이지요.
우리나라에서는 어짜피 바렛이 있던 없던 2년에 한번 내시경 검사를 받도록 되어 있습니다. 바렛식도가 진단되더라도 뭔가를 추가할 일은 거의 없을 것 같습니다.
바렛은 우리나라에서 과대평가를 받고 있는 질환입니다. 별것도 아닌데 관심만 많은 것이지요. 의사나 환자나 모두...... 여전히 중요한 것은 위암입니다. 식도에서는 편평상피세포암이 더욱 중요합니다. 바렛식도암은 그야말로 예외 중 예외일 뿐이지요. 바렛식도암을 진단해 본 것이 벌써 몇 년 되었습니다. 참 드뭅니다. 별로 중요하지 않습니다. 바렛식도암은 희귀질환 중 희귀질환입니다. 흔한 질환이 더 중요합니다. 위암이 중요합니다.
 10. 2016 ACG 가이드라인 (Shaheen NJ. AJG 2016).
10. 2016 ACG 가이드라인 (Shaheen NJ. AJG 2016).
2016년 바렛식도 가이드라인이 나왔습니다. 제가 흥미롭게 본 부분은 아래와 같습니다.
1 cm 미만의 바렛식도 의심부위는 바렛식도로 진단하지 않도록 권하고 있습니다. 조직검사도 하지 말라고 합니다 (should not be performed).
Recommendation 2 . Endoscopic biopsy should not be performed in the presence of a normal Z line or a Z line with < 1 cm of variability (strong recommendation, low level of evidence).
BE has been traditionally defined as the presence of at least 1 cm of metaplastic columnar epithelium that replaces the stratifi ed squamous epithelium normally lining the distal esophagus. The reason why such segments < 1 cm have been classifi ed as "specialized IM of the esophagogastric junction" (SIM-EGJ) and not BE is because of high interobserver variability as well as the low risk for EAC. Patients with SIM-EGJ have not demonstrated an increase in the development of dysplasia or EAC in large cohort studies aft er long-term follow-up, in contrast with patients with segments of IM >1 cm.
바렛식도라도 dysplasia가 없으면 내시경을 너무 자주 하지는 않도록 권하고 있습니다.
Acknowledging recent data on the low risk of malignant progression in patients with nondysplastic BE, endoscopic surveillance intervals are attenuated in this population; patients with nondysplastic BE should undergo endoscopic surveillance no more frequently than every 3-5 years.
Neither routine use of biomarker panels nor advanced endoscopic imaging techniques (beyond high-definition endoscopy) is recommended at this time. Endoscopic ablative therapy is recommended for patients with BE and high-grade dysplasia, as well as T1a esophageal adenocarcinoma. Based on recent level 1 evidence, endoscopic ablative therapy is also recommended for patients with BE and low-grade dysplasia, although endoscopic surveillance continues to be an acceptable alternative. Given the relatively common recurrence of BE after ablation, we suggest postablation endoscopic surveillance intervals.
Chomoprevention으로 PPI 사용을 권하고 있습니다.
Recommendation 26 . Patients with BE should receive once-daily PPI therapy. Routine use of twice-daily dosing is not recommended, unless necessitated because of poor control of refl ux symptoms or esophagitis (strong recommendation, moderate level of evidence).
PPI therapy is common in patients with BE, in part because of the high proportion of those patients who also have symptomatic GERD. In these cases, the use of PPIs is substantiated by the need for symptom control, making consideration of chemoprevention secondary. However, even in patients without refl ux symptoms, in whom BE is incidentally found during evaluation of other symptoms and/or signs, the use of PPIs deserves consideration. Several cohort studies now suggest that subjects with BE maintained on PPI therapy have a decreased risk of progression to neoplastic BE compared with those with either no acid suppressive therapy or those maintained on H2RA therapy. In addition, the risk profi le of these medications is favorable in most patients, and the cost of this class of drugs has diminished substantially in recent years because of the availability of generic forms of the medications.
These factors, combined with the theoretical consideration that the same infl ammation that may be in part be responsible for pathogenesis of BE may also promote progression of BE, make the use of PPIs in this patient population appear justifi ed, even in those without GERD symptoms. Given the low probability of a randomized study of PPI use in BE, decisions regarding this intervention will likely rely on these retrospective data and expert opinion.
[IDEN2017] Endoscopy of the lower esophagus for the detection of Barrett's esophagus and related neoplastic conditions. Lars Aabakken (Deptment of Medicine, Rikshospitalet University Hospital, Norway. lars.aabakken@medisin.uio.no)
WATS3D - 회전하는 brush를 이용하여 많은 sample을 얻은 후 3D scan을 하여 입체적으로 분석하는 새로운 방법입니다.
특별한 brush를 이용하여 조직을 얻은 후 computer를 이용하여 3-D로 조직학적 관찰을 할 수 있다는 것입니다.
최근 발간된 유럽 바렛 가이드라인을 소개하셨는데 저는 두 가지가 중요한다고 생각했습니다. (1) 1 cm 미만은 무시하라는 것("a minimum length of 1 cm")과 (2) 조직검사로 specialized intestinal metaplasia가 필요하다는 점입니다. 반가운 마음에 다음과 같이 질문하였습니다. "Overdiagnosis can be a big problem, so I strongly agree with your first statement that the minimum length of columnar metaplasia is 1 cm for the diagnosis of Barrett's esophagus. In Korea, early stage Barrett-associated adenocarcinomas are usually realated with short segment Barrett esophagus, and some of them is very short, less than 1 cm. Do you often see Barrett-associated adenocarcinoma in a very short Barrett esophagus?" 2009년 삼성서울병원에서 경험하였던 Barrett's adenocaricnoma에 대한 짧은 보고를 낸 적이 있습니다 (김상중. 대한소화기내시경학회지 2009).
정대영 교수님께서 "Seattle protocol을 따르는 의사가 얼마나 되는가?" 질문을 하셨습니다. 연자는 "very few"라고 답하였습니다. 가이드라인에서는 2cm마다 4 quadrant biopsy를 하는 Seattle protocol이 언급되는데, 너무 번거롭기 때문에 임상에서 이를 따르는 사람이 very few 한 것 같습니다. 다음 연자인 Ponchon은 42%라고 자랑스럽게 답했습니다.
[IDEN 2017] Risk evaluation and treatment for Barrett's esophagus and related neoplasia in the Western countries. Thierry Ponchon
1) Photodynamic therapy는 부작용이 너무 많습니다. esophageal stenosisrk 36%.
2) Radiofrequency ablation: 최근 메타분석에서 intestinal metaplasia (= 바렛) 재발 9.5% Dysplasia 발생 2.0%, carcinoma 1.2%
3) Cryotherapy는 대강 radiofrequency와 비슷합니다.
4) EMR - Piecemal EMR is not abandoned.
5) ESD - 연자는 "If there is any mucosal abnormality, ESD for me."라고 말했습니다.
Floor에서 non-dysplasitc Barrett에서 PPI의 역할에 대한 질문이 있었는데, 연자는 "증상이 없으면 PPI를 쓰지 않는다"고 답했습니다. 이 부분에 대한 전문가들의 의견은 아직 하나로 모이지 못하고 있지만, 최근에는 증상이 없더라도 PPI를 투여하는 쪽으로 데이타가 모이고 있습니다. 2016년 5월 9일 월요점심집담회에서 이풍렬 교수님께서 보여주셨던 슬라이드를 소개합니다. 저의 경험에 의하면 long segment Barrett esophagus 환자는 대부분 증상이 있었던 것 같습니다. 증상이 있는 경우에는 당연히 PPI를 처방하였지만, 혹시 증상이 없는 long segment Barrett esophagus 환자가 오더라도 PPI를 처방할 생각을 갖고 있습니다 (심평원 기준은 아니지만...)
[IDEN 2017] Risk evaluation and treatment for Barrett's esophagua and related neoplasia in the Eastern countries. (아산병원 김도훈)
日本은 확실히 특이합니다. Palisading vessel을 기준으로 삼는 곳은 일본밖에 없네요...
日本은 확실히 특이합니다. Barrett esophagus가 현저히 증가하는 곳은 일본밖에 없네요...
Seattle protocol을 따라 조직검사를 하는 의사의 비율을 조사한 결과입니다. [이준행 comment] 제가 보기에는... 현실은 이보다 훨씬 훨씬 적을 것 같습니다. 아직까지 한 명도 만난 적이 없습니다. 일전에 한 모임에서 이와 비슷한 질문을 한 적이 있는데, 'Seattle protocol에 따라 엄청나게 많은 조직검사를 하겠다'고 답한 선생님께 문의하였습니다. "정말 그렇게 많이 하십니까?" "아니요, 아직까지 한번도 그렇게 해 본 적이 없습니다. 앞으로 그런 환자를 만나면 그렇게 해 볼 생각이라는 것일 뿐입니다." 그렇습니다. Seattle protocol은 현실적이지 않고, 필요하지도 않다고 생각합니다. 설문조사는 현실을 정확히 반영하고 있는 것은 아닙니다. 그냥 꿈일뿐...
Long-segment Barrett esophagus와 연관된 adenocarcinoma를 멋지게 ESD로 치료한 증례를 보여주셨습니다. 노란색으로 표시한 부분을 제외한 거의 330도 정도 ESD였습니다. [이준행 comment] 저는 아직까지 비슷한 증례를 한 명도 경험한 적이 없습니다. 모두 short 또는 ultrashort segment Barrett esophagus와 관련된 바렛식도암이었습니다. 그래서 질문을 했는데요, 김도훈 선생님도 "long-segment Barrett esophagus와 연관된 adenocarcinoma를 ESD로 치료한 경험은 딱 1예였다"고 답하셨습니다. 그렇습니다. 매우 드문 일입니다. 김도훈 선생님의 멋진 치료 축하합니다. 대단한 실력입니다.^^
[2024-10-18] SMC Friday Morning Endoscopy Conference
[2025-9-16. SMC 화요아침내시경세미나]
1) EndoTODAY FAQ on Barrett esophagus
2) 바렛식도 - 내시경진단을 중심으로. 이준행. 대한소화기내시경학회지 2009. PDF
3) 바렛식도의 진단과 치료에 대한 한국 의사들의 견해. 김갑현, 이준행. 대한소화관운동학회지 2009. PDF
5) 단일 기관에서 경험한 바렛식도암의 임상적 고찰. 김상중, 이준행. 대한소화기내시경학회지 2009. PDF
6) 바렛암: 보초용종과의 구별을 포함하여. 이준행. 2015 내시경세미나. PDF
7) EndoTODAY 보초용종 sentinel polyp
8) Palisade
9) 2022년 종설 이용강
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.