 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [제7회 Web-seminar]
[제7회 Web-seminar]
SPC 진료의뢰센터와 함께 Web-seminar를 진행하고 있습니다 (문의: 02-3410-0506). 2015년 11월 3일 (화) 저녁 7시 '식도암 및 다양한 식도질환의 내시경 진단' 시간에 나온 질문 일부에 대한 답변을 드립니다. Web으로 참여해 주신 모든 분들께 다시 한번 감사드립니다. (사전등록 133명 중 83명이 참석하셨습니다. 사전등록 대비 참석율 62.4%) 그 중 9명의 선생님의 질문모음입니다.)
다음 Web-seminar는 12월 8일 (화) 저녁 7시이며 제목은 '우리나라 조기위암 내시경 치료의 현황'입니다 (링크).
 [2015-11-4. 웹세미나 질문]
[2015-11-4. 웹세미나 질문]
Esophageal melanosis의 경험이 없어서 그런데, Esophageal phlebectasia와 구별이 용이한지요? 구분이 잘 안가면 Cushion sign을 확인하는 것이 도움이 되겠는지요?
[이준행 답변]
Phlebectasia는 혈관이 늘어난 것으로 쉽게 구분될 것 같습니다. Cushion sign을 볼 정도로 크게 혈관이 늘어난 경우보다는 약간 가볍게 확장된 경우가 많다고 생각합니다.
@ 참고자료: EndoTODAY melanocytosis
식도의 nevus와 구별은 어떻게 하나요?
[이준행 답변]
저도 식도 nevus는 본 적이 없어서 정확히 답변하기는 어렵지만 문헌에는 아래와 같이 나와 있었습니다. 조직검사에서 heavily pigmented dendritic melanocytes가 특징인 것 같습니다.
Melanocytic nevi are uncommonly seen in the esophageal mucosa. To our knowledge, only a single case of blue nevus is found in the literature, and this was reported by Lam et al from a 52-year-old Chinese woman who presented with linear patches of bluish pigmentation in her lower esophagus. Like its cutaneous and mucosal counterparts, this is characterized by the presence of dendritic melanocytes in the subepithelial connective tissue without junctional melanocytic activity. The absence of cytologic atypia and the presence of heavily pigmented dendritic melanocytes in stromal tissue differentiate the lesion from melanoma and melanocytosis. (Chang. Arch Pathol Lab Med 2006)
@ 참고자료: EndoTODAY melanocytosis
식도접합부나 위문부에서 등에서 조직검사시 접근방법이 좀 어려울 때가 많고 출혈이 항상 걱정됩니다. 안전하게 조직검사를 위한 팁이 있나요?
[이준행 답변]
식도 위 접합부, 특히 하부식도부위는 palisading vessel이라고 하여 혈관이 점막층에 존재합니다. 조직검사를 하면 피가 많이 나오는 이유입니다. 그러나 작은 혈관이므로 이내 멎습니다.
GE junction 상방에서 조직검사상 papilloma로 확인됐지만 사이즈가 2cm 이상이어도 follow up만 해도 되는 건지요?
[이준행 답변]
Papilloma는 benign입니다. 조금 크더라도 치료대상은 아닌 것 같습니다. 아래 사진은 조금 비전형적이지만 크고 경과관찰 했던 papilloma입니다.
Papilloma 몇 증례를 소개합니다.
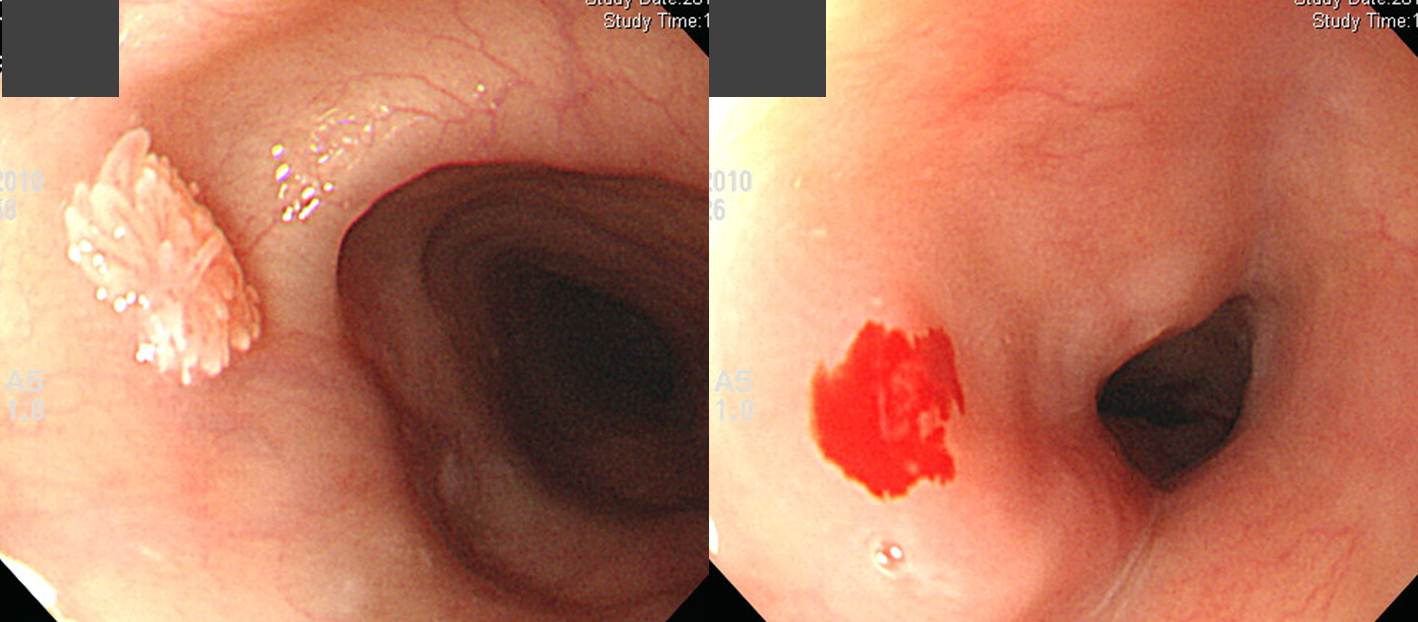
식도 유두종은 매우 흔합니다. 유두종은 premalignant lesion이 아니므로 구태여 무리해서 제거할 필요는 없다고 생각됩니다. 그러나 식도에 혹이 있다는 생각에 매우 불안해 하시는 분도 있습니다. 그러한 경우에는 내시경 조직검사를 통하여 작은 유두종을 제거해버리면 좋습니다. 오늘의 증례에서는 조직검사 forcep으로 병소의 아래쪽을 잡아 한 번에 제거할 수 있었습니다. 환자가 무척 좋아했던 것은 당연한 일입니다. (EndoTODAY 2009. 2. 27.)
Hiatal hernia, reflux esophagitis가 있던 환자의 하부식도 유두종을 절제함

Sentinel polyp으로 생각하고 절제하였는데 조직검사는 유두종으로 나옴.
식도관찰에 NBI가 도움이 되나요? 특히 식도암에 대해서?
[이준행 답변]
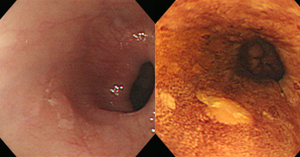
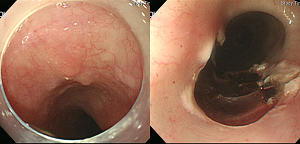
식도암 고위험 환자(두경부암, 식도암 내시경치료 과거력)에서 비확대 NBI 소견에 대한 최근 논문(Nagami. Am J Gastroenterol 2014)을 소개하는 것으로 답변을 대신합니다. 식도암에서 NBI의 유용성은 확대내시경을 이용할 때 뚜렷합니다. 일반적인 상황에서는 확대내시경을 이용하기 어려우므로 통상의 비확대 내시경에 NBI를 적용합니다. 이 방법(비확대 NBI)의 유용성에 대한 자료가 부족한 상황입니다.
결론은 고위험환자의 screening endoscopy에서 NBI는 Lugol chromoendoscopy를 대체할 수 있다는 것입니다. 아래 표에서도 실선 박스 3명을 제외한 29개의 고도이형성/식도암 병소가 비확대 NBI에서 발견이 되었기 때문입니다. 이 정도의 sensitivity면 screening endoscopy 용도로는 충분하다고 생각됩니다. 괜히 Lugol을 뿌리느라 고생할 필요도 없고 너무 많은 Lugol void area 때문에 혼란을 겪을 이유도 없습니다.
두경부암이나 식도암 내시경치료 과거력과 같은 고위험 인자가 없는 보통의 내시경에서 NBI를 사용해야 하는지는 미지수입니다. 여러 의견이 가능하겠지만 저는 식도의 관찰은 통상의 내시경(white light endoscopy)이면 충분하다고 생각합니다. NBI를 무분별하게 사용하여 검사의 sensitivity를 무한히 높일 이유는 없을 것 같습니다. Screening에서는 효과와 위험의 균형이 중요하기 때문입니다.
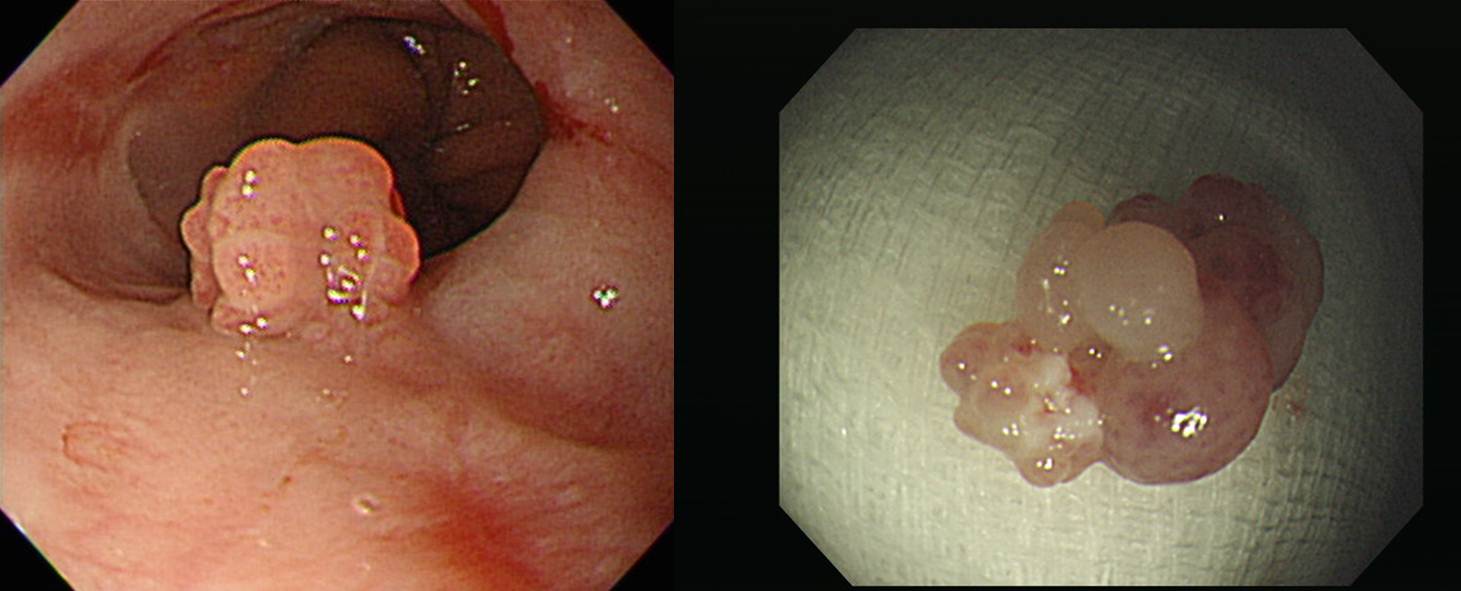
조기식도암 비확대 NBI 소견을 몇 개 소개합니다.
십이지장 bulb에 diverticulum에 음식 걸려서 obstruction 되어 forcep으로 음식을 뜯어낸적이 있는데 이것에 대해서도 내시경수술이 있나요?
[이준행 답변]
Zenker diverticulum 및 기타 식도 게실의 상당수는 endoscopic septal incision으로 치료할 수 있습니다 (Zenker 게실의 내시경 치료). 그러나 십이지장 게실은 식도쪽과 발생 기전도 다르고 벽도 얇고 천공 시 위험성도 높아서 내시경치료는 잘 하지 않는 것으로 알고 있습니다.
@ 참고: EndoTODAY 십이지장 게실
위암으로 STG billoth II 수술 한 분들은 distal 어느 부위까지 검사해야 하나요? (가능한 데까지?)
[이준행 답변]
가능한 데까지 들어가 볼 필요는 없습니다. 그냥 식도, 잔위, 그리고 소장의 맨 처음 5 cm 정도만 보시면 충분합니다. 잔위암과 문합부의 재발을 보는 것이 중요한 목표입니다.
@ 참고: EndoTODAY 수술 후 내시경 소견
(1) 연간350 여개 쯤 내시경 하는 병원인데 루골을 꼭 준비하는게 좋을까요? 메틸렌블루밖에 없어서요.(2) Lugol's solution 이 실험실용과 내시경용(인체용)이 따로 있는지요? (3) 내시경시 Lugol 원액을 희석해야하는지요?
[이준행 답변]
소화관 점막표면에 각종 색소를 살포 또는 분무하여, 점막의 미세한 요철이나 색조의 변화를 알기 쉽게 하거나, 점막과 색소간의 특수한 기능을 이용하여, 보통 내시경 관찰에서는 잘 보이지 않는 소견을 쉽게 관찰할 수 있도록 하는 것이 색소내시경(chromoscopy)입니다. 메틸렌 블루, 인디고카르민 등 여러 종류의 색소가 쓰입니다. 이 중 식도질환의 진단에는 요오드법(Lugol법)이 유용합니다. 보통 2 - 3 % 용액을 5 - 10 mL 정도 사용합니다.
루골용액이 편평상피 내의 글리코겐과 반응하여 변색되는 것을 이용한 반응법으로, 정상 구강 내, 인후두, 식도점막 등등이 편평상피로 덮여 있으므로 요오드에 의해 수분 내에 갈색으로 변색됩니다. 염증에 의한 편평상피의 결손, 재생상피, 이형상피, 암에서는 글리코겐의 농도가 떨어져 황백색의 염색이 되지 않는 부위(Lugol void area)가 형성됩니다.
묽게 염색된 영역은 경도~중등도의 이형상피인 경우가 많습니다. 양성의 경우 크기가 작고 원형의 모습이며, 악성의 경우 주위가 불규칙하고 크기가 10mm 이상인 경우가 많습니다.
일반 내시경에서 점막절제술에 적합한 식도의 표층성 암을 찾아내기는 매우 어렵다고 알려져 있으며, Lugol 법을 이용하여 염색이 되지 않는 부위에서 생검을 함으로써 발견율을 높일 수 있다고 합니다. 그러나 이러한 접근법이 실제로 환자의 생존기간을 늘리는데 얼마나 도움이 되는지는 명확하지 않습니다.
개업가에서 루골을 준비할 필요는 없을 것 같습니다. 일반적인 검사에서는 white light endoscopy로 잘 관찰하면 충분합니다.
최근 Lugol이 의학용으로 허가받지 못하였다고 사용이 중지되었습니다. 의학용으로 허가받은 Lugol이 곧 도입될 것이라는 소문은 들었는데 정확히는 잘 모르겠습니다.
@ 참고: EndoTODAY 색소내시경
B형 간염 바이러스 보균자들은 일회용 forcep을 써야 되는지요? (왠지 모든 사람을 다 쓰면 지구를 혹사시킬 거 같아서요. )
[이준행 답변]
Reusable forcep도 규정대로 잘 소독하면 문제가 없습니다. EO 가스 소독이 표준입니다. 정확하지는 않지만 autoclav도 문제가 없다는 이야기를 들은 적이 있습니다. 그러나 포르말린에 담근 것으로는 부족하다고 알고 있습니다.
Reusable forcep을 규정대로 소독하기 어려운 개업가에서는 1회용 포셉을 쓰는 것이 좋습니다.
감염 고위험 환자를 screening 한 후 내시경 검사를 하는 것은 아닙니다. 따라서 모든 환자를 감염 고위험군으로 가정하고 검사하는 것이 원칙입니다. 즉 universal precaution이 필요합니다. 그러나 이미 감염 고위험군으로 알고 있다면 1회용 forcep을 우선적으로 사용하는 것은 타당한 전략이라고 생각합니다.
예전에 학회에서 NSAIDs와 gastric ulcer에 대한 강의를 들었는데, 소화기내과 교수님이 H2 blocker는 2주 지나면 내성(?)이 생긴다고 하셨는데 혹시 자세히 설명해 주실 수 있는지요?
[이준행 답변]
H2RA는 훌륭한 위궤양 치료제입니다.
H2RA는 위식도역류질환의 치료에도 사용될 수 있습니다. 그러나 효과가 별로입니다. 비단 tolerance 문제가 아니더라도 약효가 불충분합니다. H2RA를 쓰던 위식도역류질환 환자에게 PPI를 권하여 현저하게 좋아진 경우를 많이 보았습니다. PPI는 H2RA보다 투약 횟수가 적고, 부작용 profile도 못하지 않고, 가격면에서도 크게 불리하지 않기 때문에 현 시점에서 위식도역류질환의 일반적인 치료에 H2RA를 쓴다는 것은 nonsense입니다. 단지 정책당국에서 PPI에 대한 삭감을 너무 많이 하고 있어서, 의료기관이 이에 적응한 결과일 뿐입니다.
Aspirin을 포함한 NSAID를 사용하는 환자 중 상부위장관 합병증의 고위험군에서는 예방조치가 필요합니다. 이러한 견해는 2009년 가이드라인에 상세히 기술하였습니다. 세 가지 전략을 제시하였는데요, 사실은 한 가지입니다. Misoprostol은 부작용이 많아 실제로 적용하기는 어렵습니다. Cox-2 selective agent로 바꿀 수 있는 경우는 많지 않습니다. 진통효과가 약하기 때문입니다. 그래서 결국 PPI를 추가하는 것 이외에 마땅한 방법이 없습니다. 다만 PPI 용량에 대한 논란은 남아있습니다. 여하튼 NSAID나 aspirin 관련 위장관 부작용을 예방하는데는 H2RA는 효과가 없고 PPI가 효과적이라는 것은 consensus입니다. 현재 NSAID 관련 합병증을 막기 위하여 H2RA를 쓰는 것은 (1) 가이드라인에 없고, (2) PPI보다 훨씬 못하다고 밝혀졌고, (3) H2RA를 쓰면 masking 효과때문에 오히려 합병증이 많아질 우려까지 제기된 상태입니다.
H2 blocker가 장기 치료로 효과가 떨어지는 이유는 (1) 위산분비능력이 약하다는 점과 (2) 처음에는 그나마 위산을 상당히 억제하지만 몇일이 지나면 위산분비억제 효과가 현저히 떨어진다는 점 (tolerance) 때문입니다.
Sliding hiatal hernia 의 내시경 진단에서 Schazki's ring 이 필수적인것인지요?
[이준행 답변]
Schatzki ring은 B-ring (= mucosal ring)이 현저하면서 fix된 경우를 말합니다. Sliding hiatal hernia가 심하면서 협착을 동반한 경우라고 생각하면 됩니다. 모든 sliding hiatal hernia에서 Schatzki ring이 보이는 것은 아닙니다.
@ 참고: EndoTODAY hiatal hernia
조기식도암의 Depth of invasion 이 M2 인 경우, 일본 연구 결과를 근거한다면, 추가로 수술해야한다는 Consensus 는 없는지요?
[이준행 답변]
좋은 질문입니다. 식도암은 M2부터 림프절 전이가 있기도 하고 M3부터는 제법 많습니다. 일전에 제가 T1 식도암의 림프절 전이 위험성을 분석한 바 있습니다 (J Gastroenterol Hepatol 2008). 결과 부분을 옮기면 아래와 같습니다.
"The frequency of lymph node involvement was 6.25% (4/64) in mucosal cancers and 29.3% (39/133) in submucosal cancers (P < 0.001). In patients with M1 (n = 32) and M2 (n = 14) cancers, no lymph node metastasis was found. In multivariate analysis, size larger than 20 mm, endoscopically non-flat type, and endo-lymphatic invasion were significant independent risk factors for lymph node metastasis. "
M3 암에서 림프절 전이가 갑자기 많아지고, SM에서는 더욱 많다는 점이 중요합니다. 위암에서도 depth of invasion에 따라 림프절 전이가 많아지지만 식도암에서는 그 차이가 더욱 현저합니다.
M3 식도암 중 림프절 전이를 보인 것은 대부분 장경 20mm 이상이었습니다. 그러나 장경 10 mm 분화형 M3 식도암에서 림프절 전이를 보인 증례도 있었습니다.
일본에서의 보고에 의하면 M2 식도암에서도 간혹 림프절 전이가 있다고 합니다 (Kodama. Surgery 1998).
요컨데 depth of invasion이 비슷하다면 위암보다 식도암에서 림프절 전이가 많습니다.
식도암 내시경 치료 후 병리결과에 따른 추가치료의 원칙은 아직 확립되어 있지 않습니다. 위암 내시경 치료 후 병리학적으로 불완전 절제나 재발위험이 높은 것으로 나오면 바로 수술을 하면 그만입니다. 그러나 식도에서는 수술의 morbidity와 mortality가 높기 때문에 위 ESD 후처럼 쉽게 수술을 결정할 수 없습니다.
식도암은 M3 병소에서부터 림프절 전이의 위험이 높으므로 M2로 추정되는 병소가 치료의 적응증입니다. 그러나 실제 내시경 치료를 해보면 M3나 minute SM invasion이 있는 것으로 나오는 수가 많습니다. 이를 모두 수술할 수도 없는 일이고 안 할 수도 없는 일입니다. 현재의 관례는 M3는 경과관찰을 하고 SM invasion이 있으면 수술이나 chemoRT를 추가하는 것입니다.
일본에서는 minute SM invasion이 있는 경우 혹은 M3의 경우에서 chemoRT를 권하는 경우가 있습니다. 최근 보고된 일본 연구를 소개합니다.
- From November 2004 to June 2010, 120 patients with superficial ESCC were treated by ESD at the Shiga University.
- Among the 120 patients, invasion to the muscularis mucosa or to the submucosal layer was pathologically observed in 18 patients and 14 of these received additional CRT instead of surgery.
- Radiation therapy was delivered 5 days per week at 2 Gy per fraction. The total dose was 40 Gy in 20 fractions over 4 weeks. The chemotherapy regimens consisted of 5-fluorouracil and cisplatin.
- No recurrence for 45 months.
수년전 교훈적인 증례를 경험한 바 있습니다. 조기식도암에 대한 내시경 치료를 하였고 depth of invasion은 M3가 나왔으나 endolymphatic tumor emboli가 양성이었습니다. 이를 확인하기 위하여 immunohistochemistry (D2-40)를 시행하였을 때 positive in endolymphatic tumor emboli였습니다. 여러분은 어떻게 하시겠습니까?
수술을 권하였고 수술 후 병리결과에서 39개의 림프절 중 1개에서 전이가 있었습니다. 식도암 내시경 수술 후 추가치료 여부를 결정하는 것은 어렵고도 중요한 일입니다. 좋은 병리과 의사 없이 식도암 내시경 치료를 한다는 것은 말이 되지 않습니다.
삼성서울병원 파트너즈 센터 소식지에 Webinar에 대한 기사가 실렸습니다.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.