 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
001 | 101 | 201 | 301 | 401 | 501 | 601 | 701 | 801 | 901 | 1000
갈수록 안 좋아지는 환자가 있습니다. 질병 상태가 급격히 나빠진다는 의미는 아니고, 환자입장에서 진단과 치료가 점차 심해지는 경우가 있다는 말씀입니다. 사실 그런 경우는 적지 않습니다. 조기위암 같고 수술로 끝날 것 같다고 설명하고 수술했는데 진행성 위암으로 나오고 항암치료까지 받아야 하는 환자도 그런 경우입니다.
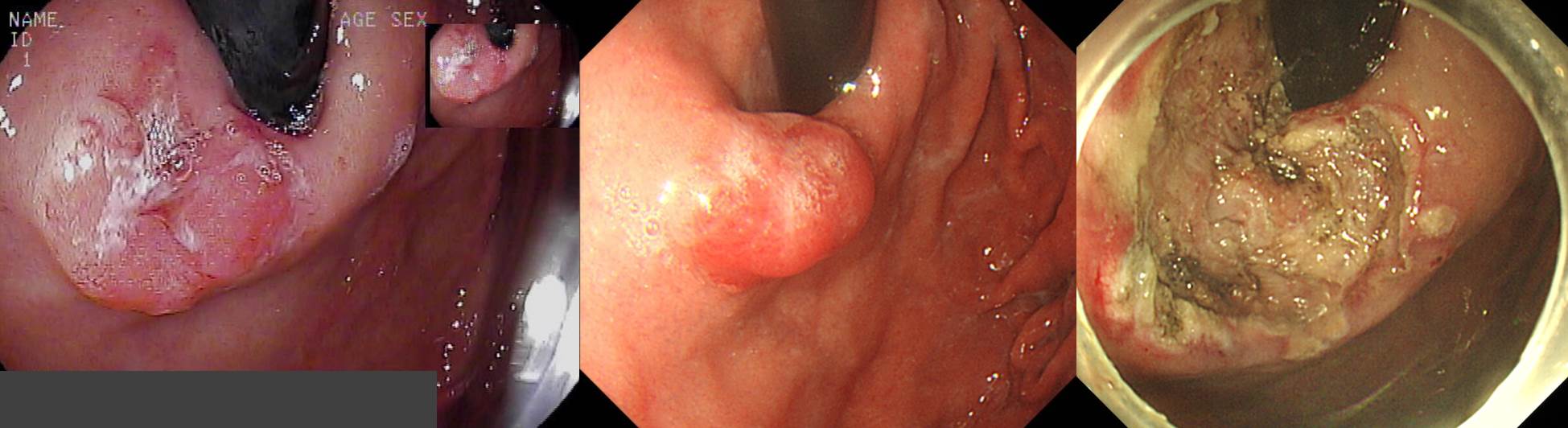
외부 검진 내시경에서 cardia의 병소가 발견되었고 조직검사에서 high grade dysaplasia가 나와 의뢰되었습니다. 외부 슬라이드를 재판독한 결과는 tubular adenocarcinoma (W/D)였고, 본 병원에서 내시경 재검한 결과는 tubular adenocarcinoma (M/D)였습니다. 85% 정도의 초기성공률을 예상한다고 설명하고 ESD를 하였는데 아래의 결과였습니다.
Stomach, endoscopic submucosal dissection:
. Early gastric carcinoma
1. Location : cardia
2. Gross type : EGC type IIa+IIb
3. Histologic type : tubular adenocarcinoma, moderately differentiated (95%) >> signet ring cell carcinoma (5%)
4. Histologic type by Lauren : mixed
5. Size of carcinoma : (1) longest diameter, 24 mm (2) vertical diameter, 19 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 1800 ㎛) (pT1b)
7. Resection margin : deep resection margin involved by carcinoma with cauterized artifacts safety margin : distal 3 mm, proximal 2 mm, anterior 10 mm, posterior 2 mm, deep 0 mm (sm only)
8. Lymphatic invasion : present
9. Venous invasion : present
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: present
ESD 병리 결과 다수의 안 좋은 소견이 있었습니다. (1) Signet ring cell carcinoma가 5% 섞인 미분화 혼재암, (2) deep SM invasion, (3) vertical resection margin involvement, (4) lymphovascular invasion이 그것입니다. 수술을 권하였습니다.
Stomach, radical total gastrectomy:
. Status post endoscopic submucosal dissection
. No residual tumor
1) Location: cannot be determined (no residual tumor)
2) Gross type: cannot be determined (no residual tumor)
3) Histologic type: cannot be determined (no residual tumor)
4) Histologic type by Lauren: cannot be determined (no residual tumor)
5) Size: cannot be determined (no residual tumor)
6) Depth of invasion: cannot be determined (no residual tumor)
7) Resection margin: free from carcinoma
8) Lymph node metastasis : no metastasis in 31 regional lymph nodes (pN0)
9) Lymphatic invasion: not identified
10) Venous invasion: not identified
11) Perineural invasion: not identified
12) Peritoneal cytology: negative
약간의 우여곡절이 있었지만 최종 수술 결과에서 no residual tumor, no lymph node involvement였습니다. 적절한 적응증으로 ESD를 시행한 후 수술이 필요한 결과가 나왔을 때, 수술 후 최종 병리결과에서 residual tumor나 lymph node 전이가 확인되는 경우는 10-20%입니다 (Kim ER. Br J Surg 2015).
이 환자를 처음부터 수술을 했으면 어떠하였을까, EUS를 했더라면 어떠하였을까 질문이 가능할 것 같습니다. 물론 EUS에서 SM invasion이 의심되는 결과가 나왔을 수도 있지만, EUS 소견만으로 처음부터 total gastrectomy를 권하기는 어려웠을 것 같습니다. 저는 ESD 전 EUS를 거의 하지 않습니다 (EndoTODAY ESD 전 EUS는 유용한가? No). 아래는 2015년 Osaka 대학에서 내시경과 EUS를 적절히 사용하는 방법을 제안한 algorithm입니다 (Tsujii Y. GIE. 2015). "CE (conventional endoscopy) accurately revealed mucosal cancer, and EUS efficiently salvaged the lesions that were over-diagnosed by CE."라고 쓰고 있습니다. '위내시경에서 점막하암으로 추정되더라도 혹시 점막암일 가능성이 있을 때만 선택적으로 EUS를 시행하여 환자에게 도움을 준다'는 아이디어입니다. ESD를 고려할 환자에서는 EUS가 필요하지 않고, 점막하암으로 생각되어 수술을 고려한 환자에서는 EUS를 해 보아서 점막암처럼 보이면 ESD를 하자는 방향입니다. 즉 EUS를 해서 수술할 환자를 ESD 하는 경우는 있지만, 그 반대의 경우(EUS 결과 의거 수술을 권함)는 없다는 것이 이들의 제안입니다. 국내에서도 이들의 방침과 같은 주장을 한 team이 있습니다. 전적으로 동의합니다.
이 정도의 병소는 일단 ESD를 하고 최종 병리결과에 의존하여 추가 치료 여부를 결정하는 것이 저의 진료 style이며, 대부분의 ESD 전문가들도 비슷한 생각을 가지고 있는 것으로 알고 있습니다. 가장 중요한 것은 ESD 병리 결과 수술이 필요하다고 나오는 경우 반드시 수술을 받으셔야 한다는 것을 사전에 잘 설명하는 것입니다. 다짐(혹은 각서)을 받아두는 것이 필요한 일이라고 생각합니다. 설명하고, 또 설명하고, 또 설명하고, 또 설명하는 수 밖에 없습니다. 저는 병리결과에 따라 수술이 필요한 경우가 15%임을 최소한 10번 설명하고 있습니다. 첫 외래에서 설명하고, 검사 후 결과보러 왔을 때 설명하고, 시술 전 회진 때 설명하고, 시술 직후 내시경실에서 절제병소를 보여드리면서 설명하고, 병동에서 회진돌 때 설명하고, 퇴원 직전 다시 한번 설명합니다. 간호 파트에서도 이와 비슷하게 여러번 설명합니다. 환자 안내서에도 씌여 있고, 환자에게 보여드리는 동영상에서도 강조되어 있습니다. 그러니... 합이 10번을 훌쩍 넘습니다. 이 정도는 되어야 환자가 수술을 받습니다. 설명이 부족한 상태에서 ESD를 하고 난 후 수술을 권하면 환자와의 랍보가 급격히 깨집니다. 급기야 병원을 옮겨 수술받는 환자도 발생합니다.
외래 자료. 예상보다 깊거나 넓은 경우가 15%-20%이며, 이 경우 "수술하셔야 합니다"라고 강조하고 있습니다.
환자 입장에서는 (1) 처음에는 dysplasia로 설명을 들었고, (2) 다음에는 암이니 85% 정도의 초기성공률을 예상하는 상태에서 ESD를 해보다는 제안을 받았고, (3) 결국에는 total gastrectomy가 필요하다는 권유에 따라 수술을 받았습니다. '갈수록 태산'이라는 말이 생각납니다. 결과는 좋았습니다. 저로서는 최선의 선택이었다고 판단하였습니다.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng. (2017-9-17)