 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [결핵성 위장질환. Gastrointestinal tuberculosis] - 終
[결핵성 위장질환. Gastrointestinal tuberculosis] - 終
1. 식도 결핵 Esophageal tubuerculosis
2. 위 결핵 Gastric tuberculosis
3. 십이지장 결핵 Duodenal tubercuosis
4. 장 결핵 Intestinal tuberculosis
5. 결핵성 복막염 Tuberculous peritonitis
6. 복부 결핵성 림프절염 Abdominal tuberculous lymphadenitis
7. 결핵성 후두염 Tuberculous laryngitis
8. FAQ
9. References
EndoTODAY 식도결핵을 참고하시기 바랍니다.
위장관 결핵은 회맹부에 호발합니다. 위결핵은 매우 드물고 대부분 이차성입니다. 특징적인 내시경 소견은 없으며 점막의 비후나 발적, 불규칙한 미란이나 궤양을 보일 수 있습니다. 일반적인 궤양치료로 호전되지 않는 경우에 의심할 수 있습니다.
2018년 12월 소화기학회지에 출혈로 내원한 위 SMT 양상의 결핵 증례가 있었습니다.
2021년 건국대 내시경 퀴즈에 위 결핵 증례가 있어서 아래 옮깁니다.
십이지장 제3부 만성 협착환자인데 조직검사에서 non-caseating granuloma, MTB-PCA 양성으로 나왔습니다.
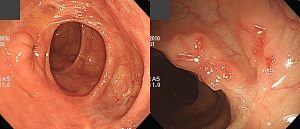
중앙대학교 병원에서 fellow 과정을 밟는 정지혜 선생님의 소개로 십이지장 결핵 증례(Clin Endosc 2014)를 보았습니다. 흑색변이 주소였던 24세 남자였습니다. 내시경 조직검사에서는 granulomatous inflammation과 necrosis 소견이었지만, QuantiFERON-TB GOLD (QFT-G; Cellestis Ltd., Carnegie, Australia) 검사가 양성이었던 점과 결핵약 투여 후 호전된 점으로 확진된 경우였습니다. 가슴 X-ray는 정상이었다고 하네요.
An ulcerohypertrophic mass is noted at the duodenal second portion below the ampulla of Vater. (Clin Endosc 2014;47:346)
(A, B) The initial scan shows an ulcerohypertrophic lesion in the duodenal second to third portion (black arrow) and mass-like, multiple perilesional enlarged lymph nodes with some necrotic changes (white arrow). (C, D) After antituberculosis treatment for 6 months, the duodenal lesion (black arrow) and multiple lymph nodes (white arrow) were decreased. (Clin Endosc 2014;47:346)
Histopathological examination shows granulomatous inflammation with necrosis. (Clin Endosc 2014;47:346)
Transparent capped endoscopy shows a scared lesion with central depression and peripheral reepithelization at 1 month after treatment. (Clin Endosc 2014;47:346)
4-1. 장결핵의 진단
장결핵의 전형적인 소견은 dirty circular ulcer입니다.
일본에서는 활동성 장결핵을 이렇게 분류하기도 합니다.
아래 인용한 아산병원의 연구에서도 transverse ulcer가 중요하다고 되어 있습니다. 그러나 저는 두 형용사 중에서 dirty가 circular보다 중요하다고 생각합니다. 물론 dirty라는 개념을 연구에 넣기는 어려웠겠지만... 여하튼 결핵은 딱 보면 지저분한 느낌입니다.
장결핵과 크론병을 구분하기 위한 메타분석도 있었습니다 (Limsrivilai J. Am J Gastroenterol 2017). 내시경 소견에 대한 부분은 다음과 같이 정리되었습니다.
"The following endoscopic findings significantly favored CD: longitudinal ulcers, aphthous ulcers, cobblestone appearance, luminal stricture, mucosal bridge, and skip lesions. Transverse ulcers and a patulous ileocecal (IC) valve significantly favored ITB. All of them were selected to build the model. Pseudopolyps did not distinguish the two diseases. Mucosal nodularity was found more often in ITB, but this was not statistically significant. For the site of involvement, rectal and sigmoid colon involvement were significant predictors of CD, while involvement of the IC valve and cecum significantly favored ITB. Involvement of rectum, sigmoid colon, and cecum were selected to build the model. Involvement of IC valve may be correlated with patulous IC valve. To avoid the possibility of including potentially interdependent variables in the model, patulous IC valve that has been reported as a significant predictor in many studies was selected. Involvement of ileum, ascending colon, transverse colon, and descending colon was not significantly different between CD and ITB. "
4-2. Intestinal Tb 가 의심될 경우 조직검사 처방
1) BL1A112A. colon 생검 1~3개 → 포르말린 통
2) BL4112. AFB stain and culture 처방 (검체 others(specify)) → saline 통
3) BG510101. Mycobacterium tuverculosis,nested PCR (검체 P17 colon) → 생검조직만
조직검사하기 전 미리 간호사에게 정보를 주어야 포르말린통에 검체가 모두 담기는 것을 막을 수 있습니다. 꼭 미리 소통하세요.
4-3. 장결핵 환자의 발열
20대 여성이 원인 미상의 발열로 내원하였습니다. 장결핵으로 진단하고 항결핵제를 투여 후 급속히 열이 없어졌습니다. 통상 2-3일 내로 현저히 체온이 떨어집니다.
4. More cases of TB colitis
우측 conjunctiva의 melanoma로 수술, 방사선 치료, 항암치료 후 interferon 치료를 받고 계신 분입니다. PET에서 상행결장의 병소가 의심되었습니다 (흰 화살표). Cecum에는 결핵성 장염의 scar가 다수 관찰되었으나 이보다 약간 원위부인 A colon에서 circumferential 방향의 얕고 지저분해보이는 궤양이 관찰되었습니다. AFB smear와 nested PCR은 음성이었으나 tissue culture에서 결핵균이 배양되었습니다. 항결핵치료 후 호전되었습니다. (EndoTODAY 목요내시경집담회 20170223)
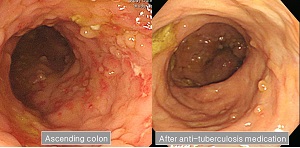
대장암 수술 후 추적 내시경 입니다. Ascending colon에서 우연히 결핵성 대장염이 발견되었습니다. 조직검사에서는 focal active colitis with focal crypt abscess 정도의 소견이었지만 tissus nested PCR 에서는 M. tuberculosis가 나왔습니다. 무증상 결핵성 대장염도 반드시 치료해야 하는가 논란이 가능하지만, 이런 경우 저는 보통 치료를 권하고 있습니다.
left: terminal ileum, right: ascending colon (EndoTODAY 목요내시경집담회 20170413)
50대 여성. A colon biopsy: Focal active inflammation with a non-caseating granuloma and lymphoid aggregates, Culture: Mycobacterium tuberculosis complex isolated
결핵성 장염의 다양한 모습 - 일본소화기내시경학회 (2017)
결핵성 장염의 다양한 모습 - 일본소화기내시경학회 (2017)
결핵성 복막염 환자의 serum CA-125는 상당히 높을 수 있습니다. 저희 병원에서 결핵성 복막염 환자 48명의 serum CA-125를 조사해 본 바 4명에서 1,000 이상이었습니다. 그 중에서 가장 높았던 경우는 CA-125가 2,702인 여성이었습니다.
결핵성 복막염 환자를 진료할 때에는 조금 이상한 기분이 듭니다. 응급실을 통하여 입원한 환자의 병실에 들어가면 거의 회진이 되지 않습니다. 환자와 가족 모두가 심하게 울고 있기 때문입니다. 초상집 분위기이지요. 난소암인데 너무 번져서 거의 손쓰기 어렵다고 들고 울고 있는 상황입니다. 결핵인데 암으로 오진한 것인지도 모르고....
제가 환자에게 몇 가지를 물어보고 (기침한 적은 없는지, 발열은 없었는지 등등) 암이 아닐 수도 있다고 하면 환자, 보호자 모두 깜짝 놀란 표정을 짓습니다. 사기꾼 보는 것과 같은 눈초리로 째래보는 분도 계셨습니다. 반대로 무슨 구세주를 만난 것 같은 기분이었다고 말한 환자도 있었습니다. 여하튼 죽을 뻔 하다가 살아난 경우입니다.
CA-125가 높다고 모두 암은 아닙니다.
지금까지 삼성서울병원에서 경험하였던 결핵성 복막염 48예를 분석하여 짧은 글로 만들어 Yonsei Medical Journal에 Clinical Significance of Serum CA-125 in Korean Females with Ascites라는 제목으로 기고하였습니다.
Purpose: Mycobacterium tuberculosis is endemic in Korea. Because tuberculous peritonitis is characterized by ascites, abdominal pain, abdominal mass and elevation of serum CA-125, it can be confused with ovarian malignancies. The aim of this study was to evaluate the significance of serum CA-125 level in the differential diagnosis of tuberculous peritonitis and ovarian malignancy in a Mycobacterium tuberculosis-endemic area.
Materials and Methods: The medical records of patients diagnosed with tuberculous peritonitis (n=48) or epithelial ovarian malignancy (n=370) at Samsung Medical Center from January 2000 to October 2009 were retrospectively reviewed.
Results: Median serum CA-125 level in the epithelial ovarian cancer group was significantly higher than that in the tuberculous peritonitis group (p≤0.01). Only one patient (2.1%) in the tuberculous peritonitis group had a serum CA-125 level over 2000 U/mL. However, 109 patients (29.5%) in the epithelial ovarian cancer group had a serum CA-125 level over 2000 U/mL. At the CA-125 ranges of 400 to 599 and 600 to 799, the proportions of those with tuberculous peritonitis were 24% and 21.9%, respectively. At a serum CA-125 level over 1000 U/mL, however, the proportion of tuberculous peritonitis was much lower (2.1%).
Conclusion: Tuberculous peritonitis should be considered in the evaluation of female patients with ascites and high serum CA-125.
혈청 CA-125의 분포입니다. 결핵성 복막염에서는 어제의 증례가 가장 높아 2,702였습니다. 그러나 1,000 이상이면 대부분 난소암이었습니다. 난소암에서 평균 CA-125치는 1,002였고 결핵성 복막염에서는 418이었습니다.
CA-125 영역별 결핵성 복막염의 분포입니다. 예를 들어서 500 정도면 약 25%는 결핵성 복막염이었습니다.
조직으로 확인된 전형적인 결핵성 복막염의 증례입니다. Fig. 5. A case of tuberculous peritonitis. (A) A 68-year old woman came to the hospital with abdominal distention which developed 2 months prior. CT scan was taken and the first impression was peritoneal carcinomatosis. (B) Laparoscopy was done and the histology showed chronic granulomatous inflammation with multinucleated giant cells. (C) No ascites were seen at the follow-up CT scan, 4 months after taking anti-Mycobacterium medication.
2개월 정도의 비특이적 상부위장관 불편감이 있던 40대 여성입니다. 내시경 검사에서 십이지장 구부의 둥근 융기부가 있고 그 중앙의 궤양이 발견되었고 같은 날 시행한 복부 초음파에서 췌장 주변의 mass가 의심되어 의뢰되었습니다. CT, PET, EUS-guided FNA 등을 시행하였습니다. CT에서는 multiple lymph adenopathy가 있고 십이지장 구부에 인접한 림프절 내부에 air가 보였습니다.
Abdominal TB lymphadenitis with fistula into the duodenal bulb로 항결핵제를 투여하였습니다. PPI가 필요한지 명확하지 않았습니다. 감염내과에서 PPI를 받아 드시고 계셨는데 중단을 권하지는 않았습니다.
 7. 결핵성 후두염. TB laryngitis with lymphadenitis
7. 결핵성 후두염. TB laryngitis with lymphadenitis
40대 남성입니다. 목이 불편하고, 덩어리지고 큰 것을 먹을 때 아프다는 증상으로 이비인후과 fellow 선생님 외래를 방문 후 조직검사가 시행되었고 다음의 소견이었습니다. "Pyriform sinus, left, punch biopsy: Chronic inflammation and inflamed granulation tissue."
이비인후과에서 시행한 CT에서는 다음과 같이 판독되었습니다.

소견: Left pyriform sinus에 2.7 cm 가량의 heterogeneously enhancing soft-tissue mass가 관찰되며 이 mass는 pyriform sinus의 apex까지 extension 되어 있음. Left neck의 IIa와 양측에 supraclavicular fossa에 multiple variable sized heterogeneously enhancing lymphadenopathy가 관찰됨.
Impression: Left pyriform sinus cancer with bilateral multiple lymph node metastases (T2 N2c)
식도 질환 유무를 확인하기 위하여 내시경 검사가 의뢰되었습니다. 식도는 정상이었고 post-cricoid area부터 left pyriform sinus media wall에 걸쳐 white plaque를 보이는 하인두 점막 염증 소견이 관찰되었습니다.
"Left pyriform sinus에 buling 및 whitish patch lesion 있어 fiberoptic guided biopsy 하였습니다. biopsy 상에서는 Chronic inflammation 소견 pending EBV 소견이나 ROF CT 상 Left pyriform sinus cancer with bilateral multiple lymph node metastases (T2N2c)" 소견으로 종양 전문 이비인후과 교수님께 의뢰된 후 수술(diagnostic laryngomicroscopic surgery with biopsy + excisional biopsy of cervical lymph node)이 시행되었습니다.
최종 병리결과는 "(1) Left pyriform sinus: Chronic inflammation, Multiple granulomas and multiple granulomatous vasculitis, (2) Lymph nodes, level III: Two reactive lymph nodes"로 나왔는데 함께 의뢰된 Tuberculosis PCR 검사에서 양성으로 나와 Tb laryngitis with lymphadenitis로 진단할 수 있었습니다. 항결핵치료 후 호전되었습니다.
[2015-12-30. 애독자 질문]
교수님, 안녕하십니까? 항상 좋은 정보, 자료와 열정에 감사드립니다. 새해에도 건승하시고 소원 성취하시기를 바랍니다. 며칠 전 애독자 증례 편지 15의 대장 결핵을 보고 문득 질문드립니다.
결핵이 의심될 때 조직검사도 하고 Tb PCR 도 보내곤 합니다만, PCR 결과가 양성으로 나오는 경우를 별로 못 본 것 같습니다. 조직검사에서 결핵이 애매모호할 때 PCR 결과에서 단서를 얻거나 진단에 도움되기를 기대하지만 그런 경우가 없어서 어째야 좋을지 의문스럽습니다. 결핵 진단에서 PCR 은 어떤 진단적 의미가 있는 것인지요? PCR 에서 도움을 얻으려면 조직을 얻을 때 특히 주의해야 할 점이 있는지도 궁금합니다.
[2015-12-30. 이준행 답변]
좋은 질문 감사합니다. 저는 장결핵 환자를 많이 보지 않습니다만, 일단 2009년 장연구학회에서 나온 장결핵 진단 가이드라인의 일부를 옮깁니다.
① 대장 점막 조직 PCR법을 이용한 결핵균의 증명은 검사의 특이도가 높은 반면 민감도가 낮아 장결핵을 크론병과 감별하는 데 결정적인 수단이 되지 못하나, 임상적으로 결핵이 의심되는 경우 보조 진단 방법으로 활용 가능성은 있다. 일반적으로 insertion element IS6110을 이용하여 PCR을 시행한다. 최초로 장결핵 진단에 대장 점막 조직 결핵균 PCR의 유용성을 알아본 연구에서는 결핵균 도말검사에서 양성인 경우 93.8%, 음성인 경우 60.0%에서 PCR 양성이라고 보고하였다. 국내 연구는 장결핵 환자 중 PCR 양성이 9.8%, 크론병이나 베체트병 환자는 PCR 양성이 0%로 비교적 낮은 양성률을 보였으며 위음성의 가능한 원인으로 반응 저해제 가능성, 결핵균의 수가 적거나 균등하게 분포되지 않아 생검 검체 내에 포함되지 않았을 가능성, 그리고 파라핀 포매 조직이므로 결핵균 DNA가 변성되거나 파괴되었을 가능성을 제시하였다. 다른 국내 연구에서는 파라핀 포매조직의 PCR 양성률 45%, 신선한 조직의 PCR 양성률 30%로 거의 차이가 없으며 충분한 양의 여러 개의 조직으로 PCR을 시행할 경우 양성률을 높이며, 육아종이 관찰되지 않는 경우에 특히 PCR이 진단 기법으로 의미가 있다고 하였다. 파라핀 포매 조직을 통상의 PCR 방법으로 할 경우 33.3%의 양성률을 보인 반면 real-time PCR 방법을 사용할 경우 66.7%의 보다 높은 양성률을 보고한 연구도 있다.
② 장결핵에서 대장 점막 조직 PCR이 위양성으로 나오는 경우는 PCR 산물의 오염 및 결핵균 DNA의 오염으로 인한 것이 대부분이고 PCR이 위음성인 경우는 가검물에 존재하는 중합효소억제인자 때문이다. 따라서 위양성 및 위음성을 낮추기 위해서는 가검물을 1% NaOH로 100도에서 2-5분간 처리하면 오염 및 억제인자를 효과적으로 제거할 수 있다.
이 분야 전문가 몇 분에게 자문한 후 다시 답변드리겠습니다.
[2015-12-30. 전문가 K 교수님 답변]
장결핵의 증상은 비특이적인 경우가 많고 심지어 아무 증상이 없이 검진 대장내시경에서 발견되기도 합니다. 비교적 흔한 증상은 점차 진행하는 설사, 복통, 체중감소 등이며, 구역감, 혈변, 발열 등을 동반하기도 합니다.
장결핵의 진단에 가장 중심적인 것은 대장내시경으로, transverse direction의 궤양, 궤양의 margin이 다소 nodular 하고 dirty한 소견을 보일 때 의심할 수 있습니다. 확진은 조직에서 caseating granuloma가 관찰되거나, AFB 양성 소견 또는 조직배양에서 M. tuberculosis가 자랄 경우 내릴 수 있으나, 아쉽게도 30% 내외입니다. 따라서 증상과 대장내시경 소견에서 장결핵이 강력히 의심될 경우, 경험적 항결핵제 치료를 통해 진단내리는 경우가 반수 이상입니다.
결핵균 PCR 검사는 결핵균에만 특이하게 존재하는 핵산(DNA)을 중합효소연쇄반응검사로 증폭하여 확인하는 분자생물학적 검사로 비교적 특이도가 높고 결과를 단시간내 얻을 수 있다는 장점이 있으나 고비용인 점, 제품마다 민감도와 특이도가 다양하다는 단점이 있어, 기존의 진단 검사를 대치할 수 없고 보조적 진단 수단으로 이용되어야 합니다.
장결핵에서 진단을 위한 결핵균 PCR 검사는 아직 데이터가 충분하지 않은 상황으로 특히 장결핵에서는 결핵균의 양이 상대적으로 작기 때문에 민감도가 낮은 단점이 있습니다. 또한 위양성을 방지하기 위해 오염 가능성을 낮추어야 합니다. 결핵균 PCR 검사는 검사 키트 제조자에 따라 나눌 수 있는데, 각 검사실에서 직접 검사를 위해 제조한 키트는 표준화가 되지 않아 진단에 사용하기에는 많은 무리가 있습니다.
사진의 증례는 장결핵의 비교적 전형적인 대장내시경 소견으로, 조직검사에서 확진되지 않더라도 경험적 항결핵제 치료를 시작해야 합니다. 결핵균 PCR 검사와 더불어 보조적 진단 기법으로 사용할 수 있는 것은 IGRA (interferon gamma release assay) test인데, 우리나라의 경우, 장결핵 환자의 약 70%에서 양성 소견을 보입니다. 하지만 IGRA test 양성이 활동성 결핵을 의미하는 바는 아닙니다.
[2015-12-30. 전문가 H 교수님 답변]
장 결핵은 조직소견/PCR/배양검사에서 진단이 안되는 경우가 많아서, 일단 임상 증상이 없거나 미미하고 내시경 육안 소견이 장 결핵에 부합되면, 육안 소견에 의존해서 진단하고 2-4개월 경험적 치료 후 호전 여부에 따라 치료 지속 여부를 결정하고 있습니다.
장결핵 환자에서 PCR 양성률을 높이는 것에 대한 제 의견을 드리자면, 결핵균은 대표적인 호기성 세균인데 산소분압이 낮고 혐기성 세균이 득세하고 있는 말단부회장/대장은 결핵균이 살기에 적합하지 않은 환경인 바, 배양검사 및 PCR 양성률이 낮은 것은 어찌보면 당연하다고 하겠습니다.
개인적인 경험에서 생검에서 육아종이 진단되는 경우도 50%를 밑도는 정도였는데, 이 또한 궤양의 크기가 작은 초기 병변에서 양성률이 높았던 듯합니다. 산소분압이 낮은 혹독한 환경에 덜 노출된 신선한(?) 병변에서 진단율이 높았던 바, PCR 양성율을 높이기 위해서도 초기 병변에서 집중적으로 생검을 하면 좋겠다는 생각입니다.
[2015-12-30. (미국 연수 중인) 전문가 H 교수님 답변]
1) 결핵 진단에서 PCR 은 어떤 진단적 의미가 있는 것인지요?
이준행 교수님께서 가이드라인을 인용하여 말씀하신 것처럼 장결핵을 진단하는데 강력한 보조적인 수단입니다 (검체 contamination이 없다면요... ) . 하지만, AFB culture +나 AFB stain + 인 경우처럼 definite diagnosis로 볼 수 없기에 empirical TB treatment 2개월 정도 후에 다시 내시경을 추적 검사하여 anti-tb 약제의 response를 확인함이 필요합니다.
2) PCR 에서 도움을 얻으려면 조직을 얻을 때 특히 주의해야 할 점이 있는지도 궁금합니다.
조직검사는 궤양 margin과 base에서 여러 조직을 얻는 것이 좋습니다. 점막에는 결핵균이 많지 않고 육아종 형성도 뚜렷하지 않기 때문에 대부분의 조직검사에서 pathognomonic finding을 주지 못하는 경우가 많습니다. 그래서 궤양의 base에서 충분한 깊이의 조직검사를 시행하는 것이 진단율을 높이는 가장 좋은 방법입니다… 하지만, mucus가 두텁게 붙어 있고 biopsy forcep이 잘 미끌어지기에 쉽지만은 않지요… 따라서, 상대적으로 조직검사가 수월한 margin에서도 충분한 깊이의 조직검사를 시행하는 것이 좋겠습니다.
결핵과 크론병의 감별은 일부 전문가는 어렵지 않다고 하지만, 쉽지 않은 경우가 종종 있습니다. 크론병을 장결핵으로 생각해서 치료가 delayed 되고 환자 compliance가 떨어지기도 하고 (일부는 결핵약 부작용에 고통받기도 하고…), 장결핵을 크론병으로 생각해 성급하게 상용한 면역억제제로 결핵의 악화가 걱정되기도 해서 임상에서는 고민되는 경우가 종종 있는 것 같습니다. 제경우에는… 조직을 이용한 AFB smear, PCR, culture 모두 진단적이지 못한 경우에는 내시경 소견, chest X ray, 임상 소견을 이용하여 잠정 진단을 내려야 하겠지만, 이련 경우 IGRA (보험은 안됩니다만)나 small bowel imaging (small bowel series, CT enterography 등)가 도움을 주는 경우가 있기에 저는 검사를 하고 있습니다. 또한, 정말 판단이 어려운 경우 환자가 증상이 없거나 경미한 경우에는 전통적인 접근으로 결핵약을 이용한 therapeutic trial을 선호합니다.
[2016-1-2. 애독자 의견]
장결핵에 대한 애독자 의견과 전문가 답변 중 "결핵균은 대표적인 호기성 세균인데 산소분압이 낮고 혐기성 세균이 득세하고 있는 말단부회장/대장은 결핵균이 살기에 적합하지 않은 환경인 바" 부분은 말단부회장 주변이 IC valve 에 의해 대변이 머물면서 가장 결핵균에 오래 노출되고 따라서 가장 장결핵 병변이 빈발하는 부분인데 자칫 해당 부위에 장결핵이 드물다는 뜻으로 오해할 수 있을 것 같습니다. 지난 애독자 질문 중에 장결핵이 왜 말단회장 주변에 호발하냐는 질문도 있었기에 한 번 짚어주시면 더 좋을 것 같습니다.
[2016-1-2. 애독자 의견]
보내주신 내용(장결핵에 대한 애독자 의견과 전문가 답변)을 읽고 제 경우에 의외로 tuberculin test가 큰 도움이 되었기에 말씀드립니다. 어렸을 때 결핵예방주사를 맞았다고 하더라도, 대부분의 성인은 tuberculin test 검사시 강한 양성 반응을 보이지 않는다는 사실을 지난 10년간의 경험을 통해 터득했기에 말씀드립니다.
저는 대장내시경 소견과 조직검사 결과가 의심될 경우, 외래에서 tuberculin test를 시행해서 강한 양성을 보이면 HREZ regimen을 시작합니다. 반대로 tuberculin test가 음성이면 mesalazine 1g tid po만 처방합니다. 제가 운이 좋은 건지 몰라도 지금까지 위 방법으로 약물투여를 하며 추적대장내시경 검사를 한 결과, tuberculin test 후에 내린 진단명은 모두 적중하였습니다. 그래서 제 외래에는 완치된 Tbc colitis 환자들과 장기간 추적 중인 Crohn's disease 환자들 수가 매년 누적되고 있습니다. 위 외과 교수님께도 tuberculin test를 적극 활용하실 것을 추천해드리고 싶습니다.
[2016-1-4. 이준행 의견]
Tuberculin test는 좋은 아이디어입니다. 이 이슈에 대한 좋은 국내자료를 보지 못한 것 같고 2009년 가이드라인에는 아직 아래와 같이 언급되고 있을 뿐이지만, 연구해 볼 가치가 있는 좋은 이슈라고 생각합니다. 장결핵과 다른 염증성 장질환을 감별진단하는 데 있어 TST의 유용성에 대한 좋은 연구 결과는 현재 없는 실정이다. 특히 결핵 감염률이 높은 지역에서는 BCG와의 교차 반응과 결핵균의 잠복 감염으로 TST가 양성으로 나올 가능성이 있어 TST 양성 결과를 판독하는 데 어려움이 있다
[2016-1-6. 애독자 KTK 의견]
교수님 좋은 말씀 감사합니다. 제가 들은 이야기를 조금 덧붙이고 싶어 글을 보냅니다. TST 검사가 좋은 검사이지만 요즘 시약을 구하기 어려워 시행해 보기 어려운 점이 있습니다. 결핵 접촉 환자에서 TST 검사를 시행해 보려고 했을 때 시약이 없어 시행하지 못한 경험이 있습니다. 제가 듣기로는 외국에서 이 시약을 충분히 생산하지 않아 국가적으로도 구하기 어렵다고 하네요...
[2020-4-14. 이준행]
병원 식당에 영상의학과제퀴즈몰이 있습니다. 상당히 어려운 문제가 많은데요... 이번 문제는 특히 어려웠던 모양입니다. Adrenal tuberculosis.
1) 장결핵 진단 가이드라인 대한소화기학회지 2009. PDF 0.7M
2) Differentiation of tuberculous peritonitis from peritonitis carcinomatosa without surgical intervention - Turkey 의사들이 Saudi Arabia의 저널에 실은 내용인데 매우 clear한 결론입니다. 초록 일부를 옮깁니다.
In univariate analysis; fever, night sweats, and abdominal pain were significantly more frequent in the TBP group compared to those in the Ov Ca group (P < 0.001, P < 0.001, and P = 0.035, respectively) and the Ga Ca group (P < 0.001, P < 0.001, and P = 0.015, respectively). Serum CA 19-9 and carcino embryonic antigen (CEA) levels were significantly lower in the TBP and Ov Ca group compared to the Ga Ca group (P < 0.001 and P < 0.001, respectively). Elevated serum CA 125 level was found in all patients with TBP and Ov Ca and in 86.6% of patients with Ga Ca. In the multivariate analysis, presence of fever (P < 0.001), night sweats (P < 0.001), age under 40 years (P = 0.008), and normal serum CA 19-9 level (P = 0.044) were independent predictor of diagnosis of tuberculous peritonitis.
5) Etiologic and laboratory analyses of ascites in patients who underwent diagnostic paracentesis
6) Clinical significance of serum CA 125 in patients with chronic liver diseases
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.