 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [EndoManual. Quick reference - Endoscopy protocol at SMC] - 終
[EndoManual. Quick reference - Endoscopy protocol at SMC] - 終
1. Basic 기본
2. Esophagus 식도
3. Stomach 위 - 조직검사, 내시경치료 후 추적검사, Helicobacter, Clipping
4. Duodenum 십이지장
6. Others 기타
다음의 순서로 기술하세요. 한글과 영문을 혼용해도 좋습니다. 자신에서 편한 방법으로 쓰기 바랍니다.
(1) 위치
(2) 크기
(3) 주소견 (mass인지, superficial lesion인지, ulcerative lesion인지 등)
(4) 부소견 - 적절한 용어를 사용하여 상세히 기술해 주세요.
(5) 진단 (impression)
(6) 분류
* SMC style로 내시경 소견을 기술하는 방법을 보다 깊게 배우고 싶으신 분에게는 description exercise workshop (DEX)을 권합니다.
* 참고: EndoTODAY 내시경 배우기 초심자 교실 DEX
* 참고: EndoTODAY 내시경 사진 촬영법
 식도암/식도이형성 내시경 치료 후 추적 조직검사 가이드
식도암/식도이형성 내시경 치료 후 추적 조직검사 가이드
"식도암 ESD 후 추적 내시경 검사에서 시술 후 기간과 상관없이 ESD scar에 육안적 이상소견이 없을 경우 루틴 조직검사는 시행하지 않는다. 사진을 잘 남긴다. 추가로 ESD site 외 식도 다른 부위에 대한 세심한 관찰은 필요하다"
1) 1 cm 미만의 바렛식도가 의심되면 사진을 잘 찍어두고 결과지에 언급하지 않는다. 임상적 의의가 없는 소견으로 간주한다.
2) 1 cm - 3 cm의 바렛식도가 의심되면 사진을 잘 찍어두고 조직검사를 2개 정도 시행하고 결과지에 r/o short segment Barrett's esophagus로 쓴다.
3) 3 cm 이상의 바렛식도가 의심되면 사진을 잘 찍어두고 조직검사를 2(4)개 정도 시행하고 결과지에 r/o long segment Barrett's esophagus로 쓴다.
4) Dysplasia가 있거나 의심되면 전문가에게 의뢰한다.
5) Dysplasia가 없으면 1년 후 추적내시경 검사를 시행한다. 추적내시경에서 자세히 관찰하여 특별히 의심되는 곳이 없으면 조직검사를 하지 않아도 좋다.
* 참고: EndoTODAY 바렛 식도
식도암 RT 전 clipping을 요청받으면 위암과 비슷하게 병소 경계 1cm 지점에 클립을 2개씩 위치시킵니다. Proximal margin보다 1 cm proximal에 두 개, distal margin보다 1 cm distal에 두 개.
식도암 proximal margin보다 1cm 상방과 distal margin보다 1cm 하방에 각각 clip을 두개씩 apply하였고 직후에 RT를 위한 simulation CT를 찍어서 치료 범위를 결정하였습니다.
내시경 추정진단에 따라 몇 개의 조직검체를 얻어야 좋을지 정해진 규칙은 없습니다. 저는 개인적으로 양성위궤양, 조기위암에서는 3개 정도, 진행성 위암에서는 6-8개 정도, SMT에서는 2개 정도의 조직검사를 해 주십시오. 조기위암에서 너무 많은 조직검사를 하면 내시경 치료에 방해가 될 수 있습니다. 진행성 위암은 조직 괴사가 심한 경우가 있으므로 상대적으로 많은 수의 조직 검체가 필요합니다.
최근 진행성 위암은 여러 marker의 개발로 과거보다 조직검사가 더 많이 필요합니다. 최소한 6개, 가능하면 8개의 조직검사를 부탁합니다.
CAP and NCCN Guidelines recommendations state that, when possible, a minimum of 5 biopsy specimens and optimally, 6 to 8, should be obtained to account for intratumoral heterogeneity of HER2 in GEA and to provide sufficient tumor specimens for diagnosis and biomarker testing. (Arch Pathol Lab Med 2016)
위암 환자에서 몇 가지 marker 검사는 환자의 진단과 치료에 크게 도움이 됩니다. HER-2 (처방코드 BP3A12), MLH1 (처방코드 BP3C25), PD-L1 28-8 (처방코드 BP3E06) 등인데요 과거에는 내시경실에서 처방을 하였으나 2024년 6월 19일부터는 병리과에서 H&E 슬라이드를 확인한 후 필요한 추가 검사를 처방하여 시행하기로 하였습니다. 내시경실에서는 위암 환자에서 HER-2, MLH1, PD-L1 28-8 등의 처방은 하지 말아주시기 바랍니다.
* 참고: EndoTODAY 조직검사
* 참고: EndoTODAY 위암 11
조기위암이나 선종 내시경 절제술 후 의미있는 재발은 육안소견에 이상이 있을 때 발견됩니다. 육안소견에서 재발이 의심되지 않았으나 조직검사에서 재발로 나오는 경우는 매우 적습니다. 따라서 조직검사를 많이 하기보다는 적게 하는 것이 좋습니다. 아래 참조.
1) 조기위암 EMR/ESD: 2년까지 추적 내시경마다 scar에서 조직검사 (1-2점) → 2년 후부터는 재발 의심 소견이 있을 때만 조직검사 (단, 조기위암 EMR/ESD 후 첫 추적 내시경에서는 antrum GC와 midbody GC에서 각각 조직검사를 하여 Giemsa staining을 의뢰한다.)
2) 선종이나 위신경내분비종양 EMR/ESD: 시술 후 첫 추적 내시경에서는 scar에서 조직검사 (1-2점) → 이후에는 재발 의심 소견이 있을 때만 조직검사 (단, 선종 EMR/ESD 후 antrum GC와 midbody GC에서 각각 조직검사를 하여 Giemsa staining을 의뢰한다.)
3) 선종 APC: 재발 의심 소견이 있을 때만 조직검사
* 참고: EndoTODAY ESD 후 내시경 소견
 [Helicobacter] Giemsa staining을 위한 헬리코박터 조직검사 위치
[Helicobacter] Giemsa staining을 위한 헬리코박터 조직검사 위치
위전정부 대만 혹은 소만에서 1점 + 위체중부 대만에서 1점.
한 곳에서만 조직을 얻을 경우는 위체중부 대만에서 1점을 채취합니다.
 위염 내시경 분류 - 이준행의 위염 내시경 분류 (last update: 2017-4-20)
위염 내시경 분류 - 이준행의 위염 내시경 분류 (last update: 2017-4-20)
위염의 내시경 분류법은 Schindler 법, Sydney 법 그리고 일본 위염 분류 등이 있습니다. 어느 하나 우리나라 현실에 맞지 않습니다. 우리 고유의 분류법이 필요한데 아직 이 분야에 대한 논의는 부족합니다. 결국 제 스타일로 스스로 만들어 쓰는 수밖에 없었습니다. '이준행 위염 내시경 분류'를 생각해봅니다.
1) '비특이적 위염 (nonspecific gastritis)'은 가장 현저한 소견을 바탕으로 진단명을 쓴다. 부족하다고 느껴지는 경우에는 딱 한 가지 진단명을 덧붙인다. 예를 들면 '만성 위축성 위염'인데 화생성 변화도 무시하기 어려운 정도라면 '만성 위축성 화생성 위염 (chronic atrophic (and) metaplastic gastritis)'이라고 쓴다.
| 내시경 소견 | 내시경 진단 |
| Erythema (hyperemia) | Chronic superficial gastritis |
| Erosions (flat or raised) | Chronic erosive gastritis |
| Atrophic changes | Chronic atrophic gastritis |
| Metaplastic changes | Chronic metaplastic gastritis |
| Hypertrophic changes | Chronic hypertrophic gastritis |
| Hematins | Chronic superficial gastritis |
2) '특이적 위염 (specific gastritis)'은 각자의 기술법에 따른다.
3) Single erosion은 암을 배제해야 하기 때문에 따로 관리한다.
4) 기타
- 쓰지 말아야 할 진단명: 출혈성 위염, 담즙 역류성 위염
- 염증 소견이 거의 없는 경우 '정상'이라는 진단을 붙인다.
* 참고: EndoTODAY 위염
 위궤양 - 십이지장 궤양은 아래를 참고하십시오.
위궤양 - 십이지장 궤양은 아래를 참고하십시오.
처음 발견한 active/healing stage gastric ulcer: 조직검사 3개 + 헬리코박터 Giemsa 조직검사 (전정부 1개 + 위체부 1개)
처음 발견한 scar stage gastric ulcer: 조직검사 3개 + 헬리코박터 Giemsa 조직검사 (전정부 1개 + 위체부 1개)
Active/healing stage gastric ulcer의 첫 추적 내시경에서 보이는 ulcer scar: 조직검사 3개 + 헬리코박터 Giemsa 조직검사 (전정부 1개 + 위체부 1개)
- 참고 1: UBT 처방이 있더라도 헬리코박터 조직검사는 해 주세요. Dual check 개념입니다.
- 참고 2: 최초 검사에서 헬리코박터 음성이었더라도 첫 추적 내시경에서는 헬리코박터 조직검사를 해 주세요. 최초 검사의 false positive를 고려해야 합니다.
- 참고 3: ESD 후 Hp 제균치료를 한 환자의 추적 내시경에서는 헬리코박터 조직검사는 필요하지 않습니다. ESD 후 Hp 제균치료 결과 판정은 UBT로 합니다.
- 참고 4: 소화성 궤양이 없었고 단지 Hp 위염때문에 선별급여 100/100으로 Hp 제균치료를 한 환자의 추적 내시경에서는 헬리코박터 조직검사는 필요하지 않습니다. Hp 위염 선별급여 100/100 제균치료 결과 판정은 UBT로 합니다.
궤양 치료 1년 후 추적 내시경: 조직검사 3개 (헬리코박터 검사는 필요하지 않습니다)
궤양 치료 2년 후 추적 내시경: 특이 소견 없는 평범한 궤양 반흔이라면 조직검사, 헬리코박터 검사 모두 필요하지 않습니다.
* 참고: EndoTODAY 소화성궤양
* 참고: FAQ 위궤양에서 Helicobacter 제균치료 후 추적검사
출혈성 궤양의 Forrest 분류
 AGML (acute gastric mucosal lesion)
AGML (acute gastric mucosal lesion)
내시경실에서 AGML을 만나면 가장 심한 곳에서 조직검사를 3점 정도 시행합시다 (H&E 염색). Helicobacter pylori 검사는 필요하지 않습니다.
어떤 수술을 예정하고 있는가에 따라 수술 방법이 달라집니다.
[1. Distal gastrectomy]
위암병소가 위체중부에 있을 때에는 subtotal gastrectomy의 절제면을 정하기 어렵기 때문에, 수술 전 내시경 클리핑이 필요합니다. 병소의 proximal edge 보다 1 cm 상방에 2개의 클립을 나란히 붙여서 위치시키는 방법을 권합니다. 이렇게 하였을 때 수술장에서 가장 잘 만져진다고 합니다.
[2. Proximal gastrectomy]
Cardia 직하부 위암에 대한 proximal gastrectomy를 위하여 clipping을 할 때에는 원위부에 두 개의 clipping을 합니다. 그러나 근위부에도 두 개의 clipping을 해 두면 근위부 절제변연을 정하는데도 도움이 됩니다.
아래는 fundus neuroendocrine tumor (조직검사에서 endolymphatic tumor emboli가 있었음)에 대한 proximal gastrectomy 전 clipping 시행한 증례입니다.
[3. Pylorus preserving gastrectomy (PPG)]
Pylorus preserving gastrectomy (PPG) 전에는 proximal과 distal 양 방향에 두 개씩 clipping이 필요합니다.
 위암 수술 후 내시경에서 음식물이 남음 (subtotal gastrectomy)
위암 수술 후 내시경에서 음식물이 남음 (subtotal gastrectomy)
1) 위암 수술 후 잔위에는 충분한 금식 후에도 약간의 음식이 남아있게 되는데 이는 비정상 소견이라기 보다는 정상 수술 후 소견이라고 할 수 있습니다.
2) 비록 어느 정도의 음식이 남아있다고 하더라고 문합부를 충분히 관찰할 수 있는 경우는 검사를 실행한 것으로 하고 결과를 입력해 주십시오 .
3) 음식물이 남아있는 경우 음식물 때문에 완전한 검사가 되지 못했음을 명기해 주십시오.
4) 해당과의 요구가 있을 경우 다시 검사를 시행할 수 있습니다.
* 참고: EndoTODAY 위암 수술 후 내시경 소견
 상부위장관 점막하종양 (SMT, submucosal tumor; SET, subepithelial tumor)
상부위장관 점막하종양 (SMT, submucosal tumor; SET, subepithelial tumor)
작은 SMT/SET에 대한 조직검사는 너무 자주 시행되고 있습니다. 육안 소견이 나쁘지 않으면 0.5-1cm 이하의 SMT/SET에 대해서는 조직검사를 하지 않아도 좋습니다. 조금이라도 varix가 의심되거나 cystic structure에서는 조직검사를 하지 맙시다. 0.5cm 이하의 tiny SMT가 의심되는 정도일 때에는 내시경 결과지에 그 내용을 기술하지 않아도 좋습니다.
1) 첫 내시경 검사에서는 조직검사를 2조각 시행해 주세요. 다만 1-2 cm 미만의 표면이 정상인 점막하종양 의심병소가 fundus, cardia, high body에 위치하면 조직검사를 하지 않아도 좋습니다. 조금이라도 vascular structure나 cyst가 의심되면 조직검사를 하면 안됩니다.
SMT 의심병소 조직검사 후 귀가 전 대량출혈을 보였던 증례. 이 부위는 생각보다 vascular origin이 많으므로 극히 주의해야 합니다. SMT 같은데 조직검사를 하여 중요한 진단을 붙인 경우는 생각보다 많지 않습니다.
vascular 하거나 cystic하면 조직검사를 하지 말라는 유명한 editorial (Eckardt. GIE 2005;62:209-212)
2) 추적 내시경 검사에서 크기나 모양의 변화가 없으면 조직검사는 필요하지 않습니다.
* 참고: EndoTODAY 위점막하종양
1) Initial 내시경: 병소에서 조직검사 2개 (Multiple이면 가장 대표적인 병소 2-3곳에서 2개씩 조직검사) + 헬리코박터 Giemsa staining 검사 (전정부 + 위체부)
2) 제균치료 후 첫 추적 내시경: 병소에서 조직검사 2개 (Multiple이면 가장 대표적인 병소 2-3곳에서 2개씩 조직검사) + 헬리코박터 Giemsa staining 검사 (전정부 + 위체부)
* UBT 처방이 있어도 헬리코박터 Giemsa staining 검사 (전정부 + 위체부)는 시행.3) 헬리코박터가 성공적으로 제균된 것이 확인된 이후의 추적 내시경: 병소에서 조직검사 2개 (Multiple이면 가장 대표적인 병소 2-3곳에서 2개씩 조직검사). 육안적으로 다 좋아졌으면 가장 현저했던 곳 1-2곳에서 2개씩.
* 헬리코박터 Giemsa staining 검사를 반복할 필요는 없습니다.
Hp 음성 MALT 림프종 환자로 RT 후 호전된 환자입니다.
그런데 추적내시경 검사의 결과가 MALToma로만 되어 있습니다. 결과만 보면 "재발인가?" 의심할 수 있습니다. MALT 림프종이었으나 치료 후 호전된 환자의 내시경을 할 때에는 'Remission after treatment for MALToma' 혹은 'MALToma in remission'으로 impression을 붙여주시기 바랍니다.
* 참고: EndoTODAY 위 MALToma
[십이지장궤양]
처음 발견한 active/healing stage duodenal ulcer: 헬리코박터 조직검사 (전정부 1개 + 위체부 1개) + 십이지장 조직검사는 optional (보통은 하지 않습니다만, 조금이라도 악성질환이 의심되면 2-3개 해 주세요.)
처음 발견한 scar stage duodenal ulcer: 헬리코박터 조직검사 (전정부 1개 + 위체부 1개). 십이지장 조직검사는 필요하지 않습니다.
제균치료 1년 혹은 그 이후 추적 내시경에서 궤양 재발의 증거가 없으면 십이지장 조직검사나 헬리코박터 조직검사는 필요하지 않습니다.
 대장내시경 +/- 용종절제술' 전 anti-thrombotics 중단
대장내시경 +/- 용종절제술' 전 anti-thrombotics 중단
대략적이고 일반적인 프로토콜입니다. 개별 환자에서는 담당 의사의 판단에 따라 적절히 조절해서 적용해 주시기 바랍니다.
임상강사 선생님들께. 대장내시경 시 항혈전제 사용 중단 안에 대하여 최근 논의가 있었습니다. 보내드리는 프로토콜과 같이 심장질환, 뇌혈관질환의 고위험군이거나 아스피린을 제외한 항혈소판 (clopidogrel, ticagrelor, prasugrel...), 항응고제 (warfarin, NOAC....) 에 대해서는 기존에 해오던 것처럼 해당과 협진 의견을 따르기로 하였고, 대장내시경을 받게되는 저위험군 환자들은 아스피린을 중단하지 않아도 대장내시경 with 용종절제술 (단 1cm 미만의 용종)은 가능하다로 수정하였습니다. 만약 저위험군 환자에 대하여 의사가 판단하여 아스피린을 끊고자 한다면 4일 중단을 권유하기로 하였습니다. 항혈전제 재시작은 프로토콜을 참조하시기 바랍니다. 감사합니다. 2017-3-28. 소화기내과 김태준
대부분의 병동 환자에서 내장내시경 전처치는 외래와 동일하게 Clicool 3L 를 처방합니다. 단, CRF나 ESRD 환자에서는 Colonlyte 4L를 복용하도록 합니다.
Clicool 3L 복용 후 장정결이 좋지 않은 경우에는 Colyte-F 2L를 추가복용합니다.
평소 변비가 심한 환자에서는 검사 전일 저녁에 장정결제와 더불어 bisacodyl 좌약을 삽입해도 좋습니다.
* 참고: EndoTODAY 장정결
 직장경(sigmoidoscopy)에서 대변이 남아 있음
직장경(sigmoidoscopy)에서 대변이 남아 있음
Sigmoidoscopy는 대장내시경보다 약간 대장정결제를 투여하고 시행하는 검사입니다. 따라서 대변이 남아있는 경우가 많습니다. 내시경실에서는 조금 대변이 남아있다는 이유로 Yal enema를 여러번 반복한 후 검사하기도 합니다. 그러나 Yal을 쓰더라도 완전히 깨끗해지는 않는 경우도 많습니다.
Sigmoidoscopy는 특별한 목적이 있어서 시행하는 검사입니다. 비록 약간의 변이 남아있더라도 검사의 목적을 달성하였다면 Yal enema를 반복하지 않는 것이 좋습니다. 아래 환자는 전립선암으로 수술 및 RT 후 radiation proctitis 여부를 보기 위한 검사였습니다. 이 정도 변이 남아 있더라도 검사 목적은 달성한 것입니다. 'Radiation proctitis 없음' 정도의 결론으로 검사를 마쳐도 무난할 것 같습니다.
* 참고: EndoTODAY 대장내시경 삽입법
 대장내시경에서 cecal intubation이 되지 않은 경우 혹은 rectum에 병소가 있고 더 이상 검사하지 못한 경우 등
대장내시경에서 cecal intubation이 되지 않은 경우 혹은 rectum에 병소가 있고 더 이상 검사하지 못한 경우 등
Colonoscopy를 시도하였으나 cecal intubation이 되지 않은 경우가 있습니다. (1) 대장 loop 등으로 끝까지 삽입되지 못한 경우, (2) 중간에 obstruction을 보이는 병소가 있어 더 이상 진행하지 못한 경우, (3) 중간에 검사의 목적에 해당하는 병소가 발견되어 더 이상 검사할 필요가 없었던 경우 등이 있습니다. 이런 경우 간혹 처방을 sigmoidoscopy로 변경하시는 분이 계시는데 바람직하지 않습니다. 그냥 colonoscopy를 시행한 것으로 기록을 남겨주시기 바랍니다. Cecum까지 보지 못한 이유를 남기면 그만입니다. Sigmoidoscopy로 바꿔 처방하지 마십시오.
Colonoscopy와 sigmoidoscopy는 검사의 목적, 전처치, 시술 후 조치 등이 전혀 다른 검사입니다. 깊게 보지 못하였다는 혹은 깊게 보지 않았다는 이유로 처방을 변경하면 내시경 시술 전후 여러가지가 이상하게 꼬입니다. 환자에게 금전적 이익도 별로 크지 않습니다. 아주 작은 금전적 이익이 있을지 모르겠으나, 치료과정에 큰 혼선과 위험이 발생한다는 것을 생각하면 처방을 바꾸는 것은 환자에게 해가 되는 일일 수도 있습니다.
Colonoscopy를 sigmoidoscopy로 처방변경하는 것을 금합니다.
* 참고: EndoTODAY 대장내시경 삽입법
 Ulcerative colitis 진단과 모니터링을 위한 조직검사 protocol
Ulcerative colitis 진단과 모니터링을 위한 조직검사 protocol
3 mm 이하는 cold biopsy로 제거할 수 있으나 이보다 크면 cold biopsy로 제거한 후 residual tumor가 많이 남습니다.
4-7 mm 는 cold snaring으로 제거할 수 있습니다. Snare로 제거하면 snare polypectomy로 처방할 수 있습니다. Cold snaring 할 때에는 tenting을 하지 않아야 합니다.
LST가 발견되고 one stage로 제거하기 어려운 상황이면 조직검사를 1-2점만 하고 submucosal injection을 하지 말아야 합니다. 조직검사를 하지 않고 사진만 잘 찍어두고 교수님께 의뢰해도 됩니다.
* 참고: EndoTODAY LST 조직검사
용종절제술 후 예방적 clipping의 효과는 입증되어 있지 않습니다. 극히 예외적인 경우(active bleeding이 조절되지 않을 때, exposed vessel이 보일 때 등)를 제외하면 예방적 clipping은 필요하지는 않습니다.
1) Indocyanine green
- The stock solution of ICG was prepared by dissolving 25 mg of powdered ICG in 2 ml of the solvent (sterilized water) provided by the manufacturer.
- For each injection, 1 ml of the suspension was used.2) Guideline
- 수술 예정 1주 안에 시행
- 병변과 1 cm 떨어져서 2곳에 충분한 양을 주사한다. 먼저 saline 주사로 bleb을 만들고 각 bleb에 ICG 용액 1cc씩 주사한다. 시술을 마친 후 사진을 남긴다.
- 병소가 작으면 병소 옆에 주사하고 병소가 크면 병소 distal에 주사한다.3) Technique
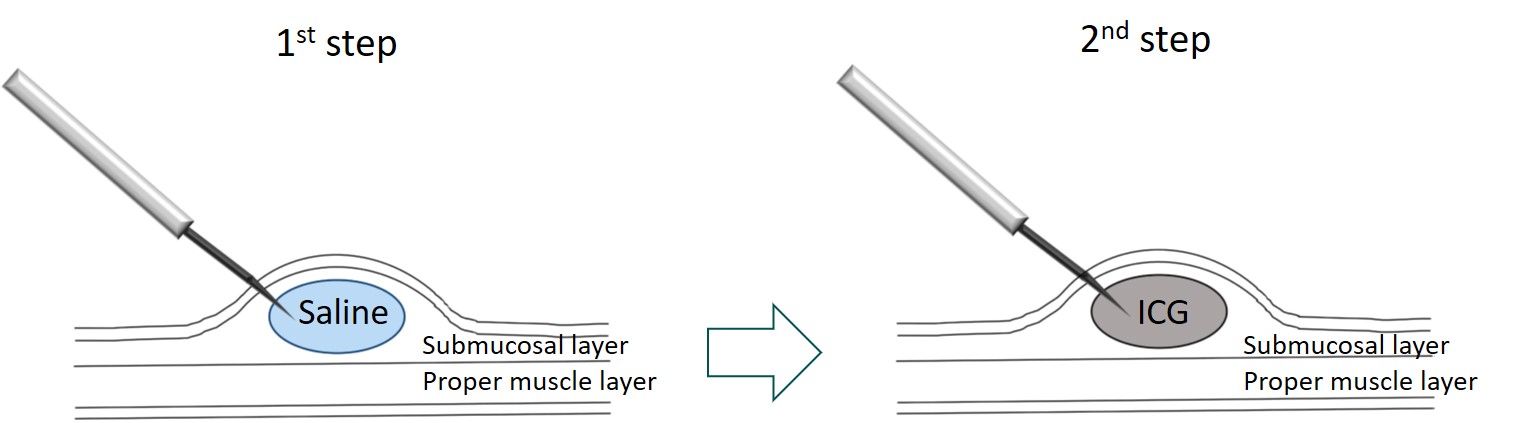
- The needle should be inserted at an oblique angle to the bowel wall to avoid penetrating the serosa.
- 2 ml of normal saline solution was injected tangentially into the submucosal layer to form a submucosal elevation.
- Then the syringe used for the saline solution was replaced by another syringe containing ICG, and 0.5-1.0 cc per injection was injected. Subsequently, the ICG syringe was replaced by the first syringe of saline, and about 2 ml of the saline solution was added to push out the ICG remaining in the needle device4) Caution
ICG cannot be used in patients with allergy to iodine.5) Complication
- preoperative adverse reactions : fever, abdominal pain, or allergy symptoms
- during surgery : focal peritonitis, inflammatory pseudotumor, abscess, or adhesion
- postoperative complications : adhesion, ileus
 장결핵 (Intestinal tuberculosis)이 의심될 경우 조직검사 처방
장결핵 (Intestinal tuberculosis)이 의심될 경우 조직검사 처방
1) 일반 조직검사 하듯이 colon 생검 1~3개. 구조화폼 이용 → 포르말린 통
2) MTB/PCR 처방 (BP8109). 구조화폼 이용. 처방창에 tuberculosis를 typing 하면 Mycobacterium tuberculosis, tissue [Real-time PCR]이 나옵니다. → 검체는
conical tube에 넣어주세요.
3) AFB stain and culture 처방 (BL4112). 다윈 구조화폼이 아니라 일반 처방창에서 AFB 1st 입력 → 검체는
conical tube에 넣어주세요.
* 참고: 조직검사 하기 전 미리 간호사에게 정보를 줘야 포르말린통에 검체가 모두 담기는 것을 막을 수 있습니다. 꼭 미리 소통하세요.
* 참고: EndoTODAY 결핵성 위장질환
Q: 복부 수술 후 screening colonoscopy를 원하는 환자에게 언제 검사를 하도록 권해야 할까요?
A: 환자의 상태에 따라, 수술의 종류에 따라 변수가 많습니다. 혈변이나 복통 등 증상 평가를 위한 대장내시경은 대부분의 경우 수술 직후라도 시행할 수 있습니다. 그러나 무증상 성인의 screening colonoscopy는 수술 6개월 이후에 받도록 권하는 것이 안전할 것 같습니다.
[내시경 검사를 하지 못한 경우의 기록]
위내시경이나 대장내시경을 시작하였는데 통상적인 방법으로 전부 관찰하지 못했더라도 내시경 검사를 실시한 것으로 해 주세요. Loop가 심하여 A colon을 관찰하지 못했더라도 대장내시경 검사는 한 것으로 해 주시고("실시"), 결과에 다 보지 못했다는 점을 명확히 써 주시면 됩니다 ("incomplete observation"). S colon에서 암을 발견하고 협착으로 인하여 그보다 상방을 관찰하지 못했다는 이유로 sigmoidoscopy로 변경하지 말기 바랍니다. 이 경우도 대장내시경 검사는 한 것이고("실시"), S colon의 암을 발견한 중요한 성과가 있는 것입니다. 처방 변경은 가급적 하지 않는 것이 좋습니다.
물론 아주 드문 예외 상황이 있습니다. 예를 들어 bowel preparation이 너무 안 좋아서 아예 안 하느니만 못한 경우입니다. 위에 음식이 너무 많아서 검사를 못한 경우도 마찬가지입니다. 이런 상황에서 검사를 한 것으로 실시할 수 없습니다 ("fail 처리"). 의무기록은 꼭 남기셔야 합니다. 그리고 가급적 사진은 남기시기 바랍니다.
검사가 fail한 경우 의무기록은 '외래 서식'을 열어 기록을 남길 것을 권합니다. 비록 진짜 외래 진료를 본 것은 아니므로 실시는 할 수 없고 임시 저장밖에 못하지만 현재로서는 그것이 최선입니다. 더 좋은 기록 방법을 만들어 보겠습니다만, 당분간은 '외래 서식'에 기록을 남기시기 바랍니다.
신경과, 재활의학과, 이비인후과 등에서 PEG 의뢰가 온 경우에는 PEG에 대한 contraindication이 없으면 가급적 PEG를 시행하는 것이 좋습니다. PEG를 꼭 필요한 경우로 한정하는 것은 여러 진료과와 갈등을 빚을 뿐입니다. 내과 의사의 입장에서 definite contraindication이 있으면 의뢰하신 의료진에게 명확히 설명하고 PEG를 시행하지 않으면 됩니다. 유연하게 대응합시다.
* 참고: EndoTODAY PEG
수거한 기생충은 올바른 수액을 담은 적당한 크기의 통에 넣어서 기생충학교실이나 미생물검사실로 보내야 합니다. 보통 생리식염수가 가장 좋습니다. 포도당이나 증류수에 기생충을 넣으면 삼투압때문에 더 이상의 검사를 못할 수 있습니다. (병원에 따라 포르말린 통에 넣어달라는 곳도 있습니다.) 미리 기생충 검사실 전화번호와 검사코드를 알아두면 막상 환자를 만났을 때 당황하지 않을 수 있습니다.
* 참고: EndoTODAY 기생충학
 병동환자 내시경 시 보호자 동반 여부 (업무연락. 2017-4-21. 내시경실장 이준행)
병동환자 내시경 시 보호자 동반 여부 (업무연락. 2017-4-21. 내시경실장 이준행)
1) 진단 위장내시경: 진정(수면) 여부와 무관하게 보호자 없이 가능하나 환자 상태가 안정적이지 않을 경우는 병동에서 진료과 자체 판단으로 보호자가 동반하도록 조처해 주기 바랍니다.
2) 치료내시경: 진정(수면) 여부와 무관하게 보호자 필요하나, 급한 경우는 보호자의 유선연락처 확보 후 시술 가능합니다.
3) 췌담도 내시경: 진정(수면) 여부와 무관하게 보호자 필요하나 급한 경우는 보호자의 유선연락처 확보 후 시술 가능합니다.
[2016-3-26. 이준행 편지]
내시경 상황별 메뉴얼이라는 도저히 불가능해 보이는 일에 도전합니다. 환자마다 다르고 검사자마다 다른데 어떻게 제가 감히 표준 메뉴얼을 만들 수 있겠습니까? 한 병원에서도 의사마다 생각이 다른 부분도 많습니다. 결국 환자 상태를 고려하여 검사자가 그 순간 최선의 판단을 하면 그만이겠지요. 정답이란 없는 영역이니까...
그러나 내시경 경험이 짧은 검사자에게는 다양한 상황에서 참고할 수 있는 무난한 메뉴얼이 있다면 판단 혹은 애드립이 쉬워질 것 같습니다. Quick reference라고나 할까요...
전적으로 개인적 의견입니다. 병원의 공식 입장 아닙니다. 여하튼 좀 더 다듬어보려고 하오니 여러분의 많은 피드백 부탁합니다.
[2016-3-28. 애독자 편지]
안녕하십니까 처음 메일 드립니다. 경남의 검진센터에 있는 모 소화기내과 의사입니다. 작년 펠로우 기간부터 메일을 수신받기 시작하여 가끔씩 읽어나가다가 올해 로컬로 나오면서 매일매일 메일을 읽어보기 시작하였습니다. 금일 이 내용은 정말 유익하고 특히 펠로우 선생님들께 도움될 것 같아서 제가 후배님들한테 전파하였습니다. 교수님 입장에서는 당연한 것으로 생각되지만 그동안 헷갈리고 애매했던 것들 시원하게 정해주셔서 감사합니다. 참조하여 잘 검사하도록 하겠습니다. 항상 건강하십시오.^^
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.